Abstract
Background
This study evaluated use of circumferential resection margin status in preoperative MRI (mrCRM) as an indication for neoadjuvant radiochemotherapy (nRCT) in rectal carcinoma patients.
Materials and Methods
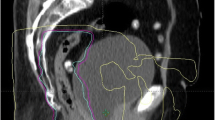
In a multicenter prospective study, nRCT was given to patients with carcinoma of the middle rectum with positive mrCRM (≤1 mm), with cT3 low rectal carcinoma, and all patients with cT4 tumors. The short-term endpoints were pathologic pCRM (≤1 mm) as a strong predictor of local recurrence rate and the quality of total mesorectal excision according to the plane of surgery. These endpoints were compared in patients with and without nRCT.
Results
Of 230 patients that met the inclusion criteria, 96 (41.7%) received a long course of nRCT and 134 (58.3%) were primarily operated on. The pCRM was positive in 13 of 230 (5.7%) (primarily operated on, 2 of 134 [1.5%]; after nRCT, 11 of 96 [11%]). In 1 of 134 (0.7%) case, the mrCRM was falsely negative. Patients at participating centers varied in terms of preoperative stage but not in pCRM positivity (0%–13%, P = .340). The plane of surgery was mesorectal (good) in 209 of 230 (90.9%), intramesorectal (moderate) in 16 of 230 (7%), and the muscularis propria plane (poor) in 2.2% (5 of 230).
Conclusions
Low pCRM positivity and the high quality of mesorectal excision support use of MRI-based nRCT in rectal carcinoma. nRCT was avoidable in 45% of patients with stage II and III disease without significant risk of undertreatment. Preoperative MRI thus allows identification of patients with high risk of local recurrence and use of selective nRCT.
Similar content being viewed by others
References
Sauer R, Becker H, Hohenberger W, et al. Preoperative chemoradiotherapy as compared with postoperative chemoradiotherapy for locally advanced rectal cancer. N Engl J Med. 2004;351:11–20.
Augestad K, Lindsetmo RO, Stulberg J, Reynolds H, Senagore A, Champagne B, et al. International preoperative rectal cancer management: staging, neoadjuvant treatment and impact of multidisciplinary teams. World J Surg. 2010;34;2689–700.
Swedish Rectal Cancer Trial. Improved survival with preoperative radiotherapy in resectable rectal cancer. New Engl J Med. 1997;336:980–7.
Peeters KCMJ, Marijnen CAM, Nagtegaal ID, Kranenbarg EK, Putter H, Wiggers T, et al. The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg. 2007;246:693–701.
Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S, et al. Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet. 2009;373:811–20.
Engstrom PF, Arnoletti JP, Benson AB III, Chen YJ, Choti MA, Cooper HS, et al. NCCN clinical practice guidelines in oncology: rectal cancer. J Natl Compr Canc Netw. 2009;7:838–81.
Van Cutsem E, Dicato M, Haustermans K, Arber N, Bosset JF, Cunningham D, et al. The diagnosis and management of rectal cancer: expert discussion and recommendations derived from the 9th World Congress in Gastrointestinal Cancer, Barcelona, 2007. Ann Surg Oncol. 2008;19(Suppl 16):vi1–vi8.
Bakx R, Emous M, Legemate DA, Zoetmulder FAN, von Tienhoven G, Bemelman WA, et al. Harm und benefits of short-term pre-operative radiotherapy in patients with resectable rectal carcinomas. EJSO. 2006;32:520–6.
Glynne-Jones R, Mawdsley S, Novell JR. The clinical significance oft the circumferential resection margin following preoperative pelvic chemo-radiotherapy in rectal cancer: why we need a common language. Colorect Dis. 2006;8:800–7.
Glynne-Jones R, Mawdsley S, Pearce T, Buyse M. Alternative clinical endpoints in rectal cancer—are we getting closer? Ann Oncol. 2006;17:1239–48.
Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment for rectal cancer? J Clin Oncol. 2008;26:303–12.
