Summary
Abstract
Everolimus (Certican®) is an orally administered mammalian target of rapamycin inhibitor (proliferation signal inhibitor) derived from sirolimus (rapamycin), which is used as part of immunosuppressant therapy in kidney and heart transplantation. When evaluated as part of triple therapy with ciclosporin and corticosteroids, everolimus showed equivalent efficacy to mycophenolate mofetil after renal transplantation, and superiority to azathioprine in cardiac transplant recipients, in terms of reducing efficacy failure after transplantation. Everolimus potentiates ciclosporin-associated nephrotoxicity, and it is recommended that concentration-controlled everolimus is used with reduced-dosage ciclosporin in order to limit renal toxicity while retaining immunosuppressive efficacy. Ongoing trials with everolimus, such as the evaluation of ciclosporin-withdrawal strategies, should help clarify its optimal usage. The use of everolimus may be associated with reduced rates of cytomegalovirus (CMV) infection and of cardiac allograft vasculopathy. Available data suggest that everolimus may be cost-neutral for healthcare providers.
Pharmacological Properties
Everolimus inhibits growth factor-stimulated cell proliferation of haematopoietic and nonhaematopoietic cells through the formation of a complex with FK506 (tacrolimus)-binding protein 12 (FKBP12). This complex binds to FKB12-rapamycin-associated protein, blocking its activity, which includes the phosphorylation of p70 S6 kinase, and subsequent protein synthesis.
Exposure-response data show a link between trough blood concentrations of everolimus and risk of acute allograft rejection in renal transplant patients, and the drug has been shown to inhibit vascular remodelling in preclinical studies and fibroblast proliferation in tissue from lung transplant patients. Synergism of everolimus with other agents, including ciclosporin, fingolimod and mycophenolate mofetil, has been noted in preclinical studies. There is no evidence of antagonism between everolimus and tacrolimus in terms of lymphocyte proliferation.
Everolimus displays dose-proportional pharmacokinetics, with rapid absorption leading to peak blood concentrations being attained within 1–2 hours of an oral dose. Steady state is generally achieved by day 4. More than 75% of the drug is sequestered into red blood cells; 75% of the fraction in plasma is bound to plasma proteins. Metabolism is chiefly via hepatic cytochrome P450 (CYP) enzymes 3A4, 3A5 and 2C8, and approximately 98% is excreted in bile as metabolites. Bioavailability is affected markedly by the presence of food, and apparent clearance is reduced in patients with moderate hepatic impairment. The elimination half-life of everolimus is 24–35 hours. Everolimus and ciclosporin are both metabolised by the CYP3A isoenzyme system, and their concomitant administration increases everolimus exposure by 2- to 3-fold. Drugs that are likely to affect the clearance of everolimus through induction or inhibition of CYP3A enzymes include erythromycin, azithromycin, ketoconazole, itraconozole and rifampicin.
Therapeutic Efficacy
Oral everolimus 1.5 or 3 mg/day, in combination with full-dosage ciclosporin microemulsion and corticosteroids, has been shown to be as effective as mycophenolate mofetil 2 g/day in the prevention of efficacy failure after kidney transplantation in two major randomised, international trials in a total of 1171 patients. Both trials ran for 3 years and were double-blind in the first year. The primary endpoint, ‘efficacy failure’ at 6 or 36 months, was a composite of biopsy-proven acute rejection (BPAR), graft loss, death or loss to follow-up. In one trial, graft survival was significantly better in the everolimus 1.5 mg/day group than in the 3 mg/day group after 36 months. Rates of mortality were similar across all groups, with >90% of patients surviving to 36 months in both studies.
Full dosages of ciclosporin were used initially in both trials, although a subsequent protocol amendment reduced ciclosporin exposure because of concerns over increases in circulating creatinine levels in the everolimus-plusciclosporin groups, which suggested that everolimus potentiated ciclosporin-associated nephrotoxicity. After the introduction of the amendment, renal function stabilised in the everolimus groups, but serum creatinine values remained higher in these groups than among mycophenolate mofetil recipients.
