Abstract
Background
Two-stage hepatectomy (TSH) is an important tool in the management of bilateral colorectal liver metastases (CRLM). This study sought to examine the presentation, management, and outcomes of patients completing TSH in major hepatobiliary centers in the United States (US).
Methods
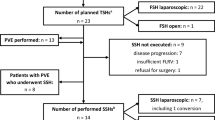
A retrospective review from five liver centers in the US identified patients who completed a TSH procedure for bilateral CRLM.
Results
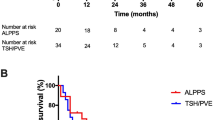
From December 2000 to March 2016, a total of 196 patients were identified. The majority of procedures were performed using an open technique (n = 194, 99.5%). The median number of tumors was 7 (range 2–33). One-hundred and twenty-eight (65.3%) patients underwent portal vein embolization. More patients received chemotherapy prior to the first stage than chemotherapy administration preceding the second stage (92% vs. 60%, p = 0.308). Median overall survival (OS) was 50 months, with a median follow-up of 28 months (range 2–143). Hepatic artery infusion chemotherapy was administered to 64 (32.7%) patients with similar OS as those managed without an infusion pump (p = 0.848). Postoperative morbidity following the second-stage resection was 47.4%. Chemotherapy prior to the second stage did not demonstrate an increased complication rate (p = 0.202). Readmission following the second stage was 10.3% and was associated with a decrease in disease-free survival (p = 0.003). OS was significantly decreased by positive resection margins and increased estimated blood loss (EBL; p = 0.036 and p = 0.05, respectively).
Conclusion
This is the largest TSH series in the US and demonstrates evidence of safety and feasibility in the management of bilateral CRLM. Outcomes are influenced by margin status and operative EBL.

Similar content being viewed by others
References
American Cancer Society. Cancer Facts & Figures 2019 [database online]. Atlanta, GA: American Cancer Society; 2019.
Clavien P. Malignant liver tumors: current and emerging therapies. Chichester: Wiley-Blackwell; 2010.
Groeschl RT, Nachmany I, Steel JL, et al. Hepatectomy for noncolorectal non-neuroendocrine metastatic cancer: a multi-institutional analysis. J Am Coll Surg 2012; 214(5):769–77.
Belghiti J, Hiramatsu K, Benoist S, et al. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg 2000; 191(1):38–46.
Jarnagin WR, Gonen M, Fong Y, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg 2002; 236(4):397–406; discussion 406–7.
Kemeny N. Presurgical chemotherapy in patients being considered for liver resection. Oncologist 2007; 12(7):825–39.
Abdalla EK, Vauthey JN, Ellis LM, et al. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 2004; 239(6):818–25; discussion 825–7.
Aloia TA, Vauthey JN, Loyer EM, et al. Solitary colorectal liver metastasis: resection determines outcome. Arch Surg 2006; 141(5):460–6; discussion 466–7.
Kanas GP, Taylor A, Primrose JN, et al. Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol 2012; 4:283–301.
Tomizawa N, Ohwada S, Ogawa T, et al. Factors affecting the prognosis of anatomical liver resection for liver metastases from colorectal cancer. Hepatogastroenterology 2006; 53(67):89–93.
Wei AC, Greig PD, Grant D, et al. Survival after hepatic resection for colorectal metastases: a 10-year experience. Ann Surg Oncol 2006; 13(5):668–76.
Adam R, Laurent A, Azoulay D, et al. Two-stage hepatectomy: A planned strategy to treat irresectable liver tumors. Ann Surg 2000; 232(6):777–85.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240(2):205–13.
Adam R, De Gramont A, Figueras J, et al. The oncosurgery approach to managing liver metastases from colorectal cancer: a multidisciplinary international consensus. Oncologist 2012; 17(10):1225–39.
Wicherts DA, de Haas RJ, Andreani P, et al. Impact of portal vein embolization on long-term survival of patients with primarily unresectable colorectal liver metastases. Br J Surg 2010; 97(2):240–50.
Imai K, Allard MA, Castro Benitez C, et al. Long-term outcomes of radiofrequency ablation combined with hepatectomy compared with hepatectomy alone for colorectal liver metastases. Br J Surg 2017; 104(5):570–9.
Philips P, Groeschl RT, Hanna EM, et al. Single-stage resection and microwave ablation for bilobar colorectal liver metastases. Br J Surg 2016; 103(8):1048–54.
