Abstract
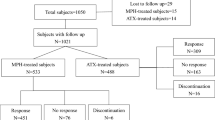
Atomoxetine is a noradrenergic reuptake inhibitor prescribed for attention-deficit/hyperactivity disorder (ADHD) that first gained approval in the USA in 2002 and has been authorized in 97 countries worldwide. The aim of this paper is to comprehensively review publications that addressed one or more of seven major safety topics relevant to atomoxetine treatment of children and adolescents (aged ≥6 years) diagnosed with ADHD. While the review focuses on children and adolescents, publications in which data from patients aged >18 years and from 6 to 18 years were analyzed in the same dataset were included. Using a predefined search strategy, including agreement of two reviewers when selecting papers, reduced the potential for bias. Using this process, we identified 70 eligible papers (clinical trials, epidemiological studies, and case reports) across the seven topics. We also referred to the European Summary of Product Characteristics (SPC) and US label. We found 15 papers about suicidality, three about aggression/hostility, seven about psychosis/mania, six about seizures, seven about hepatic effects, 29 about cardiovascular effects, and 28 about growth and development. The main findings (i.e., those from the largest and most well-conducted studies/analyses) are as follows. A large register-based study of pediatric and adult patients (6818 received atomoxetine) calculated a hazard ratio of 0.96 for suicide-related events during treatment with atomoxetine, and a meta-analysis of 23 placebo-controlled studies (N = 3883), published in 2014, found no completed suicides and no statistically significant association between atomoxetine and suicidality. The frequency of aggression/hostility was not statistically significantly higher with atomoxetine, e.g., experienced by 1.6 % (N = 21/1308) of atomoxetine-treated patients versus 1.1 % (N = 9/806) of placebo-treated patients in one meta-analysis. Symptoms of psychosis and mania were mainly observed in patients with comorbid bipolar disorder/depression. Based on spontaneous reports, during a 2-year period when 2.233 million adult and pediatric patients were exposed to atomoxetine, the reporting rate for seizures was 8 per 100,000 patients. In the manufacturer’s database, atomoxetine was a “probable cause” of three hepatic adverse events (AEs) (all reversible hepatitis), and 133 hepatic AEs had possible confounding factors and were “possibly related” to atomoxetine, during 4 years when atomoxetine exposure had reached about 4.3 million patients. Rare cases of severe liver injury are described in the US label and European SPC; a case requiring liver transplantation is described in the US label. In a comprehensive review of a clinical trials database (N = 8417 received atomoxetine), most pediatric patients experienced modest increases in heart rate and blood pressure, and 8–12 % experienced more pronounced changes (≥20 bpm, ≥15 to 20 mmHg). However, in three long-term analyses (≥2 years), blood pressure was within age norms, and few patients discontinued due to cardiovascular AEs. As described in the European SPC, QT interval prolongation is uncommon, e.g., in an open-label study, 1.4 % of 711 children and adolescents had prolonged QTc intervals (≥450 ms in males, ≥470 ms in females) that were not clinically significant at ≥3 years of treatment with atomoxetine. The European SPC warns about potential QT interval prolongation in patients with a personal or family history, or if atomoxetine is administered with other drugs that potentially affect the QT interval. Decreases in growth (weight and height gain) occurred and were greatest in patients of above average weight and height, but appeared to recover over 2–5 years of atomoxetine treatment. In conclusion, suicidality, aggression/hostility, psychosis, seizures, liver injuries, and prolonged QT interval are uncommon or rare in children and adolescents treated with atomoxetine, based on data from the predefined search and from the European SPC. Overall, the data that we assessed from our search do not suggest that associations exist between atomoxetine and suicidality or seizures. The data also suggest that an association may not exist between atomoxetine and aggression/hostility. While atomoxetine may affect the cardiovascular system, the data suggest these effects are not clinically significant in most patients. Reductions in growth appear to be reversible in the long term.


Reproduced from Spencer et al. [84], with permission
Similar content being viewed by others
Notes
The SPC language provided in this review article is accurate and consistent across EU member states that participate in the mutual recognition procedure for Strattera, plus Norway and Iceland. At present, this applies to 25 of the 28 EU member states, excluding France and Bulgaria, where licenses are not currently held for Strattera, and Croatia. Information about the mutual recognition procedure can be found at http://www.hma.eu/medicinesapprovalsystem.html [94].
With the exception that the ‘seizures’ topic is not in the ‘warnings and precautions’ section of the US label, but is in the ‘adverse reactions’ section.
The current US label states that pediatric patients treated with atomoxetine “should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases”. A similar statement is also in the European SPC. In addition, the US label states that “anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania and mania” may be “precursors to emerging suicidality”.