The same dosages of everolimus, adjusted to ensure everolimus trough blood concentrations (Cmin) of ≥3 ng/mL, were given with reduced dosages of ciclosporin in two open-label studies in a total of 493 patients. Induction therapy with basiliximab was also used in one of these trials. Rates of efficacy failure over 24 months were similar between groups overall, and BPAR was less common in patients treated with everolimus plus reduced-dosage ciclosporin who maintained a mean Cmin of everolimus in blood of ≥3 ng/mL.
Everolimus 1.5 or 3 mg/day was compared with azathioprine 1–3 mg/kg/day (both combined with full-dosage ciclosporin) in a large, randomised trial in 634 adults undergoing primary heart transplantation, with follow-up data available for 4 years. Efficacy failure was a composite of the incidence of BPAR (International Society for Heart and Lung Transplantation grade 3A or greater), rejection associated with haemodynamic compromise, graft loss or retransplantation, and death or loss to follow-up. Both dosages of everolimus were significantly more effective than azathioprine in preventing efficacy failure over 4 years of follow-up. Patient survival rates were similar across all treatment groups. Both dosages of everolimus were also significantly more effective than azathioprine at reducing the incidence of cardiac allograft vasculopathy as indicated by intravascular ultrasound. There was evidence of an association between increasing everolimus exposure and reduced severity of vasculopathy after 12 months.
Tolerability
Looking at renal function, serum creatinine levels increased during treatment of renal and cardiac transplant patients with everolimus plus full-dosage ciclosporin, and serum creatinine levels were generally higher among recipients of everolimus than among those treated with mycophenolate mofetil or azathioprine, particularly with everolimus 3 mg/day. Renal function was better preserved in patients treated with everolimus plus reduced-dosage ciclosporin than with everolimus plus full-dosage ciclosporin. Everolimus should not be used in combination with fulldosage ciclosporin over the long term; reductions in ciclosporin should start within 1 month after renal transplantation.
Among general adverse events, the most common events possibly or probably associated with everolimus in phase III trials were leukopenia, hypercholesterolaemia and hyperlipidaemia, which each occurred in >10% of patients overall. Adverse events reported at an incidence of 1–10% included infections (including pneumonia and urinary tract infections), blood disorders (e.g. anaemia, thrombocytopenia, coagulopathy, haemolytic uraemic syndrome), hypertriglyceridaemia, vascular disorders (e.g. hypertension, lymphocoele [in renal transplantation patients], thromboembolism), gastrointestinal symptoms (e.g. abdominal pain, diarrhoea, nausea, vomiting) and oedema.
Approximately three-quarters of all patients in major clinical trials experienced infections. The incidence of viral infections (including CMV infection) was lower with everolimus than with mycophenolate mofetil in one of two trials in renal transplantation. Viral infections (including CMV infection) were also less frequent with everolimus than with azathioprine among heart transplant recipients, although bacterial infections were more common with everolimus 3 mg/day than with azathioprine. The incidence of elevated lipid levels was greater among everolimus recipients than among patients treated with mycophenolate mofetil or azathioprine. In renal transplant trials, wound healing complications, specifically lymphocoele, occurred in numerically (but not statistically significantly) more recipients of everolimus than of mycophenolate mofetil.
Pharmacoeconomic Considerations
A cost analysis based on outcomes in 588 renal transplant recipients and another study assessing cost and cost effectiveness in 634 patients undergoing heart transplantation have been based on phase III studies of everolimus. Both analyses were carried out from a healthcare payer’s perspective, and focused on direct costs only with the exclusion of the cost of everolimus or the comparator immunosup-pressant. Mean overall costs of treatment were similar across patient groups in both studies, with no significant differences between everolimus and mycophenolate mofetil or azathioprine. In the renal transplantation analysis, lower total cumulative doses of ciclosporin in the everolimus groups led to significantly lower mean ciclosporin costs in these groups than in the mycophenolate mofetil group. In heart transplant recipients, incremental costs over azathioprine for each additional patient free from efficacy failure with everolimus 1.5 and 3 mg/day were, respectively, $US11 181 and $US8823 (year of costing 2001). Sensitivity analyses in which a range of hypothetical costs (based on the cost of mycophenolate mofetil) were attached to everolimus showed the findings to be robust.








Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Perico N, Remuzzi G. Prevention of transplant rejection: current treatment guidelines and future developments. Drugs 1997; 54(4): 533–70
Jorga A, Johnston A. Novel therapies in transplantation. Expert Opin Invest Drugs 2005; 14(3): 295–304
National Institute for Clinical Excellence. Kidney transplant patients to benefit from latest NICE guidance on immunosuppressive therapy [online]. Available from URL: http://www.nice.org.uk/pdf/2004_040_renal_transplant.pdf [Accessed 2005 Sep 30]
Kovarik JM. Everolimus: a proliferation signal inhibitor targeting primary causes of allograft dysfunction. Drugs Today (Barc) 2004; 40(2): 101–9
Calne RY, Collier DS, Lim S, et al. Rapamycin for immunosuppression in organ allografting [letter]. Lancet 1989; 2(8656): 227
Sedrani R, Cottens S, Kallen J, et al. Chemical modification of rapamycin: the discovery of SDZ RAD. Transplant Proc 1998; 30: 2192–4
Chapman TM, Perry CM. Everolimus. Drugs 2004; 64(8): 861–72
Nashan B. Early clinical experience with a novel rapamycin derivative. Ther Drug Monit 2002; 24(1): 53–8
Novartis Sverige AB. Summary of the product characteristics: Certican tablets. Täby, Sweden, 2003 [online]. Available from URL: http://www.mpa.se/eng [Accessed 2006 Jan 23]
Schuler W, Sedrani R, Cottens S, et al. SDZ RAD, a new rapamycin derivative: pharmacological properties in vitro and in vivo. Transplantation 1997; 64(1): 36–42
Dunn CJ, Wagstaff AJ, Perry CM, et al. Cyclosporin: an updated review of the pharmacokinetic properties, clinical efficacy and tolerability of a microemulsion-based formulation (Neoral®) in organ transplantation. Drugs 2001; 61(13): 1957–2016
Fulton B, Markham A. Mycophenolate mofetil: a review of its pharmacodynamic and pharmacokinetic properties and clinical efficacy in renal transplantation. Drugs 1996; 51(2): 278–98
Kovarik JM, Kaplan B, Tedesco Silva H, et al. Exposure-response relationships for everolimus in de novo kidney transplantation: defining a therapeutic range. Transplantation 2002 Mar 27; 73(6): 920–5
Azzola A, Havryk A, Chhajed P, et al. Everolimus and mycophenolate mofetil are potent inhibitors of fibroblast proliferation after lung transplantation. Transplantation 2004; 77(2): 275–80
Snell GI, Valentine VG, Vitulo P, et al. Everolimus versus azathioprine in maintenance lung transplant recipients: an international, randomized, double-blind clinical trial. Am J Transplant 2006; 6(1): 169–77
Boehler T, Waiser J, Schumann B, et al. The rapamycin analogue SDZ RAD inhibits LPS and anti-CD3mAb induced IL-10 synthesis in vitro and in human renal allograft recipients [abstract no. 956]. Transplantation 2000; 69(8): 360
Böhler T, Waiser J, Budde K, et al. The in vivo effect of rapamycin derivative SDZ RAD on lymphocyte proliferation. Transplant Proc 1998; 30: 2195–7
Game DS, Hernandez-Fuentes MP, Lechler RI. Everolimus and basiliximab permit suppression by human CD4+CD25+ cells in vitro. Am J Transplant 2005; 5(3): 454–64
Viklicky O, Zou H, Müller V, et al. SDZ-RAD prevents manifestation of chronic rejection in rat renal allografts. Transplantation 2000; 69(4): 497–502
Schuurman H-J, Pally C, Weckbecker G, et al. SDZ RAD inhibits cold ischemia-induced vascular remodeling. Transplant Proc 1999; 31: 1024–5
Cole OJ, Shehata M, Rigg KM. Effect of SDZ RAD on transplant arteriosclerosis in the rat aortic model. Transplant Proc 1998; 30: 2200–3
Matsumoto Y, Hof A, Baumlin Y, et al. Differential effect of cyclosporin A and SDZ RAD on neointima formation of carotid allografts in apolipoprotein E-deficient mice. Transplantation 2003 Oct 27; 76(8): 1166–70
Matsumoto Y, Hof A, Baumlin Y, et al. Differential effects of everolimus and cyclosporine A on intimai α-actin-positive cell dynamics of carotid allografts in mice. Transplantation 2004; 78(3): 345–51
