Abstract
Background
Despite improvements in surgery and chemotherapy, most patients develop recurrence after hepatectomy for metastatic colorectal cancer. Data are lacking on the effect of these patterns on outcome.
Methods
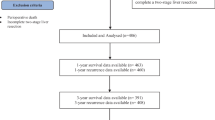
A retrospective review of a prospectively maintained hepatobiliary database was performed. Pattern and timing of recurrence and outcome after recurrence were analyzed. Univariate and multivariate analyses of factors associated with outcome after recurrence were carried out.
Results
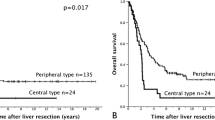
From January 1997 through May 2003, a total of 733 patients underwent hepatectomy for colorectal metastases. Of these, 637 patients (87%) were included in the analysis, and in 393 patients (62%), recurrence was documented at the time of last follow-up. Initial recurrence patterns included the following: liver only in 120 patients (31%), lung only in 107 (27%), other single sites in 49 (12%), and multiple sites in 117 (30%). Recurrence occurred within 2 years of hepatectomy in 75% of patients and after 3 years in 11%. Margins at hepatectomy, recurrence pattern, resected recurrence, and disease-free interval from time of colectomy to hepatic metastasis and from time of hepatectomy to recurrence were independently associated with survival as measured from the time of recurrence. Recurrence in the lung, resected recurrence, and time to recurrence after hepatectomy were associated with prolonged survival as measured from the time of hepatectomy and the time of recurrence.
Conclusions
The timing and pattern of recurrence after hepatic resection for metastatic colorectal cancer are important predictors of long-term survival.



Similar content being viewed by others
References
Jemal A, Murray T, Ward E, et al. Cancer statistics 2005. CA Cancer J Clin. 2005;55:10–30.
Fong Y, Fortner J, Sun R, et al. Clinical Score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 1999;230:309–30.
Scheele J, Stang R, Altendorf-Hofmann A, et al. Resection of colorectal liver metastases. World J Surg. 1995;19:59–71.
Nordlinger B, Guiguet M, Vaillant JC, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Cancer. 1996;77:1254–62.
Choti MA, Sitzmann JV, Tiburi MF, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg. 2002;235:759–66.
Fortner JG. Recurrence of colorectal cancer after hepatic resection. Am J Surg. 1988;155:378–82.
Hughes KS, Simon R, Songhorabodi S, et al. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of patterns of recurrence. Surgery. 1986;100:278–84.
Fong Y, Cohen AM, Fortner JG, et al. Liver resection for colorectal metastases. J Clin Oncol. 1997;15:938–46.
Bozzetti F, Doci R, Bignami P, et al. Patterns of failure following surgical resection of colorectal cancer liver metastases. Rationale for a multimodal approach. Ann Surg. 1987;205:264–70.
Topal B, Kaufmann L, Aerts R, et al. Patterns of failure following curative resection of colorectal liver metastases. Eur J Surg Oncol. 2003;29:248–53.
Metcalfe M, Mann C, Mullin E, et al. Detecting curable disease following hepatectomy for colorectal metastases. ANZ J Surg. 2005;75:524–7.
Ueno H, Mochizuki H, Hashiguchi Y, et al. Predictors of extrahepatic recurrence after resection of colorectal liver metastases. Br J Surg. 2004;91:327–33.
Mutsaerts ELAR, van Ruth S, Zoetmulder FAN, et al. Prognostic factors and evaluation of surgical management of hepatic metastases from colorectal origin: a 10-year single-institute experience. J Gastrointest Surg. 2005;9:178–86.
Takahashi S, Inoue K, Konoshi M, et al. Prognostic factors for poor survival after repeat hepatectomy in patients with colorectal liver metastases. Surgery. 2003;133:627–34.
Petrowsky H, Gonen M, Jarnagin W, et al. Second liver resections are safe and effective treatment for recurrent hepatic metastases from colorectal cancer. A bi-institutional analysis. Ann Surg. 2002;235:863–71.
Adam R, Bismuth H, Castaing D, et al. Repeat hepatectomy for colorectal liver metastases. Ann Surg. 1997;225:51–62.
Headrick JR, Miller DL, Nagorney DM, et al. Surgical treatment of hepatic and pulmonary metastases from colon cancer. Ann Thorac Surg. 2001;71:975–9.
Jarnagin WR, Gonen M, Fong Y, et al. Improvement in perioperative outcome after hepatic resection. Ann Surg. 2002;236:397–407.
Goldsmith NA, Woodburne RT. The surgical anatomy pertaining to liver resection. Surg Gynecol Obstet. 1957;105:310–8.
Hohenberger P, Schlag P, Schwarz V, et al. Tumor recurrence and options for further treatment after resection of liver metastases in patients with colorectal cancer. J Surg Oncol. 1990;44:245–51.
Pawlik TM, Scoggins CR, Zorzi D, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005;241:715–24.
Cady B, Jenkins RL, Steele GD, et al. Surgical margin in hepatic resection for colorectal metastasis: a critical and improvable determinant of outcome. Ann Surg. 1998;227:566–71.
Yamada H, Kondo S, Okushiba S, et al. Analysis of predictive factors for recurrence after hepatectomy for colorectal liver metastases. World J Surg. 2001;25:1129–33.
Tanaka T, Shimada H, Fujii Y, et al. Pre-hepatectomy prognostic staging to determine treatment strategy for colorectal cancer metastases to the liver. Langenbecks Arch Surg. 2004;389:371–9.
Kemeny N, Huang Y, Cohen AM, et al. Hepatic arterial infusion of chemotherapy after resection of hepatic metastases from colorectal cancer. N Engl J Med. 1999;341:2039–48.
Weitz J, Koch M, Kienle P, et al. Detection of hematogenic tumor cell dissemination in patients undergoing resection of liver metastases of colorectal cancer. Ann Surg. 2000;232:66–72.
Patel H, Le Marer N, Wharton RQ, et al. Clearence of circulating tumor cells after excision of primary colorectal cancer. Ann Surg. 2002;235;226–31.
CONFLICT OF INTEREST
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
D’Angelica, M., Kornprat, P., Gonen, M. et al. Effect on Outcome of Recurrence Patterns After Hepatectomy for Colorectal Metastases. Ann Surg Oncol 18, 1096–1103 (2011). https://doi.org/10.1245/s10434-010-1409-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-010-1409-1