In the current European SPC and US label, for children and adolescents, the target maintenance dose is 1.2 mg/kg/day in patients up to 70 kg body weight, and 80 mg/day in patients over 70 kg body weight (as a single dose in the morning, or twice daily as an evenly divided dose in the morning and late afternoon/early evening).
Of the seven safety topics reported in this review article, all the topics except “seizures” are in the “warnings and precautions” section of the US label. “Seizures” are in the “adverse reactions” section of the US label.
Since October 2011, the following statement has been included in the US label, “Pulse and blood pressure should be measured at baseline, following STRATTERA dose increases, and periodically while on therapy to detect possible clinically important increases.” The European SPC states “It is recommended that heart rate and blood pressure be measured and recorded before treatment is started and, during treatment, after each adjustment of dose and then at least every 6 months to detect possible clinically important increases.”
Between December 2011 and May 2013, a range of 6–12 % of patients, including adults, was shown in the European SPC.
The possibility of QT interval prolongation has been reported in the European SPC since May 2006 and in the approved US label since October 2006, initially based on spontaneous reports. In the current European SPC and US label, clinical trial data about QT interval prolongation are limited to one study in healthy adult CYP2D6 poor metabolizers. The US label states, “No large changes in QTc interval (i.e., increases >60 ms from baseline, absolute QTc >480 ms) were observed in the study. However, small changes in QTc interval cannot be excluded from the current study, because the study failed to demonstrate assay sensitivity. There was a slight increase in QTc interval with increased atomoxetine concentration.” The European SPC also highlights that QT interval prolongation has been reported “very rarely” in cases of overdose; that there is “the potential for an increased risk of QT interval prolongation when atomoxetine is administered with other QT prolonging drugs (such as neuroleptics, class IA and III anti-arrhythmics, moxifloxacin, erythromycin, methadone, mefloquine, tricyclic antidepressants, lithium, or cisapride), drugs that cause electrolyte imbalance (such as thiazide diuretics), and drugs that inhibit CYP2D6”; and that “atomoxetine should be used with caution in patients with congenital or acquired long QT or a family history of QT prolongation.”
Atomoxetine is contraindicated in patients with “severe cardiac or vascular disorders” in the USA (between June 2012 and August 2013, the term “severe cardiovascular disorders” was used in the US label, instead of “severe cardiac or vascular disorders”). Atomoxetine has been contraindicated in patients with “severe cardiovascular or cerebrovascular disorders” in Europe since December 2011. According to the US label, atomoxetine “should not be used in patients with severe cardiac or vascular disorders whose condition would be expected to deteriorate if they experience increases in blood pressure or heart rate that could be clinically important (for example, 15 to 20 mm Hg in blood pressure or 20 beats per minute in heart rate).” Similar language was also used in the European SPC until May 2013, when the wording was changed so that atomoxetine is contraindicated for all patients with “severe cardiovascular or cerebrovascular disorders.” The European SPC states, “Severe cardiovascular disorders may include severe hypertension, heart failure, arterial occlusive disease, angina, haemodynamically significant congenital heart disease, cardiomyopathies, myocardial infarction, potentially life-threatening arrhythmias and channelopathies (disorders caused by the dysfunction of ion channels). Severe cerebrovascular disorders may include cerebral aneurysm or stroke.”
Reports of sudden deaths of atomoxetine-treated patients with structural cardiac abnormalities have been included in the European SPC since November 2008, and in the US label since October 2006. The European SPC currently states that “atomoxetine should only be used with caution in patients with known serious structural cardiac abnormalities and in consultation with a cardiac specialist”. The US label is more cautious, stating that “atomoxetine generally should not be used in children or adolescents with known serious structural cardiac abnormalities, cardiomyopathy, serious heart rhythm abnormalities, or other serious cardiac problems that may place them at increased vulnerability to the noradrenergic effects of atomoxetine”.
None of the studies captured using the predefined search terms were large epidemiological studies in which the goal was to analyze severe/serious cardiovascular AEs in children and adolescents treated with atomoxetine. We are aware of two large epidemiological studies that had this aim, but these studies did not fulfil the predefined search criteria, as they included patients aged <6 years and are not reported in the predefined search results in Sect. 3. Nevertheless, these two studies [92, 93] are discussed in Sect. 4.
Whereas weight does not necessarily reflect growth, it can be used as an indicator of growth and development.
Of 1312 patients at baseline, 61 had data at baseline and at 5 years, 926 patients discontinued during the 5 years, and it appeared that the remainder were still enrolled in the study but had not reached the 5-year time point.
References
Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry. 2003;2:104–13.
Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490–9.
