Abstract
Background
Skeletal muscle loss during the early postoperative period frequently occurs during post-esophagectomy. Preoperative sarcopenia is a known prognostic factor. However, the prognostic significance of postoperative skeletal muscle loss remains unclear. This study was designed to clarify the impact of skeletal muscle loss during the early postoperative period on the prognosis of elderly patients undergoing esophagectomy.
Methods
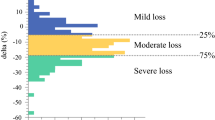
We included 316 patients (age ≥ 65 years) who underwent esophagectomy. The skeletal muscle index (SMI) at the third lumber vertebra’s bottom level was measured using computed tomography (CT) before surgery and 4 months after surgery. The SMI reduction rate, patient’s prognosis, and recurrence rates were evaluated.
Results
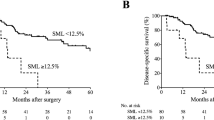
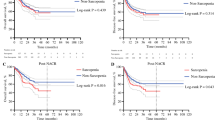
The SMI reduction rates in tertiles were < 1.25% in the first tertile (t1, n = 105), between 1.25 and 9.13% in the second tertile (t2, n = 106), and > 9.13% in the third tertile (t3, n = 105). Both relapse-free survival (RFS) and overall survival (OS) in t3 were significantly worse than those in t1 and t2 (p < 0.001). Therefore, we defined t3 as the massive reduction (MR) group and t1 and t2 as the limited reduction (LR) group. By univariate analysis, both RFS and OS were significantly poorer in the MR group than in LR. By multivariate analysis, the massive skeletal muscle loss during the early postoperative period was an independent factor for both RFS and OS.
Conclusions
Early postoperative skeletal muscle loss predicts both recurrence and poor survival.

Similar content being viewed by others
References
Fujita H, Kakegawa T, Yamana H, et al. Mortality and morbidity rates, postoperative course, quality of life, and prognosis after extended radical lymphadenectomy for esophageal cancer. Comparison of three-field lymphadenectomy with two-field lymphadenectomy. Ann Surg. 1995;222(5):654–62.
Takeuchi H, Miyata H, Gotoh M, et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg. 2014;260(2):259–66.
Mariette C, Piessen G, Triboulet JP. Therapeutic strategies in oesophageal carcinoma: role of surgery and other modalities. Lancet Oncol. 2007;8(6):545–53.
Baba Y, Yoshida N, Shigaki H, et al. Prognostic impact of postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma: a retrospective single-institution study. Ann Surg. 2016;264(2):305–11.
Saeki H, Tsutsumi S, Tajiri H, et al. Prognostic significance of postoperative complications after curative resection for patients with esophageal squamous cell carcinoma. Ann Surg. 2017;265(3):527–33.
Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997;127(5 Suppl):990s–1s.
Ida S, Watanabe M, Yoshida N, et al. Sarcopenia is a predictor of postoperative respiratory complications in patients with esophageal cancer. Ann Surg Oncol. 2015;22(13):4432–7.
Nakashima Y, Saeki H, Nakanishi R, et al. Assessment of sarcopenia as a predictor of poor outcomes after esophagectomy in elderly patients with esophageal cancer. Ann Surg. 2018;267(6):1100–4.
Jarvinen T, Ilonen I, Kauppi J, Salo J, Rasanen J. Loss of skeletal muscle mass during neoadjuvant treatments correlates with worse prognosis in esophageal cancer: a retrospective cohort study. World J Surg Oncol. 2018;16(1):27.
Reisinger KW, Bosmans JW, Uittenbogaart M, et al. Loss of skeletal muscle mass during neoadjuvant chemoradiotherapy predicts postoperative mortality in esophageal cancer surgery. Ann Surg Oncol. 2015;22(13):4445–52.
Elliott JA, Docherty NG, Eckhardt HG, et al. Weight loss, satiety, and the postprandial gut hormone response after esophagectomy: a prospective study. Ann Surg. 2017;266(1):82–90.
Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008;33(5):997–1006.
Yoshizumi T, Shirabe K, Nakagawara H, et al. Skeletal muscle area correlates with body surface area in healthy adults. Hepatol Res. 2014;44(3):313–8.
Prado CM, Lieffers JR, McCargar LJ, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008;9(7):629–35.
Sobin LH, Compton CC. TNM seventh edition: what’s new, what’s changed: communication from the International Union Against Cancer and the American Joint Committee on Cancer. Cancer. 2010;116(22):5336–9.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Martin L, Lagergren J, Lindblad M, Rouvelas I, Lagergren P. Malnutrition after oesophageal cancer surgery in Sweden. Br J Surg. 2007;94(12):1496–500.
Harada K, Yoshida N, Baba Y, et al. Pyloroplasty may reduce weight loss 1 year after esophagectomy. Dis Esophagus. 2018. https://doi.org/10.1093/dote/dox127.
Park SY, Kim DJ, Suh JW, Byun GE. Risk factors for weight loss 1 year after esophagectomy and gastric pull-up for esophageal cancer. J Gastrointest Surg. 2018;22(7):1137–43.
Doki Y, Takachi K, Ishikawa O, et al. Ghrelin reduction after esophageal substitution and its correlation to postoperative body weight loss in esophageal cancer patients. Surgery. 2006;139(6):797–805.
Miyazaki T, Tanaka N, Hirai H, et al. Ghrelin level and body weight loss after esophagectomy for esophageal cancer. J Surg Res. 2012;176(1):74–8.
