Abstract
Morphine is a drug commonly administered via the epidural or intrathecal route, and is regarded by many as the ‘gold-standard’ single-dose neuraxial opioid due to its postoperative analgesic efficacy and prolonged duration of action. However, respiratory depression is a recognized side effect of neuraxial morphine administered in the perioperative setting. We conducted an extensive review of articles published since 1945 that examine respiratory depression or failure associated with perioperative intrathecal or epidural morphine use.
Respiratory depression was previously thought to result from the interaction of opioid in the cerebrospinal fluid with ventral medullary opioid receptors. More recently, the preBötzinger complex located in the medulla has been identified as the site responsible for the decrease in respiratory rate following systemic administration of opioids. Neurons in the preBötzinger complex expressing neurokinin-1 receptors are selectively inhibited by opioids, and therefore are the mediators of opioid-induced respiratory depression.
Epidural, intrathecal and plasma pharmacokinetics of opioids are complex, vary between neuraxial compartments, and can even differ within the epidural space itself depending upon level of insertion. Caution should be exercised when prescribing systemic opioids (intravenous or oral) in addition to neuraxial morphine as this can compound the potential for early or delayed respiratory depression.
There is a wide range of incidences for respiratory depression following neuraxial morphine in a perioperative setting. Disparity of definitions used for the diagnosis of respiratory depression in the literature precludes identification of the exact incidence of this rare event.
The optimal neuraxial opioid dose is a balance between the conflicting demands of providing optimal analgesia while minimizing dose-related adverse effects. Dose-response studies show that neuraxial morphine appears to have an analgesic efficacy ‘ceiling’. The optimal ‘single-shot’ intrathecal dose appears to be 0.075–0.15mg and the ideal ‘single-shot’ epidural morphine dose is 2.5–3.75mg. Analgesic efficacy studies have not been adequately powered to show differences in the incidence of clinically significant respiratory depression. Opioid antagonists such as naloxone to prevent or treat opioid-induced respiratory depression have a number of limitations. Researchers have recently focused on non-opioid drugs such as serotonin receptor agonists. Early evidence suggests that ampakine (α-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid [AMPA]) receptor modulators may be effective at reducing opioid-induced respiratory depression while maintaining analgesia. Sodium/proton exchanger type 3 (NHE3) inhibitors, which act centrally on respiratory pathways, also warrant further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1. Introduction
The discovery that opioid receptors are localized within lamina II of the dorsal horn in the CNS suggested that exogenous opioids could be administered via the neuraxial route to produce analgesia.[1] A number of published reports of intrathecal[2] and epidural[3] morphine administration in humans have since been published, and in 1984 preservative-free morphine received US FDA approval for neuraxial administration. Analgesia delivered via the neuraxial route lasts longer than the systemic route, with effects persisting 12–24 hours,[4] and in some cases longer, following administration.[5] Recognized benefits of neuraxial opioids when compared with intravenous administration include better postoperative analgesia, increased functional ability, earlier ambulation and earlier return of bowel function.[6,7] Furthermore, unlike with neuraxial local anaesthetics, there is negligible motor, sensory or autonomic blockade associated with neuraxial opioids.[2,3,8]
Neuraxial morphine is now extensively used in the perioperative setting[9] due to improved analgesia, greater duration of action and dose-sparing effects when compared with its administration via the systemic route. Despite significant analgesic advantages of neuraxial morphine over systemic administration, there are a number of potential adverse effects of which respiratory depression is the most concerning. Cases of life-threatening respiratory depression were reported soon after clinical administration of neuraxial morphine.[10–12] Recent closed-claims data found that 13 of 93 claims made between 1995 and 2007 were due to respiratory depression; six cases involved intravenous opioids, three cases involved neuraxial opioids, and in the remaining four cases the drug and route were not named. The majority of these cases resulted in significant morbidity or permanent brain damage, and resulted in treatment costs of approximate £2.75million.[13] Although the absolute risk of respiratory depression is small, concern for this adverse effect may result in underuse of neuraxial morphine for routine postoperative analgesia.[14]
This article reviews relevant publications addressing the issue of respiratory depression secondary to neuraxial morphine. A literature review of studies that examined neuraxial morphine-induced respiratory depression was performed. Published articles written in English between 1945 and 2010 were identified using the MEDLINE, Cochrane, EMBASE and Web of Science databases. Literature written in English using the terms ‘intrathecal or spinal or neuraxial or extradural or epidural or neuraxial’ and ‘opioid’, were combined with ‘respiratory depression or respiratory failure’. 360 articles were reviewed by hand, of which 165 were excluded. We selected 63 articles containing ‘opioids and neuraxial’ and 132 articles containing ‘morphine and neuraxial’. Additional articles were reviewed to explain certain points.