Polanczyk G, de Lima MS, Horta BL, et al. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942–8.
Polanczyk GV, Willcutt EG, Salum GA, et al. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol. 2014;43:434–42.
Rasmussen P, Gillberg C. Natural outcome of ADHD with developmental coordination disorder at age 22 years: a controlled, longitudinal, community-based study. J Am Acad Child Adolesc Psychiatry. 2000;39:1424–31.
Biederman J, Faraone SV. The effects of attention-deficit/hyperactivity disorder on employment and household income. MedGenMed. 2006;8:12.
Doshi JA, Hodgkins P, Kahle J, et al. Economic impact of childhood and adult attention-deficit/hyperactivity disorder in the United States. J Am Acad Child Adolesc Psychiatry. 2012;51:990–1002.
Langley K, Fowler T, Ford T, et al. Adolescent clinical outcomes for young people with attention-deficit hyperactivity disorder. Br J Psychiatry. 2010;196:235–40.
Dalsgaard S, Mortensen PB, Frydenberg M, Thomsen PH. Long-term criminal outcome of children with attention deficit hyperactivity disorder. Crim Behav Ment Health. 2013;23:86–98.
Dalsgaard S, Østergaard SD, Leckman JF, et al. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385:2190–6.
Barbaresi WJ, Colligan RC, Weaver AL, et al. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131:637–44.
Savill NC, Buitelaar JK, Anand E, et al. The efficacy of atomoxetine for the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a comprehensive review of over a decade of clinical research. CNS Drugs. 2015;29:131–51.
Bolea-Alamañac B, Nutt DJ, Adamou M, British Association for Psychopharmacology, et al. Evidence-based guidelines for the pharmacological management of attention deficit hyperactivity disorder: update on recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2014;28:179–203.
Hazell PL, Kohn MR, Dickson R, et al. Core ADHD symptom improvement with atomoxetine versus methylphenidate: a direct comparison meta-analysis. J Atten Disord. 2011;15:674–83.
Hanwella R, Senanayake M, de Silva V. Comparative efficacy and acceptability of methylphenidate and atomoxetine in treatment of attention deficit hyperactivity disorder in children and adolescents: a meta-analysis. BMC Psychiatry. 2011;11:176.
Newcorn JH, Sutton VK, Weiss MD, Sumner CR. Clinical responses to atomoxetine in attention-deficit/hyperactivity disorder: the Integrated Data Exploratory Analysis (IDEA) study. J Am Acad Child Adolesc Psychiatry. 2009;48:511–8.
Panei P, Arcieri R, Bonati M, et al. Safety of psychotropic drug prescribed for attention-deficit/hyperactivity disorder in Italy. Adverse Drug React Bull. 2010;260:999–1002.
Ruggiero S, Rafaniello C, Bravaccio C, et al. Safety of attention-deficit/hyperactivity disorder medications in children: an intensive pharmacosurveillance monitoring study. J Child Adolesc Psychopharmacol. 2012;22:415–22.
Didoni A, Sequi M, Panei P, et al. One-year prospective follow-up of pharmacological treatment in children with attention-deficit/hyperactivity disorder. Eur J Clin Pharmacol. 2011;67:1061–7.
Arcieri R, Germinario EA, Bonati M, et al. Cardiovascular measures in children and adolescents with attention-deficit/hyperactivity disorder who are new users of methylphenidate and atomoxetine. J Child Adolesc Psychopharmacol. 2012;22:423–31.
Germinario EA, Arcieri R, Bonati M, et al. Attention-deficit/hyperactivity disorder drugs and growth: an Italian prospective observational study. J Child Adolesc Psychopharmacol. 2013;23:440–7.
STRATTERA®. Summary of product characteristics. Eli Lilly & Co. http://www.medicines.org.uk/emc/history/14482 Accessed 1 Dec 2015.
STRATTERA®. Full prescribing information. Eli Lilly & Co. http://pi.lilly.com/us/strattera-pi.pdf Accessed 1 Dec 2015.
STRATTERA®. Full prescribing information. Eli Lilly & Co. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.Label_ApprovalHistory#apphist Accessed 1 Dec 2015.
Chen Q, Sjölander A, Runeson B, et al. Drug treatment for attention-deficit/hyperactivity disorder and suicidal behaviour: register based study. BMJ. 2014;348:g3769.
Bangs ME, Wietecha LA, Wang S, et al. Meta-analysis of suicide-related behavior or ideation in child, adolescent, and adult patients treated with atomoxetine. J Child Adolesc Psychopharmacol. 2014;24:426–34.