Liu J, Xie X, Zhou C, Peng S, Rao D, Fu J. Which factors are associated with actual 5-year survival of oesophageal squamous cell carcinoma? Eur J Cardio-thoracic Surg. 2012;41(3):e7–11.
Martin L, Birdsell L, Macdonald N, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013;31(12):1539–47.
Harimoto N, Shirabe K, Yamashita YI, et al. Sarcopenia as a predictor of prognosis in patients following hepatectomy for hepatocellular carcinoma. Br J Surg. 2013;100(11):1523–30.
Liu J, Motoyama S, Sato Y, et al. Decreased skeletal muscle mass after neoadjuvant therapy correlates with poor prognosis in patients with esophageal cancer. Anticancer Res. 2016;36(12):6677–85.
Huang DD, Ji YB, Zhou DL, et al. Effect of surgery-induced acute muscle wasting on postoperative outcomes and quality of life. J Surg Res. 2017;218:58–66.
Takamori S, Toyokawa G, Okamoto T, et al. Clinical impact and risk factors for skeletal muscle loss after complete resection of early non-small cell lung cancer. Ann Surg Oncol. 2018;25(5):1229–36.
Tsukioka T, Izumi N, Kyukwang C, et al. Loss of muscle mass is a novel predictor of postoperative early recurrence in N2-positive non-small-cell lung cancer. Ann Thorac Cardiovasc Surg. 2018;24(3):121–6.
Miyake M, Morizawa Y, Hori S, et al. Clinical impact of postoperative loss in psoas major muscle and nutrition index after radical cystectomy for patients with urothelial carcinoma of the bladder. BMC Cancer. 2017;17(1):237.
Fukushima H, Nakanishi Y, Kataoka M, Tobisu KI, Koga F. Postoperative changes in skeletal muscle mass predict survival of patients with metastatic renal cell carcinoma undergoing cytoreductive nephrectomy. Clin Genitourinary Cancer. 2017;15(2):e229–38.
Takeda Y, Akiyoshi T, Matsueda K, et al. Skeletal muscle loss is an independent negative prognostic factor in patients with advanced lower rectal cancer treated with neoadjuvant chemoradiotherapy. PloS One. 2018;13(4):e0195406.
Mayanagi S, Tsubosa Y, Omae K, et al. Negative impact of skeletal muscle wasting after neoadjuvant chemotherapy followed by surgery on survival for patients with thoracic esophageal cancer. Ann Surg Oncol. 2017;24(12):3741–7.
George J, Cannon T, Lai V, et al. Cancer cachexia syndrome in head and neck cancer patients: Part II. Pathophysiology. Head Neck. 2007;29(5):497–507.
Baracos VE. Cancer-associated cachexia and underlying biological mechanisms. Ann Rev Nutr. 2006;26:435–61.
Guttridge DC, Mayo MW, Madrid LV, Wang CY, Baldwin AS, Jr. NF-kappaB-induced loss of MyoD messenger RNA: possible role in muscle decay and cachexia. Sci (New York, NY). 2000;289(5488):2363–6.
Sorensen J. Lung cancer cachexia: can molecular understanding guide clinical management? Integrative Cancer Ther. 2018;17(3):1000–8.
Rice TW, Ishwaran H, Hofstetter WL, et al. Esophageal cancer: associations with (pN+) lymph node metastases. Ann Surg. 2017;265(1):122–9.
Boshier PR, Ziff C, Adam ME, Fehervari M, Markar SR, Hanna GB. Effect of perioperative blood transfusion on the long-term survival of patients undergoing esophagectomy for esophageal cancer: a systematic review and meta-analysis. Dis Esophagus. 2018. https://doi.org/10.1093/dote/dox134.
Pedersen BK, Febbraio MA. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat Rev Endocrinol. 2012;8(8):457–65.
Tidball JG. Regulation of muscle growth and regeneration by the immune system. Nat Rev Immunol. 2017;17(3):165–78.
Froghi F, Sanders G, Berrisford R, et al. A randomised trial of post-discharge enteral feeding following surgical resection of an upper gastrointestinal malignancy. Clin Nutr (Edinburgh, Scotland). 2017;36(6):1516–9.
Healy LA, Ryan A, Doyle SL, et al. Does prolonged enteral feeding with supplemental omega-3 fatty acids impact on recovery post-esophagectomy: results of a randomized double-blind trial. Ann Surg. 2017;266(5):720–8.
Temel JS, Abernethy AP, Currow DC, et al. Anamorelin in patients with non-small-cell lung cancer and cachexia (ROMANA 1 and ROMANA 2): results from two randomised, double-blind, phase 3 trials. Lancet Oncol. 2016;17(4):519–31.
Nakamura M, Nakamori M, Ojima T, et al. The effects of rikkunshito on body weight loss after esophagectomy. J Surg Res. 2016;204(1):130–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Fig. 1
Study population (TIFF 619 kb)
Supplemental Fig. 2
The method to assess skeletal muscle mass (green area); skeletal muscle index = skeletal muscle mass/height2 (cm2/m2) (TIFF 2186 kb)
Rights and permissions
About this article
Cite this article
Takahashi, K., Watanabe, M., Kozuki, R. et al. Prognostic Significance of Skeletal Muscle Loss During Early Postoperative Period in Elderly Patients with Esophageal Cancer. Ann Surg Oncol 26, 3727–3735 (2019). https://doi.org/10.1245/s10434-019-07616-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07616-0