2. Pathophysiology of Respiratory Depression
Respiratory depression has been reported following both intrathecal and epidural morphine.[15,16] Respiratory depression following epidural morphine is classically described as biphasic,[17] with early (<2 hours) and delayed (>2 hours) presentations. Most reports of early respiratory depression involve lipophilic opioids (sufentanil or fentanyl) administered via the epidural route.[18–22]
Delayed respiratory depression is a phenomenon associated with hydrophilic morphine rather than lipophilic neuraxial opioids.[15,16] It usually occurs 6–12 hours following intrathecal or epidural administration and may persist up to 24 hours.[17,23,24] Delayed respiratory depression is caused by rostral spread in the cerebrospinal fluid (CSF) and slow penetration into the brainstem. High concentrations of μ-opioid receptors exist within the ventral medulla, which are important in the normal regulation of respiration. Direct application of small doses of opioid to the chemosensitive anterolateral surface of the medulla,[25,26] fourth or lateral ventricles,[27,28] or pontine or medullary respiratory centres can induce significant respiratory depression.[29] Respiratory depression was previously thought to result from the interaction of opioid in the CSF with ventral medullary opioid receptors.[30] Studies in rats suggested that respiratory depression occurring after the administration of opioids resulted from a dual effect involving μ- and δ-receptors.[31] More recently, the preBötzinger complex located in the medulla has been identified as the site responsible for the decrease in respiratory rate following systemic administration of opioids. Neurons in the preBötzinger complex expressing neurokinin-1 receptors are selectively inhibited by opioids, and therefore are the mediators of opioid-induced respiratory depression.[32]
3. Pharmacokinetics of Neuraxial Morphine
Epidural, intrathecal and plasma pharmacokinetics of opioids are complex, vary between neuraxial compartments, and can even differ within the epidural space itself depending upon level of insertion. The bioavailability of opioids in the intrathecal and epidural compartments is determined primarily by the drug’s hydrophobicity.[33] Hydrophilic morphine has a high CSF bioavailability, excellent spinal penetration, prolonged duration and less systemic absorption than lipophilic opioids. Morphine penetrates the spinal cord slowly, facilitating cephalad spread in the CSF. A poor correlation between the analgesic effect and plasma levels of morphine has been observed following epidural administration, suggesting a predominantly spinal effect.[34,35] Morphine levels within the CSF following intrathecal morphine administration are approximately 3 times those in plasma. Supra-spinal redistribution of morphine through the CSF plays an important role in the generation of analgesia and CNS side effects.[36]
The long duration of action of morphine is due to the slow rate of clearance of the drug from the opioid receptors.[37,38] In addition, morphine is absorbed more slowly from the intrathecal space than following epidural or intramuscular administration, further prolonging its analgesic effect.[39]
Direct administration of morphine into the CSF is the most efficient method of delivering opioid to the spinal cord receptors. Appreciable cervical CSF concentrations occur 1–5 hours after lumbar intrathecal morphine administration. Morphine reaches the cisterna magna and fourth and lateral ventricles by 1–2 and 3–6 hours, respectively.[40] The hyperbaric form of morphine decreases cephalad diffusion and minimizes the central depressant effects of the drug.[41] It remains within the CSF for prolonged periods and slowly diffuses to the plasma compartment.[42] Morphine is not metabolized within the CNS, and therefore morphine-6-glucoronide cannot be detected in CSF following intrathecal administration.[43] Elimination is thought to be dependent on reabsorption via arachnoid granulations.[44] The terminal elimination half-life of morphine within the CSF is 2–4 hours, similar to that within plasma.[45,46]
Peak blood and CSF levels of morphine occur at 10–15 minutes and 1–4 hours, respectively, following epidural administration.[38,46–48] Approximately 3% of the epidural morphine dose crosses the dura to enter the CSF.[46,47] Epidural morphine administration produces blood concentrations similar to those seen following an equivalent intra-muscular dose.[49] Animal studies examining behavioural and toxicological effects have failed to demonstrate neurotoxicity secondary to long-term administration of epidural and intrathecal morphine.[50]
4. Patients at Risk of Respiratory Depression
There are a number of well described risk factors for developing respiratory depression after neuraxial morphine (table I).[15,51–60] In 2009, the American Society of Anesthesiologists published practice guidelines for the prevention, detection and management of respiratory depression associated with neuraxial opioid administration.[52] These guidelines suggest that a history and physical examination directed at identifying risk factors, in particular sleep apnoea, should be performed in all patients prior to administration of neuraxial opioids. Importantly, opioid-induced respiratory depression can still occur in healthy patients receiving neuraxial morphine without co-existing morbidity,[53] and clinicians must anticipate this rare but hazardous event.[53,61] Caution should be exercised when prescribing systemic opioids (intravenous or oral) in addition to neuraxial morphine as this can compound the potential for early or delayed respiratory depression.
5. Incidence of Respiratory Depression
Numerous publications including randomized controlled trials, case reports, prospective and retrospective analyses of databases, surveys and meta-analyses have attempted to define the true incidence of respiratory depression associated with neuraxial morphine use. Disparity of definitions used for the diagnosis of respiratory depression precludes identification of the exact incidence of this rare event. Definitions have included respiratory rate, hypercarbia, low arterial oxygen saturation (SaO2), decreased level of consciousness, increased level of sedation, treatment with naloxone and decreased ventilator response to hypoxia or hypercarbia.[62] In addition, the incidence of respiratory depression following neuraxial morphine has been shown to be dose-dependent. Therefore, the reported incidence of respiratory depression from earlier studies using larger doses may not be relevant to current clinical practice which utilizes smaller neuraxial morphine doses.[15,63,64]
The incidences of respiratory depression determined from large retrospective and prospective database analyses are outlined in table II.[57,65–73] The incidence is 0.26–3% for intrathecal morphine in dose ranges of 0.15–0.8 mg, and 0–2.8% for epidural morphine administration with dose ranges of 2–5 mg. These incidences are similar to those reported by Etches et al.[64] in 1989 (0.09–3%). In their review, the authors commented that the true incidence was unknown due to the lack of well designed prospective studies at the time. More recently, two meta-analyses determined the incidence of respiratory depression in patients receiving low-dose (<0.2 and 0.2–0.3 mg) intrathecal morphine to be 0–1.2%.[51,74] Table III shows recent randomized controlled trials performed since 2000 not included in the two mentioned meta-analyses.[75–88] The incidence of respiratory depression in these studies ranges from 0% to 3.4% in the 985 patients receiving intrathecal morphine in dose ranges between 0.025 to 0.4 mg. Differences in the incidences among the studies may reflect different doses, additional analgesics utilized, different surgical populations, and various definitions used to define respiratory depression.
Studies indicate that the incidence of respiratory depression is not greater with neuraxial compared with systemic administration of morphine.[51,66,74,89] Although earlier studies suggested that respiratory depression was greater with intrathecal morphine compared with epidural administration,[15,37] these differences may be attributed to the higher intrathecal morphine doses used in those studies. More recent studies indicate that epidural and intrathecal morphine appear to provide similar analgesia and adverse effects (such as sedation, pruritus, nausea and vomiting) when an equipotent analgesia conversion ratio of 20–30 : 1 is used.[84,90,91] One potential disadvantage of epidural administration of morphine is that inadvertent subdural or intrathecal administration with a dose intended for the epidural route can lead to profound sedation and respiratory depression, potentially requiring opioid reversal, intensive care monitoring and ventilatory support.[92]
6. Neuraxial Morphine ‘Analgesic Ceiling’, Dose-Response and Dose-Related Adverse Effects
The optimal neuraxial opioid dose is essentially a balance between the conflicting demands of providing optimal analgesia while minimizing dose-related adverse effects. Several studies have attempted to determine the optimal dose of intrathecal and epidural morphine for postoperative analgesia.