Schwartz S, Correll CU. Efficacy and safety of atomoxetine in children and adolescents with attention-deficit/hyperactivity disorder: results from a comprehensive meta-analysis and metaregression. J Am Acad Child Adolesc Psychiatry. 2014;53:174–87.
Atomoxetine ADHD and Comorbid MDD Study Group, Bangs ME, Emslie GJ, et al. Efficacy and safety of atomoxetine in adolescents with attention-deficit/hyperactivity disorder and major depression. J Child Adolesc Psychopharmacol. 2007;17:407–20.
Bangs ME, Tauscher-Wisniewski S, Polzer J, et al. Meta-analysis of suicide-related behavior events in patients treated with atomoxetine. J Am Acad Child Adolesc Psychiatry. 2008;47:209–18.
Donnelly C, Bangs M, Trzepacz P, et al. Safety and tolerability of atomoxetine over 3 to 4 years in children and adolescents with ADHD. J Am Acad Child Adolesc Psychiatry. 2009;48:176–85.
Garside D, Ropero-Miller JD, Riemer EC. Postmortem tissue distribution of atomoxetine following fatal and nonfatal doses: three case reports. J Forensic Sci. 2006;51:179–82.
Tamayo JM, Pumariega A, Rothe EM, et al. Latino versus Caucasian response to atomoxetine in attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2008;18:44–53.
Wehmeier PM, Schacht A, Lehmann M, et al. Emotional well-being in children and adolescents treated with atomoxetine for attention-deficit/hyperactivity disorder: findings from a patient, parent and physician perspective using items from the pediatric adverse event rating scale (PAERS). Child Adolesc Psychiatry Ment Health. 2008;2(1):11.
Paxton GA, Cranswick NE. Acute suicidality after commencing atomoxetine. J Paediatr Child Health. 2008;44:596–8.
Kilincaslan A, Mutluer T, Pasabeyoglu B, et al. Treatment of children with autism spectrum disorders and co-existing attention deficit hyperactivity disorder, with atomoxetine: a retrospective study. In: 5th international congress on psychopharmacology and international symposium on child and adolescent psychopharmacology: Turkey; 30 Oct–3 Nov 2013.
Bushe CJ, Savill NC. Suicide related events and attention deficit hyperactivity disorder treatments in children and adolescents: a meta-analysis of atomoxetine and methylphenidate comparator clinical trials. Child Adolesc Psychiatry Ment Health. 2013;7:19.
McCarthy S, Cranswick N, Potts L, et al. Mortality associated with attention-deficit hyperactivity disorder (ADHD) drug treatment: a retrospective cohort study of children, adolescents and young adults using the general practice research database. Drug Saf. 2009;32:1089–96.
Polzer J, Bangs ME, Zhang S, et al. Meta-analysis of aggression or hostility events in randomized, controlled clinical trials of atomoxetine for ADHD. Biol Psychiatry. 2007;61:713–9.
Chang K, Nayar D, Howe M, et al. Atomoxetine as an adjunct therapy in the treatment of co-morbid attention-deficit/hyperactivity disorder in children and adolescents with bipolar I or II disorder. J Child Adolesc Psychopharmacol. 2009;19:547–51.
Hah M, Chang K. Atomoxetine for the treatment of attention-deficit/hyperactivity disorder in children and adolescents with bipolar disorders. J Child Adolesc Psychopharmacol. 2005;15:996–1004.
Aydemir H, Oztop DB, Uytun MC, et al. Is it ADHD or bipolar disorders? A case report. In: 5th international congress on psychopharmacology and international symposium on child and adolescent psychopharmacology: Turkey; 30 Oct–3 Nov 2013.
Guney E, Uneri OS. Atomoxetine induced hypomania-like symptoms in a pre-adolescent patient. In: 5th international congress on psychopharmacology and international symposium on child and adolescent psychopharmacology: Turkey; 30 Oct–3 Nov 2013.
Bhattacharjee S, Chen H, Bhatara V, et al. Is stimulant or atomoxetine utilization associated with neurological adverse events in children with attention-deficit/hyperactivity disorder (ADHD)? A retrospective analysis of propensity score matched data. Value Health. 2011;14:A185.
Dumitru I, Salan A. Treating children with epilepsy and comorbid attention-deficit/hyperactivity disorder (ADHD). Eur J Neurol. 2012;19:208.
McAfee AT, Holdridge KC, Johannes CB, et al. The effect of pharmacotherapy for attention deficit hyperactivity disorder on risk of seizures in pediatric patients as assessed in an insurance claims database. Curr Drug Saf. 2008;3:123–31.
McAfee AT, Landon J, Jones M, et al. A cohort study of the risk of seizures in a pediatric population treated with atomoxetine or stimulant medications. Pharmacoepidemiol Drug Saf. 2013;22:386–93.