Salminen US, Maasilta PK, Taskinen El, et al. Prevention of small airway obliteration in a swine heterotopic lung allograft model. J Heart Lung Transplant 2000; 19(2): 193–206
Salminen US, Alho H, Taskinen E, et al. Effects of rapamycin analogue SDZ RAD on obliterative lesions in a porcine heterotopic bronchial allograft model. Transplant Proc 1998; 30: 2204–5
Weckbecker G, Caballero V, Court M, et al. Differential effects of FTY720, RAD, and CsA on signs of chronic rejection in the rat tracheal allograft model. Graft 2002; 5(3): 145–8
Schuurman H-J, Cottens S, Fuchs S, et al. SDZ RAD, a new rapamycin derivative: synergism with cyclosporine. Transplantation 1997; 64(1): 32–5
Hausen B, Boeke K, Berry GJ, et al. Coadministration of neoral and the novel rapamycin analog, SDZ RAD, to rat lung allograft recipients: potentiation of immunosuppressive efficacy and improvement of tolerability of staggered versus simultaneous treatment. Transplantation 1999; 67(7): 956–62
Schuurman H-J, Ringers J, Schuler W, et al. Oral efficacy of the macrolide immunosuppressant SDZ RAD and of cyclosporine microemulsion in cynomolgus monkey kidney allotransplantation. Transplantation 2000; 69(5): 737–42
Hausen B, Ikonen T, Briffa N, et al. Combined immunosuppression with cyclosporine (neoral) and SDZ RAD in non-human primate lung transplantation: systematic pharmacokineticbased trials to improve efficacy and tolerability. Transplantation 2000; 69(1): 76–86
Nikolova Z, Hof A, Baumlin Y, et al. The peripheral lymphocyte count predicts graft survival in DA to Lewis heterotopic heart transplantation treated with FTY720 and SDZ RAD. Transpl Immunol 2000; 8(2): 115–24
Reis A, Megahed M, Reinhard T, et al. Coadministration of the new macrolide immunosuppressant RAD and mycophenolate mofetil in experimental corneal transplantation. Transplantation 2000; 70(9): 1397–401
Stracke S, Ramudo L, Keller F, et al. Different antiproliferative capacity and overadditive effects of everolimus and mycophenolate mofetil in endothelial and vascular smooth muscle cells in vitro [abstract no. 271]. Am J Transplant 2005; 5 Suppl. 11: 225
Delaney MP, Higgins RM, Morris AG. FK506 and the rapamycin analogue, SDZ RAD do not have antagonistic effects on lymphocytes from renal transplant patients [abstract no. 657]. Am J Transplant 2001; 1 Suppl. 1: 301
Kovarik JM, Hartmann S, Figueiredo J, et al. Effect of rifampin on apparent clearance of everolimus. Ann Pharmacother 2002 Jun; 36(6): 981–5
Kahan BD, Wong RL, Carter C, et al. A phase I study of a 4-week course of SDZ-RAD (RAD) quiescent cyclosporine-prednisone-treated renal transplant recipients. Transplantation 1999; 68: 1100–6
Kovarik JM, Kaplan B, Tedesco Silva H, et al. Pharmacokinetics of an everolimus-cyclosporine immunosuppressive regimen over the first 6 months after kidney transplantation. Am J Transplant 2003; 3(5): 606–13
Kovarik JM, Hartmann S, Figueiredo J, et al. Effect of food on everolimus absorption: quantification in healthy subjects and a confirmatory screening in patients with renal transplants. Pharmacotherapy 2002; 22(2): 154–9
Kovarik JM, Kahan BD, Kaplan B, et al. Longitudinal assessment of everolimus in de novo renal transplant recipients over the first post-transplant year: pharmacokinetics, exposure-response relationships, and influence on cyclosporine. Clin Pharmacol Ther 2001; 69: 48–56
Kovarik JM, Sabia H, Rouilly M, et al. Influence of renal and hepatic impairment on everolimus pharmacokinetics: are dose adjustments necessary? [abstract no. 989]. Am J Transplant 2001; 1 Suppl. 1: 385
Neumayer H-H, Paradis K, Korn A, et al. Entry-into-human study with the novel immunosuppressant SDZ RAD in stable renal transplant recipients. Br J Clin Pharmacol 1999; 48: 694–703