6.1 Intrathecal Morphine Doses
Due to the widespread use of neuraxial opioids in obstetric patients, intrathecal and epidural morphine have been extensively studied in this setting. Palmer et al.[93] compared the analgesic efficacy of increasing intrathecal morphine doses (0, 0.025, 0.05, 0.075, 0.1, 0.2, 0.3, 0.4 and 0.5 mg) following caesarean delivery and found no significant analgesic benefit using doses greater than 0.075 mg. Another dose-response study of intrathecal morphine 0.05, 0.1 and 0.2 mg in the post-caesarean population observed that 0.1 and 0.2 mg provided comparable effective post-caesarean analgesia, while the 0.05 mg dose was less effective.[94] However, the incidence of adverse effects was greater with the 0.2 mg dose. Milner et al.[95] reported that intrathecal morphine 0.1 mg produced similar post-caesarean analgesia to that of 0.2 mg. There were no reports of respiratory depression, but the lower dose resulted in less nausea and vomiting. Similarly, Yang et al.[96] found that intrathecal morphine 0.1 mg compared with 0.25 mg, provided similar analgesia but with fewer adverse effects post-caesarean delivery. A post-caesarean analgesia study using a wide range of intrathecal morphine doses (0–0.2 mg), found that the dose that produced a 50% effective response (ED50) was 0.02 ± 0.05 mg; however, significant analgesic variability was noted.[97] A systematic review recommended 0.1 mg as the optimal intrathecal morphine dose for caesarean delivery analgesia.[4] The use of multimodal adjuvant analgesia including NSAIDs postoperatively may further reduce dose requirements. Cardoso et al.[98] found that 0.025 mg of intrathecal morphine when combined with systemic diclofenac was as effective as 0.05 or 0.1 mg.
A number of dose-response studies with intrathecal morphine have been conducted in non-obstetric surgical populations. Sarma and Bostrom[99] examined the dose-response of intrathecal morphine (0, 0.1, 0.3 and 0.5 mg) in patients undergoing total abdominal hysterectomy under general anaesthesia. The ‘analgesic ceiling’ in this study was 0.3 mg. Another dose-response study observed pain relief and adverse effects of intrathecal morphine doses (0, 0.04, 0.06, 0.08, 0.1, 0.12, 0.15 and 0.2 mg) in patients undergoing cholecystectomy with spinal anaesthesia.[100] Optimal analgesia without respiratory depression was obtained in the 0.06–0.12 mg dose range. The incidence of respiratory depression was greater with doses of 0.15 and 0.2 mg. Hassett et al.[101] examined the analgesic efficacy and adverse effect profile of 0.1, 0.2 and 0.3 mg intrathecal morphine in patients undergoing elective total knee replacement. They found morphine 0.2 mg to be the optimal analgesic dose, but observed no differences between adverse effects or respiratory depression amongst the doses studied. Slappendel et al.[102] studied various intrathecal morphine doses (0.025, 0.05, 0.1 or 0.2 mg) for total hip surgery and concluded that 0.1 mg was the optimal analgesic dose. The incidence of pruritus and requirement for antipruritic medication was dose-related, although there were no reports of respiratory depression or differences in oxygen desaturation among the different groups within this study. In a study of patients undergoing lumbar fusion randomized to receive morphine (0.2, 0.3 or 0.4 mg) injected into the dural sac under direct visualization, pain scores were better with 0.3 and 0.4 mg doses.[103] However, respiratory rate was lower and the partial pressure of arterial carbon dioxide (PaCO2) was consistently higher in patients receiving the 0.4 mg dose.
The effects of increasing intrathecal morphine doses (0.2, 0.4 and 0.6 mg) were assessed in non-surgical healthy, young, adult male volunteers.[23] The authors reported dose-related respiratory depression with significant decreases in SpO2 (measured by pulse oximetry), the need for supplemental oxygen, and increased peak mean PaCO2. The PaCO2 peaks occurred 6.5–7.5 hours after intrathecal morphine administration. A meta-analysis of 28 studies (n = 790) determined adverse effects of intrathecal morphine in patients undergoing surgery with spinal anaesthesia.[51] The authors found that intrathecal morphine resulted in an increased incidence of adverse effects (pruritus, nausea and vomiting) compared with patients not receiving intrathecal morphine. The incidence of pruritus was found to be dose-dependent. Higher doses (≥0.3 mg) of intrathecal morphine were associated with a greater number of episodes of respiratory depression, 9% (7/80) compared with lower doses 1% (2/247), but the difference in incidence was not statistically significant.
6.2 Epidural Morphine Doses
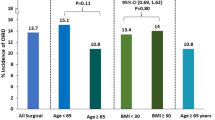
The dose-effect relationship of epidural morphine has also been studied. A dose-response study by Palmer et al.[104] determined that the optimal post-caesarean analgesic dose of epidural morphine was 3.75 mg. In the dose range studied (0, 1.25, 2.5, 3.75 and 5 mg), increasing the dose beyond this ‘analgesic ceiling’ did not improve postoperative analgesia or reduce opioid use (figure 1). A 3 mg dose of epidural morphine was similarly recommended by Fuller et al.[71] based on a large retrospective post-caesarean study. Chumpathong et al.[105] found similar post-caesarean analgesia and adverse effects with 2.5, 3 and 4 mg doses of epidural morphine. A study by Rosen et al.[106] demonstrated that 2 mg did not provide adequate post-caesarean analgesia compared with 5 and 7.5 mg of epidural morphine.
Fig. 1 Dose-response relationship of intrathecal morphine for post-caesarean analgesia. = patient-controlled analgesia [reproduced from Palmer et al.,[104] with permission].
The analgesic and adverse effects of 1, 2, 3, 4 and 5 mg epidural morphine were examined in patients undergoing orthopaedic procedures.[107] Authors recommended 3 mg of epidural morphine as the optimal dose. Patients receiving ≥2 mg required less postoperative analgesia and experienced less postoperative pain, but the 5 mg dose produced mild respiratory depression (mean PaCO2 5 mm Hg greater than control group). A dose-dependent increase in pruritus and urinary catheterization was also observed. Rawal and Wattwil[63] performed a dose-response study in healthy volunteers administering epidural morphine doses of 2, 4 or 10 mg, and in the clinical part of the study administering epidural morphine 4 mg in surgical patients undergoing cholecystectomy. The authors found a dose-related depression in ventilatory drive (reduction in minute ventilation and increase in partial pressure of end tidal carbon dioxide [PETCO2]) in the healthy volunteers. PETCO2 levels were higher and remained elevated longer in surgical patients than in volunteers given the same 4 mg dose. An infusion of naloxone (5 μg/kg/hour) was also found to prevent respiratory depression in the volunteers.