Wernicke JF, Holdridge KC, Jin L, et al. Seizure risk in patients with attention-deficit-hyperactivity disorder treated with atomoxetine. Dev Med Child Neurol. 2007;49:498–502.
Bangs ME, Jin L, Zhang S, et al. Hepatic events associated with atomoxetine treatment for attention-deficit hyperactivity disorder. Drug Saf. 2008;31:345–54.
Lim JR, Faught PR, Chalasani NP, et al. Severe liver injury after initiating therapy with atomoxetine in two children. J Pediatr. 2006;148:831–4.
Stojanovski SD, Casavant MJ, Mousa HM, et al. Atomoxetine-induced hepatitis in a child. Clin Toxicol (Phila). 2007;45:51–5.
Uneri OS, Copur M, Tanidir C, et al. Liver enzymes levels during atomoxetine treatment in children and adolescents. Eur Child Adolesc Psychiatry. 2011;20:S204.
Uneri OS, Copur M, Tanidir C, et al. Liver enzymes and bilirubin levels during atomoxetine treatment in children and adolescents. Düşünen Adam. 2013;26:22–7.
Allen AJ, Kurlan RM, Gilbert DL, et al. Atomoxetine treatment in children and adolescents with ADHD and comorbid tic disorders. Neurology. 2005;65:1941–9.
Camporeale A, Beasley C, Tanaka Y, et al. Changes in blood pressure and heart rate associated with atomoxetine treatment in attention-deficit/hyperactivity disorder. Eur Neuropsychopharmacol. 2012;22:S429–30.
Cardo E, Porsdal V, Quail D, et al. Fast vs. slow switching from stimulants to atomoxetine in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2013;23:252–61.
Carlson GA, Dunn D, Kelsey D, et al. A pilot study for augmenting atomoxetine with methylphenidate: safety of concomitant therapy in children with attention-deficit/hyperactivity disorder. Child Adolesc Psychiatry Ment Health. 2007;1(10). doi:10.1186/1753-2000-1-10.
Escobar R, Soutullo C, San Sebastián J, et al. Atomoxetine safety and efficacy in children with attention deficit/hyperactivity disorder (ADHD): initial phase of 10-week treatment in a relapse prevention study with a Spanish sample [in Spanish]. Actas Esp Psiquiatr. 2005;33:26–32.
Hammerness P, Georgiopoulos A, Doyle RL, et al. An open study of adjunct OROS-methylphenidate in children who are atomoxetine partial responders: II. Tolerability and pharmacokinetics. J Child Adolesc Psychopharmacol. 2009;19:493–9.
Kratochvil CJ, Newcorn JH, Arnold LE, et al. Atomoxetine alone or combined with fluoxetine for treating ADHD with comorbid depressive or anxiety symptoms. J Am Acad Child Adolesc Psychiatry. 2005;44:915–24.
Kratochvil CJ, Wilens TE, Greenhill LL, et al. Effects of long-term atomoxetine treatment for young children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2006;45:919–27.
Sert A, Gokcen C, Aypar E, et al. Effects of atomoxetine on cardiovascular functions and on QT dispersion in children with attention deficit hyperactivity disorder. Cardiol Young. 2012;22:158–61.
Spencer TJ, Sallee FR, Gilbert DL, et al. Atomoxetine treatment of ADHD in children with comorbid Tourette syndrome. J Atten Disord. 2008;11:470–81.
Stojanovski SD, Robinson RF, Baker SD, et al. Children and adolescent exposures to atomoxetine hydrochloride reported to a poison control center. Clin Toxicol (Phila). 2006;44:243–7.
Takahashi M, Takita Y, Yamazaki K, et al. A randomized, double-blind, placebo-controlled study of atomoxetine in Japanese children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19:341–50.
Trzepacz PT, Williams DW, Feldman PD, et al. CYP2D6 metabolizer status and atomoxetine dosing in children and adolescents with ADHD. Eur Neuropsychopharmacol. 2008;18:79–86.
Wernicke JF, Faries D, Girod D, et al. Cardiovascular effects of atomoxetine in children, adolescents, and adults. Drug Saf. 2003;26:729–40.
Wilens TE, Kratochvil C, Newcorn JH, et al. Do children and adolescents with ADHD respond differently to atomoxetine? J Am Acad Child Adolesc Psychiatry. 2006;45:149–57.
Wilens TE, Newcorn JH, Kratochvil CJ, et al. Long-term atomoxetine treatment in adolescents with attention-deficit/hyperactivity disorder. J Pediatr. 2006;149:112–9.