Strassburg J, Junginger T, Trinh T, Püttcher O, Oberholzer K, Heald RJ, et al. Magnetic resonance imaging (MRT-)based indication for neoadjuvant treatment of rectal carcinoma and the surrogate endpoint CRM status. Int J Colorect Dis. 2008;23:1099–107.
MERCURY Study Group. Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observation study. Br Med J. 2006;333:779–82.
Daniels IR, Fisher SE, Heald RJ, Moran BJ. Accurate staging, selective preoperative therapy and optimal surgery improves outcome in rectal cancer. A review of the recent evidence. Colorect Dis. 2007;9:290–301.
Smith N, Brown G. Preoperative staging of rectal cancer. Acta Oncol. 2008;47:20–31.
Shibab OC, Moran BJ, Heald RJ, Quirke P, Brown G. MRI staging of low rectal cancer. Eur Radiol. 2009:19:643–50.
Hermanek P, Hohenberger W, Fietkau R, Rödel C. Individualized magnetic resonance imaging-based neoadjuvant chemoradiation for middle and lower rectal carcinoma. Colorect Dis. 2011;13:39–47.
UICC (2002) Sobin LH, Wittekind Ch, editors. TNM classification of malignant tumors. 6th ed. New York: Wiley-Liss; 2002.
Brown G, Daniels IR. Preoperative staging of rectal cancer: the MERCURY research project. Recent Results Cancer Res. 2005;165:58–74.
Brown G, Daniels IR, Richardson C, Revell F, Pepperson D, Bourne M. Techniques and trouble-shooting in high spatial resolution thin slice MRI for rectal cancer. Br J Radiol. 2005;78:245–51.
Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal surgery—the clue to pelvic recurrence? Br J Surg. 1982;69:613–6.
Nagtegaal ID, van de Velde CJH, Marijnen CAM, van Krieken JH, Quirke P. Low rectal cancer: a call for a change of approach in abdominoperineal resection. J Clin Oncol. 2005;23:9257–64.
Quirke P, Morris E. Reporting colorectal cancer. Histopathology. 2007;50:103–12.
Maughan NJ, Quirke P. Modern management of colorectal cancer—a pathologist’s view. Scand J Surg. 2003;92:11–9.
Merkel S, Hohenberger W, Hermanek P. Intra-operative local tumor cell dissemination in rectal carcinoma surgery: effect of operation principles and neoadjuvant therapy. Chirurg. 2010;81:719–27.
Quirke P, Dixon MF. The prediction of local recurrence in rectal adenocarcinoma by histopathological examination. Int J Colorect Dis. 1988;3:127–31.
Chambers W, Collins G, Warren B, Cunningham C, Mortensen N, Lindsey I. Benchmarking circumferential resection margin (R1) resection rate for rectal cancer in the neoadjuvant era. Colorectal Dis. 2010;12:909–13.
Burton S, Brown G, Daniels IR, Norman AR, Mason B, Cunningham. MRI directed multidisciplinary team preoperative treatment strategy: the way to eliminate positive circumferential margins? Brit J Cancer. 2006;94:351–7.
Quirke P, Steele R, Monson J, Grieve R, Khanna S, Couture J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG C016 randomised clinical trial. Lancet. 2009;373;821–8.
Nagtegaal ID, van de Velde CJH, van der Worp E, Kapiteijn E, Quirke P, van Krieken JHJM. Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol. 2002;20:1729–34.
Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP, et al. Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg. 2002;235:449–57.
Hermanek P, Merkel S, Fietkau R, Rödel C, Hohenberger W. Regional lymph node metastasis and locoregional recurrence of rectal carcinoma in the era of TME surgery. Implications for treatment decisions. Int J Colorect Dis. 2010;25:359–68.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Strassburg, J., Ruppert, R., Ptok, H. et al. MRI-Based Indications for Neoadjuvant Radiochemotherapy in Rectal Carcinoma: Interim Results of a Prospective Multicenter Observational Study. Ann Surg Oncol 18, 2790–2799 (2011). https://doi.org/10.1245/s10434-011-1704-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-011-1704-5