6.3 Optimal Intrathecal and Epidural Morphine Dose Recommendations intheSurgical Setting
Dose-response studies show that neuraxial morphine appears to have an analgesic efficacy ‘ceiling’. The optimal ‘single-shot’ intrathecal dose appears to be 0.075–0.15 mg and the ideal ‘single-shot’ epidural morphine dose is 2.5–3.75 mg. Analgesic efficacy studies have not been adequately powered to show differences in the incidence of clinically significant respiratory depression. However, opioid-related adverse effects, particularly pruritus, have been found to be dose-related in a number of studies.
7. Drugs to Minimize Opioid-Related Respiratory Depression
Opioid antagonists such as naloxone are available clinically to treat opioid-induced respiratory depression.[108] However, their use may lead to a loss in analgesia resulting in difficult pain management.[109] Moreover, the potential for re-narcotization exists due to the relatively short elimination half-life of naloxone. A number of adverse effects secondary to reversal of analgesia and release of catecholamines by a central mechanism have been described following the use of opioid antagonists such as naloxone. These adverse effects include pain, psychological stimulation, and sympathomimetic responses including pulmonary oedema in severe circumstances.[110] A continuous naloxone infusion of 3–4 μg/kg/hour for up to 10 hours has been recommended by some to avoid such adverse effects,[111] whereas others recommend naloxone infusions with intermittent supplemental dose titration with repeated small boluses of 0.8 μg/kg until adequate reversal of respiratory depression is achieved.[112]
There is much interest in developing therapeutic interventions that reverse respiratory depression secondary to opioids whilst preserving their analgesic effects. Researchers have recently focused on using non-opioid drugs such as serotonin receptor agonists, ampakines (α-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid [AMPA] receptor modulators) and minocycline. A number of studies examining these newer drugs have proven effective in animal models;[113,114] however, few have thus far shown to be clinically beneficial. Glutamate-mediated neurotransmission via AMPA receptors at the preBötzinger complex is crucial part of the generation of rhythmic respiratory pattern.[115–117] In 2010, Oertel et al.[118] studied ampakine CX717 in 16 healthy male volunteers in whom intravenous alfentanil at a target concentration of 100 ng/mL was used to induce respiratory depression. A decrease in respiratory rate was noted to be 3 ± 33% in those receiving a 1.5 g oral dose of CX717 prior to the alfentanil compared with 26 ± 28% in the placebo group receiving no ampakine. Ventilator response to hypercapnic challenge and blood oxygenation were also shown to be less significantly affected with CX717 compared with the placebo group. Importantly, the authors observed that the analgesic effects of alfentanil were unchanged by the CX717. The mechanism of action is thought to be an AMPA receptor neuronal excitation by the CX717, which counteracts the depression caused by the μ-opioid receptors at the preBötzinger complex.[119] Although early in its development, there is considerable potential for the use of this drug in patients receiving neuraxial morphine.
Repinotan is a selective serotonin (5HT)1A receptor agonist, which has been investigated in humans for its neuroprotective effects following stroke[120] and traumatic brain injury.[121] Guenther and colleagues[122] demonstrated spontaneous breathing in anaesthetized rats following morphine-induced respiratory depression. The dose-response curve of spontaneous breathing following morphine-induced ventilatory depression appears to be ‘bell shaped’ after 5HT1A receptor stimulation, which suggests diminished stimulatory effects at higher concentrations.[123] The effects on opioid-induced respiratory depression and nociception are yet to be established in humans.
Microglial inhibitors have shown potential to enhance the analgesic efficacy of morphine. Minocycline, a tetracycline derivative and microglial inhibitor,[124] improved analgesia and reduced opioid-induced respiratory depression in rats.[114] These findings may stimulate future research of this drug in a clinical setting. Sodium/proton exchanger type 3 (NHE3) inhibitors that act centrally on respiratory pathways are another class of drugs that warrant further study.[125,126]
8. Conclusion
Neuraxial morphine has contributed significantly to improve analgesia in many surgical settings. The analgesic benefits related to neuraxial morphine administration far outweigh the risks associated with the rare incidence of respiratory depression. In addition, the risk of respiratory depression following neuraxial morphine is not greater than that following systemic morphine administration.[66,89] Neuraxial morphine appears to have an analgesic efficacy ‘ceiling’ and utilizing larger doses may increase adverse effects without necessarily improving analgesia. The optimal intrathecal dose appears to be 0.075–0.15 mg and the ideal epidural morphine dose is 2.5–3.75 mg. There are a number of novel non-opioid drugs such as serotonin receptor agonists, ampakines and minocycline being developed that may reduce the risk of opioid-induced respiratory depression in the future.