Wicherts DA, Miller R, de Haas RJ, et al. Long-term results of two-stage hepatectomy for irresectable colorectal cancer liver metastases. Ann Surg 2008; 248(6):994–1005.
Tsai S, Marques HP, de Jong MC, et al. Two-stage strategy for patients with extensive bilateral colorectal liver metastases. HPB (Oxford) 2010; 12(4):262–9.
Lam VW, Laurence JM, Johnston E, et al. A systematic review of two-stage hepatectomy in patients with initially unresectable colorectal liver metastases. HPB (Oxford) 2013; 15(7):483–91.
Regimbeau JM, Cosse C, Kaiser G, et al. Feasibility, safety and efficacy of two-stage hepatectomy for bilobar liver metastases of colorectal cancer: a LiverMetSurvey analysis. HPB (Oxford) 2017; 19(5):396–405.
Wang J, Margonis GA, Amini N, et al. The prognostic value of varying definitions of positive resection margin in patients with colorectal cancer liver metastases. J Gastrointest Surg 2018; 22(8):1350–7.
Miller CL, Taylor MS, Qadan M, et al. Prognostic significance of surgical margin size after neoadjuvant FOLFOX and/or FOLFIRI for colorectal liver metastases. J Gastrointest Surg 2017; 21(11):1831–40.
Laurent C, Adam JP, Denost Q, et al. Significance of R1 resection for advanced colorectal liver metastases in the era of modern effective chemotherapy. World J Surg 2016; 40(5):1191–9.
Andreou A, Aloia TA, Brouquet A, et al. Margin status remains an important determinant of survival after surgical resection of colorectal liver metastases in the era of modern chemotherapy. Ann Surg 2013; 257(6):1079–88.
Postlewait LM, Squires MH, 3rd, Kooby DA, et al. The relationship of blood transfusion with peri-operative and long-term outcomes after major hepatectomy for metastatic colorectal cancer: a multi-institutional study of 456 patients. HPB (Oxford) 2016; 18(2):192–9.
Linecker M, Kuemmerli C, Clavien PA, et al. Dealing with insufficient liver remnant: Associating liver partition and portal vein ligation for staged hepatectomy. J Surg Oncol 2019; 119(5):604–12.
Moris D, Ronnekleiv-Kelly S, Kostakis ID, et al. Operative results and oncologic outcomes of associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) versus two-stage hepatectomy (TSH) in patients with unresectable colorectal liver metastases: a systematic review and meta-analysis. World J Surg 2018; 42(3):806–15.
Zhou Z, Xu M, Lin N, et al. Associating liver partition and portal vein ligation for staged hepatectomy versus conventional two-stage hepatectomy: a systematic review and meta-analysis. World J Surg Oncol 2017; 15(1):227.
Ratti F, Schadde E, Masetti M, et al. Strategies to increase the resectability of patients with colorectal liver metastases: a multi-center case-match analysis of ALPPS and conventional two-stage hepatectomy. Ann Surg Oncol 2015; 22(6):1933–42.
Sandström P, Røsok BI, Sparrelid E, et al. ALPPS improves resectability compared with conventional two-stage hepatectomy in patients with advanced colorectal liver metastasis: results from a scandinavian multicenter randomized controlled trial (LIGRO trial). Ann Surg 2018; 267(5):833–40.
Adam R, Imai K, Castro Benitez C, et al. Outcome after associating liver partition and portal vein ligation for staged hepatectomy and conventional two-stage hepatectomy for colorectal liver metastases. Br J Surg 2016; 103(11):1521–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mariana I. Chavez, Sepideh Gholami, Bradford J. Kim, Georgios A. Margonis, Cecilia G. Ethun, Susan Tsai, Kathleen K. Christians, Callisia Clarke, Harveshp Mogal, Shishir K. Maithel, Timothy M. Pawlik, Michael I. D’Angelica, Thomas A. Aloia, Daniel Eastwood, and T. Clark Gamblin declare they have no conflicts of interest or financial disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chavez, M.I., Gholami, S., Kim, B.J. et al. Two-Stage Hepatectomy for Bilateral Colorectal Liver Metastases: A Multi-institutional Analysis. Ann Surg Oncol 28, 1457–1465 (2021). https://doi.org/10.1245/s10434-020-09459-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09459-6