Michelson D, Read HA, Ruff DD, et al. CYP2D6 and clinical response to atomoxetine in children and adolescents with ADHD. J Am Acad Child Adolesc Psychiatry. 2007;46:242–51.
Newcorn JH, Michelson D, Kratochvil CJ, et al. Low-dose atomoxetine for maintenance treatment of attention-deficit/hyperactivity disorder. Pediatrics. 2006;118:e1701–6.
Prasad S, Furr AJ, Zhang S, et al. Baseline values from the electrocardiograms of children and adolescents with ADHD. Child Adolesc Psychiatry Ment Health. 2007;1:11.
Quintana H, Cherlin EA, Duesenberg DA, et al. Transition from methylphenidate or amphetamine to atomoxetine in children and adolescents with attention-deficit/hyperactivity disorder-a preliminary tolerability and efficacy study. Clin Ther. 2007;29:1168–77.
Gundogdu U, Benk F, Bahadir AT, et al. Treatment with atomoxetine: a case with Williams syndrome. Bulletin of Clinical Psychopharmacology. In: Conference: 5th international congress on psychopharmacology and international symposium on child and adolescent psychopharmacology: Turkey; 30 Oct–3 Nov 2013.
Dittmann RW, Cardo E, Nagy P, et al. Efficacy and safety of lisdexamfetamine dimesylate and atomoxetine in the treatment of attention-deficit/hyperactivity disorder: a head-to-head, randomized, double-blind, phase IIIb study. CNS Drugs. 2013;27:1081–92.
Garg J, Arun P, Chavan BS. Comparative short term efficacy and tolerability of methylphenidate and atomoxetine in attention deficit hyperactivity disorder. Indian Pediatr. 2014;51:550–4.
Yamaguchi H, Nagumo K, Nakashima T, et al. Life-threatening QT prolongation in a boy with attention-deficit/hyperactivity disorder on atomoxetine. Eur J Pediatr. 2014;173(12):1631–4.
Bhagat A, Deshmukh V, Shah M, et al. Appetite and weight loss in children with attention deficit hyperactivity disorder taking atomoxetine. Indian J Psychiatry. 2011;1:S69–70.
Biederman J, Wigal SB, Spencer TJ, et al. A post hoc subgroup analysis of an 18-day randomized controlled trial comparing the tolerability and efficacy of mixed amphetamine salts extended release and atomoxetine in school-age girls with attention-deficit/hyperactivity disorder. Clin Ther. 2006;28:280–93.
Dell’Agnello G, Maschietto D, Bravaccio C, et al. Atomoxetine hydrochloride in the treatment of children and adolescents with attention-deficit/hyperactivity disorder and comorbid oppositional defiant disorder: a placebo-controlled Italian study. Eur Neuropsychopharmacol. 2009;19:822–34.
Durell TM, Pumariega AJ, Rothe EM, et al. Effects of open-label atomoxetine on African–American and Caucasian pediatric outpatients with attention-deficit/hyperactivity disorder. Ann Clin Psychiatry. 2009;21:26–37.
Kratochvil CJ, Bohac D, Harrington M, et al. An open-label trial of tomoxetine in pediatric attention deficit hyperactivity disorder. J Child Adolesc Psychopharmacol. 2001;11:167–70.
Martenyi F, Zavadenko NN, Jarkova NB, et al. Atomoxetine in children and adolescents with attention-deficit/hyperactivity disorder: a 6-week, randomized, placebo-controlled, double-blind trial in Russia. Eur Child Adolesc Psychiatry. 2010;19:57–66.
Spencer TJ, Newcorn JH, Kratochvil CJ, et al. Effects of atomoxetine on growth after 2-year treatment among pediatric patients with attention-deficit/hyperactivity disorder. Pediatrics. 2005;116:e74–80.
Spencer TJ, Kratochvil CJ, Sangal RB, et al. Effects of atomoxetine on growth in children with attention-deficit/hyperactivity disorder following up to five years of treatment. J Child Adolesc Psychopharmacol. 2007;17:689–700.
Trzepacz PT, Spencer TJ, Zhang S, et al. Effect of atomoxetine on Tanner stage sexual development in children and adolescents with attention deficit/hyperactivity disorder: 18-month results from a double-blind, placebo-controlled trial. Curr Med Res Opin. 2011;27(Suppl 2):45–52.
Wang Y, Zheng Y, Du Y, et al. Atomoxetine versus methylphenidate in paediatric outpatients with attention deficit hyperactivity disorder: a randomized, double-blind comparison trial. Aust N Z J Psychiatry. 2007;41:222–30.
Yildiz O, Sismanlar SG, Memik NC, et al. Atomoxetine and methylphenidate treatment in children with ADHD: the efficacy, tolerability and effects on executive functions. Child Psychiatry Hum Dev. 2011;42:257–69.