References
Nishio Y, Sinatra RS, Kitahata LM, et al. Spinal cord distribution of 3H-morphine after intrathecal administration: relationship to analgesia. Anesth Analg 1989 Sep; 69(3): 323–7
Wang JK, Nauss LA, Thomas JE. Pain relief by intrathecally applied morphine in man. Anesthesiology 1979 Feb; 50(2): 149–51
Behar M, Magora F, Olshwang D, et al. Epidural morphine in treatment of pain. Lancet 1979 Mar 10; I(8115): 527–9
Dahl JB, Jeppesen IS, Jorgensen H, et al. Intraoperative and postoperative analgesic efficacy and adverse effects of intrathecal opioids in patients undergoing cesarean section with spinal anesthesia: a qualitative and quantitative systematic review of randomized controlled trials. Anesthesiology 1999 Dec; 91(6): 1919–27
Mathews ET, Abrams LD. Intrathecal morphine in open heart surgery [letter]. Lancet 1980; II: 527–8
Cohen SE, Woods WA. The role of epidural morphine in the postcesarean patient: efficacy and effects on bonding. Anesthesiology 1983 Jun; 58(6): 500–4
Rosaeg OP, Lui AC, Cicutti NJ, et al. Peri-operative multimodal pain therapy for caesarean section: analgesia and fitness for discharge. Can J Anaesth 1997 Aug; 44(8): 803–9
Cousins MJ, Mather LE, Glynn CJ, et al. Selective spinal analgesia. Lancet 1979 May 26; I(8126): 1141–2
Brill S, Gurman GM, Fisher A. A history of neuraxial administration of local analgesics and opioids. Eur J Anaesthesiol 2003 Sep; 20(9): 682–9
Glynn CJ, Mather LE, Cousins MJ, et al. Spinal narcotics and respiratory depression. Lancet 1979 Aug 18; 2(8138): 356–7
Liolios A, Andersen FH. Selective spinal analgesia [letter]. Lancet 1979 Aug 18; II(8138): 357
Scott DB, McClure J. Selective epidural analgesia. Lancet 1979 Jun 30; I(8131): 1410–1
Cranshaw J, Gupta KJ, Cook TM. Litigation related to drug errors in anaesthesia: an analysis of claims against the NHS in England 1995–2007. Anaesthesia 2009 Dec; 64(12): 1317–23
Stoelting RK. Intrathecal morphine: an underused combination for postoperative pain management. Anesth Analg 1989 Jun; 68(6): 707–9
Gustafsson LL, Schildt B, Jacobsen K. Adverse effects of extradural and intrathecal opiates: report of a nationwide survey in Sweden. Br J Anaesth 1982 May; 54(5): 479–86
Stenseth R, Sellevold O, Breivik H. Epidural morphine for postoperative pain: experience with 1085 patients. Acta Anaesthesiol Scand 1985 Jan; 29(1): 148–56
Kafer ER, Brown JT, Scott D, et al. Biphasic depression of ventilatory responses to CO2 following epidural morphine. Anesthesiology 1983 May; 58(5): 418–27
Koren G, Sandler AN, Klein J, et al. Relationship between the pharmacokinetics and the analgesic and respiratory pharmacodynamics of epidural sufentanil. Clin Pharmacol Ther 1989 Oct; 46(4): 458–62
Brockway MS, Noble DW, Sharwood-Smith GH, et al. Profound respiratory depression after extradural fentanyl. Br J Anaesth 1990 Feb; 64(2): 243–5
Stienstra R, Pannekoek BJ. Respiratory arrest following extradural sufentanil. Anaesthesia 1993 Dec; 48(12): 1055–6
Whiting WC, Sandler AN, Lau LC, et al. Analgesic and respiratory effects of epidural sufentanil in patients following thoracotomy. Anesthesiology 1988 Jul; 69(1): 36–43
Negre I, Gueneron JP, Ecoffey C, et al. Ventilatory response to carbon dioxide after intramuscular and epidural fentanyl. Anesth Analg 1987 Aug; 66(8): 707–10
Bailey PL, Rhondeau S, Schafer PG, et al. Dose-response pharmacology of intrathecal morphine in human volunteers. Anesthesiology 1993 Jul; 79(1): 49–59; discussion 25A
Abboud TK, Moore M, Zhu J, et al. Epidural butorphanol or morphine for the relief of post-cesarean section pain: ventilatory responses to carbon dioxide. Anesth Analg 1987 Sep; 66(9): 887–93
Hurle MA, Mediavilla A, Florez J. Morphine, pentobarbital and naloxone in the ventral medullary chemosensitive areas: differential respiratory and cardiovascular effects. J Pharmacol Exp Ther 1982 Mar; 220(3): 642–7
Pokorski M, Grieb P, Wideman J. Opiate system influences central respiratory chemosensors. Brain Res 1981 Apr 27; 211(1): 221–6
Mueller RA, Lundberg DB, Breese GR, et al. The neuropharmacology of respiratory control. Pharmacol Rev 1982 Sep; 34(3): 255–85
Yaksh TL. Spinal opiate analgesia: characteristics and principles of action. Pain 1981 Dec; 11(3): 293–346
Denavit-Saubie M, Champagnat J, Zieglgansberger W. Effects of opiates and methionine-enkephalin on pontine and bulbar respiratory neurones of the cat. Brain Res 1978 Oct 20; 155(1): 55–67
Shook JE, Watkins WD, Camporesi EM. Differential roles of opioid receptors in respiration, respiratory disease, and opiate-induced respiratory depression. Am Rev Respir Dis 1990 Oct; 142(4): 895–909
Morin-Surun MP, Boudinot E, Gacel G, et al. Different effects of mu and delta opiate agonists on respiration. Eur J Pharmacol 1984 Feb 17; 98(2): 235–40
Montandon G, Qin W, Liu H, et al. PreBötzinger complex neurokinin-1 receptor-expressing neurons mediate opioid-induced respiratory depression. J Neurosci 2011 Jan 26; 31(4): 1292–301
Bernards CM, Shen DD, Sterling ES, et al. Epidural, cerebrospinal fluid, and plasma pharmacokinetics of epidural opioids (part 1): differences among opioids. Anesthesiology 2003 Aug; 99(2): 455–65
Youngstrom PC, Cowan RI, Sutheimer C, et al. Pain relief and plasma concentrations from epidural and intramuscular morphine in post-cesarean patients. Anesthesiology 1982 Nov; 57(5): 404–9
Weddel SJ, Ritter RR. Serum levels following epidural administration of morphine and correlation with relief of postsurgical pain. Anesthesiology 1981 Mar; 54(3): 210–4
Moulin DE, Inturrisi CE, Foley KM. Cerebrospinal fluid pharmacokinetics of intrathecal morphine sulfate and D-Ala2-D-Leu5-enkephalin. Ann Neurol 1986 Aug; 20(2): 218–22