Levy GA, Grant D, Paradis K, et al. Pharmacokinetics and tolerability of 40-0-[2-hydroxyethyl]rapamycin in de novo liver transplant recipients. Transplantation 2001; 71(1): 160–3
Budde K, Neumayer H-H, Lehne G, et al. Tolerability and steady-state pharmacokinetics of everolimus in maintenance renal transplant patients. Nephrol Dial Transplant 2004; 19(10): 2606–14
Kovarik JM, Eisen H, Dorent R, et al. Everolimus in de novo cardiac transplantation: pharmacokinetics, therapeutic range, and influence on cyclosporine exposure. J Heart Lung Transplant 2003; 22(10): 1117–25
Doyle RL, Hertz MI, Dunitz JM, et al. RAD in stable lung and heart/lung transplant recipients: safety, tolerability, pharmacokinetics, and impact of cystic fibrosis. J Heart Lung Transplant 2001; 20(3): 330–9
Kirchner GI, Meier-Wiedenbach I, Manns MP. Clinical pharmacokinetics of everolimus. Clin Pharmacokinet 2004; 43(2): 83–95
Serkova N, Hausen B, Berry GJ, et al. Tissue distribution and clinical monitoring of the novel macrolide immunosuppressant SDZ-RAD and its metabolites in monkey lung transplant recipients: interaction with cyclosporine. J Pharmacol Exp Ther 2000; 294(1): 323–32
Jacobsen W, Serkova N, Hausen B, et al. Comparison of the in vitro metabolism of the macrolide immunosuppressants sirolimus and RAD. Transplant Proc 2001; 33(1–2): 514–5
Kirchner GI, Winkler M, Mueller L, et al. Pharmacokinetics of SDZ RAD and cyclosporin including their metabolites in seven kidney graft patients after the first dose of SDZ RAD. Br J Clin Pharmacol 2000; 50(5): 449–54
Kirchner GI, Mueller L, Winkler M, et al. Long-term pharmacokinetics of the metabolites of everolimus and cyclosporine in renal transplant recipients. Transplant Proc 2002; 34(6): 2233–4
Kovarik JM, Hsu C-H, McMahon L, et al. Population pharmacokinetics of everolimus in de novo renal transplant patients: impact of ethnicity and comedications. Clin Pharmacol Ther 2001; 70(3): 247–54
Kovarik JM, Sabia HD, Figueiredo J, et al. Influence of hepatic impairment on everolimus pharmacokinetics: implications for dose adjustment. Clin Pharmacol Ther 2001; 70(5): 425–30
Kovarik JM, Kalbag J, Figueiredo J, et al. Differential influence of two cyclosporine formulations on everolimus pharmacokinetics: a clinically relevant pharmacokinetic interaction. J Clin Pharmacol 2002; 42(1): 95–9
Budde K, Lehne G, Winkler M, et al. Influence of everolimus on steady-state pharmacokinetics of cyclosporine in maintenance renal transplant patients. J Clin Pharmacol 2005; 45(7): 781–91
Kovarik JM, Dantal J, Civati G, et al. Influence of delayed initiation of cyclosporine on everolimus pharmacokinetics in de novo renal transplant patients. Am J Transplant 2003; 3: 1576–80
Kovarik JM, Beyer D, Bizot MN, et al. Effect of multiple-dose erythromycin on everolimus pharmacokinetics. Eur J Clin Pharmacol 2005; 61(1): 35–8
Kovarik JM, Beyer D, Bizot MN, et al. Blood concentrations of everolimus are markedly increased by ketoconazole. J Clin Pharmacol 2005; 45(5): 514–8
Kovarik JM, Hartmann S, Hubert M, et al. Pharmacokinetic and pharmacodynamic assessments of HMG-CoA reductase inhibitors when coadministered with everolimus. J Clin Pharmacol 2002; 42(2): 222–8
Nashan B, Curtis J, Ponticelli C, et al. Everolimus and reduced-exposure cyclosporine in de novo renal-transplant recipients: a three-year phase II, randomized, multicenter, open-label study. Transplantation 2004; 78(9): 1332–40
Vitko S, Margreiter R, Weimar W, et al. Everolimus (Certican) 12-month safety and efficacy versus mycophenolate mofetil in de novo renal transplant recipients. Transplantation 2004; 78(10): 1532–40
