Abstract
Background
Recent studies indicate that women with unilateral breast cancer are choosing contralateral prophylactic mastectomy (CPM) at an increasing rate. There is limited literature evaluating the postoperative complication rates associated with CPM without breast reconstruction. The objective of this study was to compare postoperative complications in women undergoing unilateral mastectomy (UM) and sentinel lymph node biopsy (SLNB) to those undergoing bilateral mastectomy (BM) and SLNB for the treatment of their breast cancer.
Methods
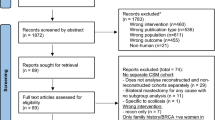
The American College of Surgeons National Surgery Quality Improvement Program (ACS NSQIP) Participant Use Files between 2007 and 2010 were used to identify women with breast cancer undergoing UM or BM with SLNB. Individual and composite end points of 30-day complications were used to compare both groups by univariate and multivariate analyses.
Results
We identified 4,219 breast cancer patients who had a SLNB: 3,722 (88.2 %) had UM and 497 (11.8 %) had BM. The wound complication rate was significantly higher in the BM group versus the UM group, 5.8 % versus 2.9 % [unadjusted odds ratio (OR) 2.1, 95 % confidence interval (CI) 1.3–3.3, P < 0.01]. The overall 30-day complication rate in UM patients was 4.2 % versus 7.6 % in the BM group (unadjusted OR 1.9, 95 % CI 1.3–2.7, P < 0.01). The adjusted OR for overall complications adjusting for important patient characteristics was 1.9 (95 % CI 1.3–2.8, P < 0.01). Independent predictors of overall postoperative complications were body mass index (OR 1.1, P < 0.01) and smoking (OR 2.2, P < 0.01).
Conclusions
For patients with breast cancer, bilateral mastectomy is associated with an increased risk of wound and overall postoperative complications. Discussion of these outcomes is imperative when counseling women contemplating CPM.
Similar content being viewed by others
References
Cemal Y, Alboroz CR, Disa JJ, et al. A paradigm shift in US breast reconstruction: part 2. The influence of changing mastectomy patterns on reconstructive rate and method. Plastic Reconstr Surg. 2013;131:320–6.
Tuttle TM, Habermann EB, Grund EH, Morris TJ, Virnig BA. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol. 2007;25:5203–9.
Tuttle TM, Jarosek S, Habermann EB, Arrington A, et al. Increasing rates of contralateral prophylactic mastectomy among patients with ductal carcinoma in situ. J Clin Oncol. 2009;27:1362–7.
Van Sprundel TC, Schmidt MK, Rookus MA, et al. Risk reduction of contralateral breast cancer and survival after contralateral prophylactic mastectomy in BRCA1 or BRCA2 mutation carriers. Br J Cancer. 2005;93:287–92.
Healey EA, Cook EF, Orav EJ, et al. Contralateral breast cancer: clinical characteristics and impact on prognosis. J Clin Oncol. 1993;11:1545–52.
Gao X, Fisher SG, Emami B. Risk of second primary cancer in the contralateral breast in women treated for early-stage breast cancer: a population-based study. Int J Radiat Oncol Biol Phys. 2003;15;56:1038–45.
Nicols HB, Berrington de Gonzalez A, Lacey JV Jr, Rosenberg PS, Anderson WF. Declining incidence of contralateral breast cancer in the United States from 1975 to 2006. J Clin Oncol. 2011;29:1564–9.
Stucky CC, Gray RJ, Wasif N, Dueck AC, Pockaj BA. Increase in contralateral prophylactic mastectomy: echoes of a bygone era? Surgical trends for unilateral breast cancer. Ann Surg Oncol. 2010;17 3:330–7.
Fisher CS, Martin-Dunlap T, Ruppel MB, et al. Fear of recurrence and perceived survival benefit are primary motivators for choosing mastectomy over breast conservation therapy regardless of age. Ann Surg Oncol. 2012;19:3246–50.