Cousins MJ, Mather LE. Intrathecal and epidural administration of opioids. Anesthesiology 1984 Sep; 61(3): 276–310
Gourlay GK, Cherry DA, Plummer JL, et al. The influence of drug polarity on the absorption of opioid drugs into CSF and subsequent cephalad migration following lumbar epidural administration: application to morphine and pethidine. Pain 1987 Dec; 31(3): 297–305
Chauvin M, Samii K, Schermann JM, et al. Plasma pharmacokinetics of morphine after i.m., extradural and intrathecal administration. Br J Anaesth 1982 Aug; 54(8): 843–7
Chiro G. Observations on the circulation of the cerebrospinal fluid. Acta Radiol Diagn (Stockh) 1966; 5: 988–1002
Caute B, Monsarrat B, Gouarderes C, et al. CSF morphine levels after lumbar intrathecal administration of isobaric and hyperbaric solutions for cancer pain. Pain 1988 Feb; 32(2): 141–6
Sandouk P, Scherrmann JM, Chauvin M. Rate-limiting diffusion processes following intrathecal administration of morphine. Eur J Clin Pharmacol 1986; 30(5): 575–9
Hanna MH, Peat SJ, Woodham M, et al. Analgesic efficacy and CSF pharmacokinetics of intrathecal morphine-6-glucuronide: comparison with morphine. Br J Anaesth 1990 May 1; 64(5): 547–50
Davies GK, Tolhurst-Cleaver CL, James TL. Respiratory depression after intrathecal narcotics. Anaesthesia 1980 Nov; 35(11): 1080–3
Nordberg G, Hedner T, Mellstrand T, et al. Pharmacokinetic aspects of intrathecal morphine analgesia. Anesthesiology 1984 May; 60(5): 448–54
Sjostrom S, Tamsen A, Persson MP, et al. Pharmacokinetics of intrathecal morphine and meperidine in humans. Anesthesiology 1987 Dec; 67(6): 889–95
Ionescu TI, Taverne RH, Drost RH, et al. Epidural morphine anesthesia for abdominal aortic surgery: pharmacokinetics. Reg Anesth 1989 May–Jun; 14(3): 107–14
Gourlay GK, Cherry DA, Cousins MJ. Cephalad migration of morphine in CSF following lumbar epidural administration in patients with cancer pain. Pain 1985 Dec; 23(4): 317–26
Bellanca L, Latteri MT, Latteri S, et al. Plasma and CSF morphine concentrations after i.m. and epidural administration. Pharmacol Res Commun 1985; 17(2): 189–96
Sabbe MB, Grafe MR, Mjanger E, et al. Spinal delivery of sufentanil, alfentanil, and morphine in dogs: physiologic and toxicologic investigations. Anesthesiology 1994; 81(4): 899–920
Gehling M, Tryba M. Risks and side-effects of intrathecal morphine combined with spinal anaesthesia: a meta-analysis. Anaesthesia 2009 Jun; 64(6): 643–51
Horlocker TT, Burton AW, Connis RT, et al. Practice guidelines for the prevention, detection, and management of respiratory depression associated with neuraxial opioid administration. Anesthesiology 2009 Feb; 110(2): 218–30
Weinger M. Dangers of postoperative opioids. APSF Newsletter 2007; 21: 61–8
Chaney MA. Side effects of intrathecal and epidural opioids. Can J Anaesth 1995 Oct; 42(10): 891–903
Horlocker TS. Practice guidelines for the prevention, detection and management of respiratory depressioan associated with neuraxial opioid administration: preliminary report by ASA task fore on neuraxial anesthesia. ASA Newsletter 2007; 71: 24–6
Pleym H, Spigset O, Kharasch ED, et al. Gender differences in drug effects: implications for anesthesiologists. Acta Anaesthesiol Scand 2003; 47(3): 241–59
Abouleish E, Rawal N, Rashad MN. The addition of 0.2 mg subarachnoid morphine to hyperbaric bupivacaine for cesarean delivery: a prospective study of 856 cases. Reg Anesth 1991 May–Jun; 16(3): 137–40
Romberg RR, Olofsen E, Bijl H, et al. Polymorphism of mu-opioid receptor gene (OPRM1: c.118A>G) does not protect against opioid-induced respiratory depression despite reduced analgesic response. Anesthesiology 2005 Mar; 102(3): 522–30
Robins K, Lyons G. Opioid-related narcosis in a woman with myopathy receiving magnesium. Int J Obstet Anesth 2007 Oct; 16(4): 367–9
Skatrud JB, Dempsey JA, Kaiser DG. Ventilatory response to medroxyprogesterone acetate in normal subjects: time course and mechanism. J Appl Physiol 1978 Jun; 44(6): 393–44
Hughes SC. Respiratory depression following intraspinal narcotics: expect it! Int J Obstet Anesth 1997 Jul; 6(3): 145–6
Ko S, Goldstein DH, VanDenKerkhof EG. Definitions of ‘respiratory depression’ with intrathecal morphine postoperative analgesia: a review of the literature. Can J Anaesth 2003 Aug–Sep; 50(7): 679–88
Rawal N, Wattwil M. Respiratory depression after epidural morphine: an experimental and clinical study. Anesth Analg 1984 Jan; 63(1): 8–14
Etches RC, Sandler AN, Daley MD. Respiratory depression and spinal opioids. Can J Anaesth 1989 Mar; 36(2): 165–85
Kato R, Shimamoto H, Terui K, et al. Delayed respiratory depression associated with 0.15mg intrathecal morphine for cesarean section: a review of 1915 cases. J Anesth 2008; 22(2): 112–6
Shapiro A, Zohar E, Zaslansky R, et al. The frequency and timing of respiratory depression in 1524 postoperative patients treated with systemic or neuraxial morphine. J Clin Anesth 2005 Nov; 17(7): 537–42
Flisberg P, Rudin A, Linner R, et al. Pain relief and safety after major surgery: a prospective study of epidural and intravenous analgesia in 2696 patients. Acta Anaesthesiol Scand 2003 Apr; 47(4): 457–65
Gwirtz KH, Young JV, Byers RS, et al. The safety and efficacy of intrathecal opioid analgesia for acute postoperative pain: seven years’ experience with 5969 surgical patients at Indiana University Hospital. Anesth Analg 1999 Mar; 88(3): 599–604
Tsui SL, Irwin MG, Wong CM, et al. An audit of the safety of an acute pain service. Anaesthesia 1997 Nov; 52(11): 1042–7
Rygnestad T, Borchgrevink PC, Eide E. Postoperative epidural infusion of morphine and bupivacaine is safe on surgical wards: organisation of the treatment, effects and side-effects in 2000 consecutive patients. Acta Anaesthesiol Scand 1997 Aug; 41(7): 868–76