Vitko S, Margreiter R, Weimar W, et al. Three-year efficacy and safety results from a study of everolimus versus mycophenolate mofetil in de novo renal transplant patients. Am J Transplant 2005; 5: 2521–30
Lorber MI, Mulgaonkar S, Butt KM, et al. Everolimus versus mycophenolate mofetil in the prevention of rejection in de novo renal transplant recipients: a 3-year randomized, multicenter, phase III study. Transplantation 2005 Jul 27; 80(2): 244–52
Vitko S, Tedesco H, Eris J, et al. Everolimus with optimized cyclosporine dosing in renal transplant recipients: 6-month safety and efficacy results of two randomized studies. Am J Transplant 2004; 4: 626–35
Magee J, Tedesco H, Pascual J, et al. Efficacy and safety of 2 doses of everolimus combined with reduced dose Neoral® in de novo kidney transplant recipients: 12 months analysis [abstract no. 504]. Am J Transplant 2004; 4 Suppl. 8: 296–7
Pascual J, Cambi V, Dissegna D, et al. Efficacy and safety of 2 doses of everolimus combined with reduced dose Neoral® in de novo kidney transplant recipients: 24 months analysis [abstract no. 1010]. Am J Transplant 2005; 5 Suppl. 11: 414
Whelchel J, Vitko S, Eris J, et al. Excellent graft function in de novo kidney transplant recipients treated with Certican®, Simulect ® and reduced Neoral® exposure: 12-month results [abstract no. 507]. Am J Transplant 2004; 4 Suppl. 8: 297
Leone J, Vitko S, Whelchel J, et al. Excellent graft function in de novo kidney transplant recipients treated with Certican®, Simulect® and reduced Neoral® exposure: 24 month result [abstract no. 1011]. Am J Transplant 2005; 5 Suppl. 11: 414
Lorber MI, Ponticelli C, Whelchel J, et al. Therapeutic drug monitoring for everolimus in kidney transplantation using 12-month exposure, efficacy, and safety data. Clin Transplant 2005 Apr; 19(2): 145–52
Eisen HJ, Tuzcu EM, Dorent R, et al. Everolimus for the prevention of allograft rejection and vasculopathy in cardiactransplant recipients. N Engl J Med 2003; 349(9): 847–58
Hauck W, Delgado D, Perrone S, et al. Everolimus reduces cardiac allograft vasculopathy in de novo heart transplant recipients: 24 month follow-up [abstract no. 153]. Can J Cardiol 2003 Oct; 19. Suppl.: 90A
Hare J, Perrone S, Eisen H. 48M follow up: everolimus in cardiac transplantation. The RAD B253 Team Cardiology [abstract no. OR-032 plus oral presentation]. 12th European Society for Organ Transplantation Congress; 2005 Oct 15–19; Geneva [online]. Available from URL: http://www.abstracts2view.com/esot [Accessed 2006 Feb 17]
Starling RC, Hare JM, Hauptman P, et al. Therapeutic drug monitoring for everolimus in heart transplant recipients based on exposure-effect modeling. Am J Transplant 2004; 4(12): 2126–31
Eisen H, Starling R, Kobashigawa J. Incidence of MACE and economic burden in de novo heart transplantation patients: a 4-year comparison of everolimus and azathioprine [poster no. PO-111]. 12th European Society for Organ Transplantation Congress; 2005 Oct 15–19; Geneva
Holmes M, Chilcott J, Walters S, et al. Economic evaluation of everolimus versus mycophenolate mofetil in combination with cyclosporine and prednisolone in de novo renal transplant recipients. Transpl Int 2004; 17(4): 182–7
Radeva JI, Reed SD, Kalo Z, et al. Economic evaluation of everolimus vs. azathioprine at one year after de novo heart transplantation. Clin Transplant 2005; 19(1): 122–9
Keown P, Ethgen O, Yang XL, et al. Economic evaluation of everolimus with reduced-dose cyclosporine in de novo renal transplant recipients [abstract no. 1369]. Am J Transplant 2005; 5 Suppl. 11: 504
Tenderich G, Dorent R, Yang XL, et al. Cost-effectiveness of everolimus vs mycophenolate mofetil in de novo heart transplant recipients [abstract no. 375]. Am J Transplant 2005; 5 Suppl. 11: 251