Posey DJ, Wiegand RE, Wilkerson J, et al. Open-label atomoxetine for attention-deficit/hyperactivity disorder symptoms associated with high-functioning pervasive developmental disorders. J Child Adolesc Psychopharmacol. 2006;16:599–610.
Pott W, Albayrak O, Hinney A, et al. Successful treatment with atomoxetine of an adolescent boy with attention deficit/hyperactivity disorder, extreme obesity, and reduced melanocortin 4 receptor function. Obes Facts. 2013;6:109–15.
Davies M, Cornelius V, Fogg C, et al. A study to examine events of suicidal ideation in patients prescribed atomoxetine in England; results of an interim modified prescription event monitoring study. Drug Saf. 2009;32(10):976.
Linden S, Bussing R, Gerhard T, et al. Risk of suicide and suicide attempt associated with atomoxetine compared to central nervous system stimulant treatment. Pharmacoepidemiol Drug Saf. 2013;22(Suppl 1):175–6.
Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365:1896–904.
Schelleman H, Bilker WB, Strom BL, et al. Cardiovascular events and death in children exposed and unexposed to ADHD agents. Pediatrics. 2011;127(6):1102–10.
Heads of Medicines Agencies (HMA). Medicines approval system. http://www.hma.eu/medicinesapprovalsystem.html. Accessed 2 Dec 2015.
Bushe CJ, Savill NC. Systematic review of atomoxetine data in childhood and adolescent attention-deficit hyperactivity disorder 2009–2011: focus on clinical efficacy and safety. J Psychopharmacol. 2014;28:204–11.
Duff G. Strattera (atomoxetine)—conclusions of a risk:benefit review. MHRA. 2006. http://webarchive.nationalarchives.gov.uk/20141205150130/. http://www.mhra.gov.uk/Safetyinformation/Safetywarningsalertsandrecalls/Safetywarningsandmessagesformedicines/CON2023222. Accessed 9 July 2015.
MHRA public assessment report. Atomoxetine: a review of the effects on heart rate and blood pressure. 2012. http://www.mhra.gov.uk/home/groups/s-par/documents/websiteresources/con152778.pdf. Accessed 9 July 2015.
MHRA public assessment report. Strattera 4 mg/mL oral solution (atomoxetine hydrochloride). 2014. http://www.mhra.gov.uk/home/groups/par/documents/websiteresources/con493430.pdf. Accessed 9 July 2015.
Cortese S, Castellanos FX. The relationship between ADHD and obesity: implications for therapy. Expert Rev Neurother. 2014;14:473–9.
Cortese S, Comencini E, Vincenzi B, et al. Attention-deficit/hyperactivity disorder and impairment in executive functions: a barrier to weight loss in individuals with obesity? BMC Psychiatry. 2013;13:286.
Kompus K, Løberg EM, Posserud MB, Lundervold AJ. Prevalence of auditory hallucinations in Norwegian adolescents: Results from a population-based study. Scand J Psychol. Epub. 2015;. doi:10.1111/sjop.12219.
Bartels-Velthuis AA, Jenner JA, van de Willige G, et al. Prevalence and correlates of auditory vocal hallucinations in middle childhood. Br J Psychiatry. 2010;196:41–6.
Bartels-Velthuis AA, van de Willige G, Jenner JA, et al. Course of auditory vocal hallucinations in childhood: 5-year follow-up study. Br J Psychiatry. 2011;199:296–302.
Reinblatt SP, Mahone EM, Tanofsky-Kraff M, et al. Pediatric loss of control eating syndrome: association with attention-deficit/hyperactivity disorder and impulsivity. Int J Eat Disord. 2015. doi:10.1002/eat.22404.
Chronis-Tuscano A, Molina BS, Pelham WE, et al. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2010;67:1044–51.
Bakken RJ, Paczkowski M, Kramer HP, et al. Effects of atomoxetine on attention-deficit/hyperactivity disorder in clinical pediatric treatment settings: a naturalistic study. Curr Med Res Opin. 2008;24:449–60.
Hammerness PG, Karampahtsis C, Babalola R, et al. Attention-deficit/hyperactivity disorder treatment: what are the long-term cardiovascular risks? Expert Opin Drug Saf. 2015;14:543–51.
Davis SM, Katusic SK, Barbaresi WJ, et al. Epilepsy in children with attention-deficit/hyperactivity disorder. Pediatr Neurol. 2010;42:325–30.
Hesdorffer DC, Ludvigsson P, Olafsson E, et al. ADHD as a risk factor for incident unprovoked seizures and epilepsy in children. Arch Gen Psychiatry. 2004;61:731–6.