Fuller JG, McMorland GH, Douglas MJ, et al. Epidural morphine for analgesia after caesarean section: a report of 4880 patients. Can J Anaesth 1990 Sep; 37(6): 636–40
Leicht CH, Hughes SC, Dailey PA, et al. Epidural morphine sulfate for analgesia after cesarean section: a prospective report of 1000 patients [abstract]. Anesthesiology 1986; 65: A366
Kotelko DM, Dailey PA, Shnider SM, et al. Epidural morphine analgesia after cesarean delivery. Obstet Gynecol 1984 Mar; 63(3): 409–13
Meylan N, Elia N, Lysakowski C, et al. Benefit and risk of intrathecal morphine without local anaesthetic in patients undergoing major surgery: meta-analysis of randomized trials. Br J Anaesth 2009 Feb; 102(2): 156–67
Frassanito L, Vergari A, Zanghi F, et al. Post-operative analgesia following total knee arthroplasty: comparison of low-dose intrathecal morphine and single-shot ultrasound-guided femoral nerve block: a randomized, single blinded, controlled study. Eur Rev Med Pharmacol Sci 2010 Jul; 14(7): 589–96
Duman A, Apiliogullari S, Balasar M, et al. Comparison of 50microg and 25 microg doses of intrathecal morphine on postoperative analgesic requirements in patients undergoing transurethral resection of the prostate with intrathecal anesthesia. J Clin Anesth 2010 Aug; 22(5): 329–33
Yamashita K, Fukusaki M, Ando Y, et al. Postoperative analgesia with minidose intrathecal morphine for bipolar hip prosthesis in extremely elderly patients. J Anesth 2009; 23(4): 504–7
Draisci G, Frassanito L, Pinto R, et al. Safety and effectiveness of coadministration of intrathecal sufentanil and morphine in hyperbaric bupivacaine-based spinal anesthesia for cesarean section. J Opioid Manag 2009 Jul–Aug; 5(4): 197–202
Andrieu G, Roth B, Ousmane L, et al. The efficacy of intrathecal morphine with or without clonidine for postoperative analgesia after radical prostatectomy. Anesth Analg 2009 Jun; 108(6): 1954–7
Massicotte L, Chalaoui KD, Beaulieu D, et al. Comparison of spinal anesthesia with general anesthesia on morphine requirement after abdominal hysterectomy. Acta Anaesthesiol Scand 2009 May; 53(5): 641–7
Ko JS, Choi SJ, Gwak MS, et al. Intrathecal morphine combined with intravenous patient-controlled analgesia is an effective and safe method for immediate postoperative pain control in live liver donors. Liver Transpl 2009 Apr; 15(4): 381–9
Gehling MH, Luesebrink T, Kulka PJ, et al. The effective duration of analgesia after intrathecal morphine in patients without additional opioid analgesia: a randomized double-blind multicentre study on orthopaedic patients. Eur J Anaesthesiol 2009 Aug; 26(8): 683–8
Ziegeler S, Fritsch E, Bauer C, et al. Therapeutic effect of intrathecal morphine after posterior lumbar interbody fusion surgery: a prospective, double-blind, randomized study. Spine (Phila Pa 1976 2008 Oct 15; 33(22): 2379–86
Dualé C, Frey C, Bolandard F, et al. Epidural versus intrathecal morphine for postoperative analgesia after Caesarean section. Br J Anaesth 2003 Nov; 91(5): 690–4
Techanivate A, Kiatgungwanglia P, Yingsakmongkol W. Spinal morphine for post-operative analgesia after lumbar laminectomy with fusion. J Med Assoc Thai 2003 Mar; 86(3): 262–9
Devys JM, Mora A, Plaud B, et al. Intrathecal+PCA morphine improves analgesia during the first 24 hr after major abdominal surgery compared to PCA alone. Can J Anaesth 2003 Apr; 50(4): 355–61
Fournier R, Van Gessel E, Macksay M, et al. Onset and offset of intrathecal morphine versus nalbuphine for postoperative pain relief after total hip replacement. Acta Anaesthesiol Scand 2000 Sep; 44(8): 940–5
Culebras X, Gaggero G, Zatloukal J, et al. Advantages of intrathecal nalbuphine, compared with intrathecal morphine, after cesarean delivery: an evaluation of postoperative analgesia and adverse effects. Anesth Analg 2000 Sep; 91(3): 601–5
Cashman JN, Dolin SJ. Respiratory and haemodynamic effects of acute postoperative pain management: evidence from published data. Br J Anaesth 2004 Aug; 93(2): 212–23
Sarvela J, Halonen P, Soikkeli A, et al. A double-blinded, randomized comparison of intrathecal and epidural morphine for elective cesarean delivery. Anesth Analg 2002 Aug; 95(2): 436–40
Ng K, Parsons J, Cyna AM, et al. Spinal versus epidural anaesthesia for caesarean section. Cochrane Database Syst Rev 2004; (2): CD003765
Chadwick HS, Bernards CM, Kovarik DW, et al. Subdural injection of morphine for analgesia following cesarean section: a report of three cases. Anesthesiology 1992 Sep; 77(3): 590–4
Palmer CM, Emerson S, Volgoropolous D, et al. Dose-response relationship of intrathecal morphine for post-cesarean analgesia. Anesthesiology 1999 Feb; 90(2): 437–44
Uchiyama A, Nakano S, Ueyama H, et al. Low dose intrathecal morphine and pain relief following caesarean section. Int J Obstet Anesth 1994 Apr; 3(2): 87–91
Milner AR, Bogod DG, Harwood RJ. Intrathecal administration of morphine for elective Caesarean section: a comparison between 0.1 mg and 0.2 mg. Anaesthesia 1996 Sep; 51(9): 871–3
Yang T, Breen TW, Archer D, et al. Comparison of 0.25 mg and 0.1 mg intrathecal morphine for analgesia after Cesarean section. Can J Anaesth 1999 Sep; 46(9): 856–60
Gerancher JC, Floyd H, Eisenach J. Determination of an effective dose of intrathecal morphine for pain relief after cesarean delivery. Anesth Analg 1999 Feb; 88(2): 346–51
Cardoso MM, Carvalho JC, Amaro AR, et al. Small doses of intrathecal morphine combined with systemic diclofenac for postoperative pain control after cesarean delivery. Anesth Analg 1998 Mar; 86(3): 538–41