Ethgen O, Yang XL, Spaepen E, et al. Everolimus with reduced-dose cyclosporine vs mycophenolate mofetil with full-dose cyclosporine: a European health economic perspective in de novo renal transplant recipients [poster no. PO-229]. 12th European Society for Organ Transplantation Congress; 2005 Oct 15–19; Geneva
Lehmkuhl H, Tenderich G, Annemans L. Economic evaluation of everolimus and mycophenolate mofetil vs azathioprine in de novo heart transplantation [poster no. PO-96]. 12th European Society for Organ Transplantation Congress; 2005 Oct 15–19; Geneva
Kobashigawa J, Miller L, Renlund D, et al. A randomized active-controlled trial of mycophenolate mofetil in heart transplant recipients. Mycophenolate Mofetil Investigators. Transplantation 1998; 66(4): 507–15
Cecka JM. The UNOS renal transplant registry. In: Cecka JM, Terasaki PI, editors. Clinical transplants 2002. Los Angeles: UCLA Immunogenetics Center, 2002: 1–20
International Society for Heart and Lung Transplantation. ISHLT transplant registry quarterly reports for heart in North America: survival rates for transplants performed between January 1, 2000 and December 31, 2003 [online]. Available from URL: http://www.ishlt.org/registries [Accessed 2006 Feb 16]
Hariharan S, Johnson CP, Bresnahan BA, et al. Improved graft survival after renal transplantation in the United States, 1988 to 1996. New Engl J Med 2000; 342(9): 605–12
Meier-Kriesche HU, Schold JD, Srinivas TR, et al. Lack of improvement in renal allograft survival despite a marked decrease in acute rejection rates over the most recent era. Am J Transplant 2004; 4(3): 378–83
US Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients. OPTN/SRTR 2005 annual report: survival rates. Table 1.13 [online]. Available from URL: http://www.optn.org [Accessed 2006 Feb 24]
Schweitzer EJ, Matas AJ, Gillingham KJ, et al. Causes of renal allograft loss: progress in the 1980s, challenges for the 1990s. Ann Surg 1991; 214(6): 679–88
Flechner SM, Modlin CS, Serrano DP, et al. Determinants of chronic renal allograft rejection in cyclosporine-treated recipients. Transplantation 1996; 62(9): 1235–41
Hostetter TH. Chronic transplant rejection. Kidney Int 1994; 46(1): 266–79
Massy ZA, Guijarro C, Wiederkehr MR, et al. Chronic renal allograft rejection: immunologic and nonimmunologic risk factors. Kidney Int 1996; 49(2): 518–24
Keck BM, Bennett LE, Rosendale J, et al. Worldwide thoracic organ transplantation: a report from the UNOS/ISHLT international registry for thoracic organ transplantation. In: Cecka JM, Terasaki PI, editors. Clinical transplants 1999. Los Angeles: UCLA Immunogenetics Center, 1999: 35–49
Laine J, Holmberg C, Hayry P. Chronic rejection and late allograft dysfunction. Pediatr Nephrol 1996; 10(2): 221–9
Sollinger HW. Mycophenolate mofetil for the prevention of acute rejection in primary cadaveric renal allograft recipients. US Renal Transplant Mycophenolate Mofetil Study Group. Transplantation 1995; 60(3): 225–32
Anon. A blinded, randomized clinical trial of mycophenolate mofetil for the prevention of acute rejection in cadaveric renal transplantation. The Tricontinental Mycophenolate Mofetil Renal Transplantation Study Group. Transplantation 1996; 61: 1029–37
Valantine H. Cardiac allograft vasculopathy after heart transplantation: risk factors and management. J Heart Lung Transplant 2004; 23 (5 Suppl.): S187–93
Kobashigawa JA, Tobis JM, Starling RC, et al. Multicenter intravascular ultrasound validation study among heart transplant recipients: outcomes after 5 years. J Am Coll Cardiol 2005; 45(9): 1532–7
Eisen H, Kobashigawa J, Starling RC, et al. Improving outcomes in heart transplantation: the potential of proliferation signal inhibitors. Transplant Proc 2005; 37 (4 Suppl.): 4–17S
Avery RK. Viral triggers of cardiac-allograft dysfunction. N Engl J Med 2001; 344: 1545–7