Chou IC, Chang YT, Chin ZN, et al. Correlation between epilepsy and attention deficit hyperactivity disorder: a population-based cohort study. PLoS ONE. 2013;8:e57926.
Socanski D, Aurlien D, Herigstad A, et al. Epilepsy in a large cohort of children diagnosed with attention deficit/hyperactivity disorders (ADHD). Seizure. 2013;22:651–5.
Ercan E, Ercan ES, Atılgan H, et al. Predicting aggression in children with ADHD. Child Adolesc Psychiatry Ment Health. 2014;8:15.
Savill N, Bushe CJ. A systematic review of the safety information contained within the Summaries of Product Characteristics of medications licensed in the United Kingdom for Attention Deficit Hyperactivity Disorder. How does the safety prescribing advice compare with national guidance? Child Adolesc Psychiatry Ment Health. 2012;6(1):2. doi:10.1186/1753-2000-6-2.
Retz W, Rösler M. The relation of ADHD and violent aggression: What can we learn from epidemiological and genetic studies? Int J Law Psychiatry. 2009;32:235–43.
Lifford KJ, Harold GT, Thapar A. Parent-child hostility and child ADHD symptoms: a genetically sensitive and longitudinal analysis. J Child Psychol Psychiatry. 2009;50:1468–76.
Vitiello B, Elliott GR, Swanson JM, et al. Blood pressure and heart rate over 10 years in the multimodal treatment study of children with ADHD. Am J Psychiatry. 2012;169(2):167–77.
Swanson JM, Elliott GR, Greenhill LL, et al. Effects of stimulant medication on growth rates across 3 years in the MTA follow-up. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1015–27.
Wietecha LA, Ruff DD, Allen AJ, et al. Atomoxetine tolerability in pediatric and adult patients receiving different dosing strategies. J Clin Psychiatry. 2013;74(12):1217–23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This review was funded by Eli Lilly & Company. Michael Riley, PhD, from Trilogy Writing and Consulting GmbH, Frankfurt, Germany, provided medical writing support on behalf of Eli Lilly & Co.
Conflict of interest
NC Savill, KA Day, E Anand, T Treuer, H Upadhyaya, and LA Kryzhanovskaya are full-time employees and stock holders of Eli Lilly & Co. VA Reed is a full-time employee of Eli Lilly & Co. JK Buitelaar has been a consultant, a member of an advisory board, and/or a speaker for Janssen-Cilag BV, Eli Lilly, Bristol-Myers Squibb, Organon/Schering Plough, UCB, Shire, Medice, and Servier. DR Coghill has received grants to support research from Shire and Vifor Pharma; honoraria for participation in advisory boards for Shire, Novartis, and Sandoz; speaker fees for Shire, Novartis, and Eli Lilly; royalties from Oxford University Press; and has provided expert testimony for GlaxoSmithKline.
Appendix
Appendix
1.1 Strategy Used to Search Embase, Ovid MEDLINE(R), and Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations
The search was originally conducted up to July 2013, as shown below. However, it was updated to include literature published up to 16 August 2014 (not shown).
Database: Embase <1974 to 2013 July 25>, Ovid MEDLINE(R) <1946 to July week 3 2013>, Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations <July 25, 2013>
1 exp atomoxetine/(3060) |
2 exp attention deficit disorder/(54376) |
3 1 and 2 (2079) |
4 limit 3 to (human and (child <unspecified age> or preschool child <1 to 6 years> or school child <7 to 12 years> or adolescent <13 to 17 years>)) [Limit not valid in Ovid MEDLINE(R), Ovid MEDLINE(R) In-Process; records were retained] (725) |
5 limit 4 to yr = ”2001–Current” (722) |
6 5 use oemezd (722) |
7 atomoxetine.mp. (4248) |
8 tomoxetine.mp. (146) |
9 LY139603.mp. (17) |
10 7 or 8 or 9 (4289) |
11 exp Attention Deficit Disorder with Hyperactivity/ (54376) |
12 10 and 11 (2818) |
13 limit 12 to (humans and yr = ”2001–Current” and “all child (0 to 18 years)”) [Limit not valid in Embase; records were retained] (2468) |
14 13 use mesz,prem (476) |
15 6 or 14 (1198) |
16 remove duplicates from 15 (879) |
Rights and permissions
About this article
Cite this article
Reed, V.A., Buitelaar, J.K., Anand, E. et al. The Safety of Atomoxetine for the Treatment of Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A Comprehensive Review of Over a Decade of Research. CNS Drugs 30, 603–628 (2016). https://doi.org/10.1007/s40263-016-0349-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-016-0349-0