Sarma VJ, Bostrom UV. Intrathecal morphine for the relief of post-hysterectomy pain: a double-blind, dose-response study. Acta Anaesthesiol Scand 1993 Feb; 37(2): 223–7
Yamaguchi H, Watanabe S, Motokawa K, et al. Intrathecal morphine dose-response data for pain relief after cholecystectomy. Anesth Analg 1990 Feb; 70(2): 168–71
Hassett P, Ansari B, Gnanamoorthy P, et al. Determination of the efficacy and side-effect profile of lower doses of intrathecal morphine in patients undergoing total knee arthroplasty. BMC Anesthesiol 2008; 8: 5
Slappendel R, Weber EW, Dirksen R, et al. Optimization of the dose of intrathecal morphine in total hip surgery: a dose-finding study. Anesth Analg 1999 Apr; 88(4): 822–6
Boezaart AP, Eksteen JA, Spuy GV, et al. Intrathecal morphine: double-blind evaluation of optimal dosage for analgesia after major lumbar spinal surgery. Spine (Phila Pa 1976) 1999 Jun 1; 24(11): 1131–7
Palmer CM, Nogami WM, Van Maren G, et al. Postcesarean epidural morphine: a dose-response study. Anesth Analg 2000 Apr; 90(4): 887–91
Chumpathong S, Santawat U, Saunya P, et al. Comparison of different doses of epidural morphine for pain relief following cesarean section. J Med Assoc Thai 2002 Sep; 85 Suppl. 3: S956–62
Rosen MA, Hughes SC, Shnider SM, et al. Epidural morphine for the relief of postoperative pain after cesarean delivery. Anesth Analg 1983 Jul; 62(7): 666–72
Lanz E, Kehrberger E, Theiss D. Epidural morphine: a clinical double-blind study of dosage. Anesth Analg 1985 Aug; 64(8): 786–91
Longnecker DE, Grazis PA, Eggers Jr GW. Naloxone for antagonism of morphine-induced respiratory depression. Anesth Analg 1973 May–Jun; 52(3): 447–53
Cepeda MS, Africano JM, Manrique AM, et al. The combination of low dose of naloxone and morphine in PCA does not decrease opioid requirements in the postoperative period. Pain 2002 Mar; 96(1–2): 73–9
Taff RH. Pulmonary edema following naloxone administration in a patient without heart disease. Anesthesiology 1983 Dec; 59(6): 576–7
Johnstone RE, Jobes DR, Kennell EM, et al. Reversal of morphine anesthesia with naloxone. Anesthesiology 1974 Oct; 41(4): 361–7
Takahashi M, Sugiyama K, Hori M, et al. Naloxone reversal of opioid anesthesia revisited: clinical evaluation and plasma concentration analysis of continuous naloxone infusion after anesthesia with high-dose fentanyl. J Anesth 2004; 18(1): 1–8
Manzke T, Guenther U, Ponimaskin EG, et al. 5-HT4(a) receptors avert opioid-induced breathing depression without loss of analgesia. Science 2003 Jul 11; 301(5630): 226–9
Hutchinson MR, Northcutt AL, Chao LW, et al. Minocycline suppresses morphine-induced respiratory depression, suppresses morphine-induced reward, and enhances systemic morphine-induced analgesia. Brain Behav Immun 2008 Nov; 22(8): 1248–56
Greer JJ, Smith JC, Feldman JL. Role of excitatory amino acids in the generation and transmission of respiratory drive in neonatal rat. J Physiol 1991; 437: 727–49
Funk GD, Smith JC, Feldman JL. Generation and transmission of respiratory oscillations in medullary slices: role of excitatory amino acids. JNeurophysiol 1993; 70(4): 1497–515
Pace RW, Mackay DD, Feldman JL, et al. Inspiratory bursts in the preBötzinger complex depend on a calcium-activated non-specific cation current linked to glutamate receptors in neonatal mice. J Physiol 2007 Jul 1; 582(1): 113–25
Oertel BG, Felden L, Tran PV, et al. Selective antagonism of opioid-induced ventilatory depression by an ampakine molecule in humans without loss of opioid analgesia. Clin Pharmacol Ther 2010 Feb; 87(2): 204–11
Greer JJ, Ren J. Ampakine therapy to counter fentanyl-induced respiratory depression. Respiratory Physiol Neurobiol 2009; 168(1–2): 153–7
Teal P, Davis S, Hacke W, et al. A randomized, double-blind, placebo-controlled trial to evaluate the efficacy, safety, tolerability, and pharmacokinetic/pharmacodynamic effects of a targeted exposure of intravenous repinotan in patients with acute ischemic stroke: modified Randomized Exposure Controlled Trial (mRECT). Stroke 2009 Nov; 40(11): 3518–25
Ohman J, Braakman R, Legout V. Repinotan (BAY x 3702): a 5HT1A agonist in traumatically brain injured patients. J Neurotrauma 2001 Dec; 18(12): 1313–21
Guenther U, Wrigge H, Theuerkauf N, et al. Repinotan, a selective 5-HT1A-R-agonist, antagonizes morphine-induced ventilatory depression in anesthetized rats. Anesth Analg 2010 Oct; 111(4): 901–7
Calabrese EJ, Baldwin LA. U-shaped dose-responses in biology, toxicology, and public health. Annu Rev Public Health 2001; 22: 15–33
Cui Y, Liao XX, Liu W, et al. A novel role of minocycline: attenuating morphine antinociceptive tolerance by inhibition of p38 MAPK in the activated spinal microglia. Brain Behav Immun 2008 Jan; 22(1): 114–23
Kiwull-Schone H, Kiwull P, Frede S, et al. Role of brain-stem sodium/proton exchanger 3 for breathing control during chronic acid base imbalance. Am J Respir Crit Care Med 2007 Sep 1; 176(5): 513–9
Wiemann M, Piechatzek L, Gopelt K, et al. The NHE3 inhibitor AVE1599 stimulates phrenic nerve activity in the rat. J Physiol Pharmacol 2008 Mar; 59(1): 27–36
Acknowledgements
No sources of funding were used in the preparation of this review. Brendan Carvalho reports receiving funding from EKR Therapeutics as principal investigator for study conduct (DepoDur™), and Epimed International, Inc. for research efforts. Drs Sultan and Gutierrez report no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sultan, P., Gutierrez, M.C. & Carvalho, B. Neuraxial Morphine and Respiratory Depression. Drugs 71, 1807–1819 (2011). https://doi.org/10.2165/11596250-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11596250-000000000-00000