Lindenfeld J, Miller GG, Shakar SF, et al. Drug therapy in the heart transplant recipient. Part II: immunosuppressive drugs. Circulation 2004; 110(25): 3858–65
Clinical Trials Insight. Everolimus in transplant rejection: ongoing trials [online]. Available from URL: http://bi.adisinsight.com/cti [Accessed 2006 Feb 27]
Kuypers DRJ. Benefit-risk assessment of sirolimus in renal transplantation. Drug Saf 2005; 28(2): 153–81
Ross H, Burton J, Pflugfelder P, et al. Neoral® and Certican® can be safely combined in stable cardiac transplant recipients: 12-week interim analysis of a Canadian pilot study [poster no. PO-97]. 12th European Society for Organ Transplantation Congress; 2005 Oct 15–19; Geneva
Lehmkuhl H, Ross H, Eisen H, et al. Everolimus (Certican) in heart transplantation: optimizing renal function through minimizing cyclosporine exposure. Transplant Proc 2005; 37(10): 4145–9
Mabasa VH, Ensom MH. The role of therapeutic monitoring of everolimus in solid organ transplantation. Ther Drug Monit 2005; 27(5): 666–76
Neumayer H-H. Introducing everolimus (Certican) in organ transplantation: an overview of preclinical and early clinical developments. Transplantation 2005; 79: S72–5
Wyeth Pharmaceuticals Inc. Rapamune® (sirolimus): oral solution and tablets package insert [online]. Available from URL: http://www.wyeth.com [Accessed 2006 Feb 28]
Hale DA, Kirk AD. Mammalian target of rapamycin inhibitors in transplantation: novel immunosuppressive strategies with sirolimus. Curr Opin Organ Transplant 2004; 9(4): 400–5
Montagnino G, Sandrini S, Casciani C, et al. A randomized trial of steroid avoidance in renal transplant patients treated with everolimus and cyclosporine. Transplant Proc 2005; 37(2): 788–90
Evans RW. Cost-effectiveness analysis of transplantation. Surg Clin North Am 1986; 66(3): 603–16
Evans RW. Socioeconomic aspects of heart transplantation. Curr Opin Cardiol 1995; 10(2): 169–79
van Hout B, Bonsel G, Habbema D, et al. Heart transplantation in the Netherlands; costs, effects and scenarios. J Health Econ 1993; 12(1): 73–93
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: K. Budde, Medizinische Klinik mS Nephrologie, Universitätsmedizin Berlin Charité, Berlin, Germany; H.J. Eisen, Division of Cardiology, Drexel University College of Medicine, Philadelphia, Pennsylvania, USA; M. Kuwana, Department of Internal Medicine, Keio University School of Medicine, Tokyo, Japan; B. Nashan, Multi Organ Transplant Program, QEII Health Sciences Centre, Dalhousie University, Halifax, Canada; H.-H. Neumayer, Medizinische Klinik mS Nephrologie, Universitätsmedizin Berlin Charité, Berlin, Germany; J. Patel, UCLA Heart Transplant Program, David Geffen School of Medicine at UCLA, Los Angeles, California, USA; G. Remuzzi, Mario Negro Institute for Pharmacological Research, Bergamo, Italy.
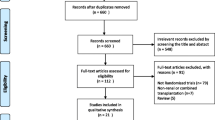
Data Selection
Sources: Medical literature published in any language since 1980 on ‘everolimus’, identified using MEDLINE and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: MEDLINE search terms were ‘everolimus’. EMBASE search terms were ‘everolimus’. AdisBase search terms were ‘everolimus’ or ‘SDZ-RAD’. Searches were last updated 9 March 2006.
Selection: Studies in renal and cardiac transplant patients who received everolimus. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: everolimus, cardiac transplantation, pharmacodynamics, pharmacokinetics, renal transplantation, therapeutic use, tolerability.
Rights and permissions
About this article
Cite this article
Dunn, C., Croom, K.F. Everolimus. Drugs 66, 547–570 (2006). https://doi.org/10.2165/00003495-200666040-00009
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200666040-00009