Zion SM, Slezak JM, Sellers TA, et al. Reoperations after prophylactic mastectomy with or without implant reconstruction. Cancer. 2003;98:2152–60.
Barton MB, West CN, Liu IL, et al. Complications following bilateral prophylactic mastectomy. J Natl Cancer Inst Monogr. 2005;35:61–6.
Birkmeyer JD, Shahian DM, Dimick JB, et al. Blueprint for a new American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2008;207:777–82.
Cohen ME, Dimick JB, Bilimoria KY, Ko CY, Richards K, Hall BL. Risk adjustment in the American College of Surgeons National Surgical Quality Improvement Program: a comparison of logistic versus hierarchical modeling. J Am Coll Surg. 2009;209:687–93.
Shiloach M, Frencher S, Steeger J, et al. Towards robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210:6–16.
Davis GB, Peric M, Chan LS, Wong AK, Sener SF. Identifying risk factors for surgical site infections in mastectomy patients using the National Surgical Quality Improvement Program database. Am J Surg. 2013;205:194–9.
Xue DQ, Qian C, Yang L, Wang XF. Risk factors for surgical site infections after breast surgery: a systematic review and meta-analysis. Eur J Surg Oncol. 2012;38:375–81.
Decker MR, Greenblatt DY, Havlena J, Wilke LG, Greenberg CC, Neuman HB. Impact of neo-adjuvant chemotherapy on wound complications after breast surgery. Surgery. 2012;152:382–8.
El-Tamer MB, Ward BM, Schifftner T, Neumayer L, Khuri S, Henderson W. Morbidity and mortality following breast cancer surgery in women: national benchmarks for standards of care. Ann Surg. 2007;245:665–71.
Arrington AK, Jarosek SL, Virnig BA, Habermann EB, Tuttle TM. Patient and surgeon characteristics associated with increased use of contralateral prophylactic mastectomy in patients with breast cancer. Ann Surg Oncol. 2009;16:2697–704.
Khan NA, Quan H, Bugar JM, Lemaire JB, Brant R, Ghali WA. Association of postoperative complications with hospital costs and length of stay in a tertiary care center. J Gen Intern Med. 2006;21:177–80.
Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA Jr. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199:531–7.
Lohrisch C, Paltiel C, Gelmon K, et al. Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. J Clin Oncol. 2006;24:4888–94.
Shannon C, Ashley S, Smith IE. Does timing of adjuvant chemotherapy for early breast cancer influence survival? J Clin Oncol. 2003;21:3792–7.
Cold S, Düring M, Ewertz M, Knoop A, Møller S. Does timing of adjuvant chemotherapy influence the prognosis after early breast cancer? Results of the Danish Breast Cancer Cooperative Group (DBCG). Br J Cancer. 2005;93:627–32.
Colleoni M, Bonetti M, Coates AS, et al. Early start of adjuvant chemotherapy may improve treatment outcome for premenopausal breast cancer patients with tumors not expressing estrogen receptors. The International Breast Cancer Study Group. J Clin Oncol. 2000;18:584–90.
Hershman DL, Wang X, McBride R, Jacobson JS, Grann VR, Neugut AI. Delay of adjuvant chemotherapy initiation following breast cancer surgery among elderly women. Breast Cancer Res Treat. 2006;99:313–21.
Disclosures
Drs. Osman, Saleh, Jackson, Corrigan and Cil have no financial affiliations to disclose. No external sources of funding were used for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclaimer: American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Rights and permissions
About this article
Cite this article
Osman, F., Saleh, F., Jackson, T.D. et al. Increased Postoperative Complications in Bilateral Mastectomy Patients Compared to Unilateral Mastectomy: An Analysis of the NSQIP Database. Ann Surg Oncol 20, 3212–3217 (2013). https://doi.org/10.1245/s10434-013-3116-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-013-3116-1