Abstract
Background
The global burden of pancreatic cancer has steadily increased, while the prognosis after pancreatic cancer diagnosis remains poor. This study aims to compare the stage- and age-specific pancreatic cancer net survival (NS) for seven high-income countries: Australia, Canada, Denmark, Ireland, New Zealand, Norway, and United Kingdom.
Methods
The study included over 35,000 pancreatic cancer cases diagnosed during 2012–2014, followed through 31 December 2015. The stage- and age-specific NS were calculated using the Pohar-Perme estimator.
Results
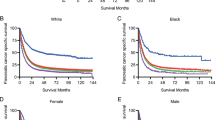
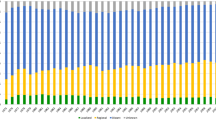
Pancreatic cancer survival estimates were low across all 7 countries, with 1-year NS ranging from 21.1% in New Zealand to 30.9% in Australia, and 3-year NS from 6.6% in the UK to 10.9% in Australia. Most pancreatic cancers were diagnosed with distant stage, ranging from 53.9% in Ireland to 83.3% in New Zealand. While survival differences were evident between countries across all stage categories at one year after diagnosis, this survival advantage diminished, particularly in cases with distant stage.
Conclusion
This study demonstrated the importance of stage and age at diagnosis in pancreatic cancer survival. Although progress has been made in improving pancreatic cancer prognosis, the disease is highly fatal and will remain so without major breakthroughs in the early diagnosis and management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
This study is based on cancer registry data provided by registries participating in ICBP SURVMARK-2 project. Data are owned by cancer registries and authors are not permitted to share these data externally except in aggregate form, e.g. publication. Any data request should be directed to each corresponding cancer registry.
References
International Agency for Research on Cancer. Global Cancer Observatory. http://gco.iarc.fr/ (2020).
Arnold M, Abnet CC, Neale RE, Vignat J, Giovannucci EL, McGlynn KA, et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology. 2020;159:335.e5–49.e5.
Global Burden of Disease Study (GBD) Pancreatic Cancer Collaborators. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2019;4:934–47.
McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS, et al. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2018;24:4846–61.
Arnold M, Rutherford MJ, Bardot A, Ferlay J, Andersson TM, Myklebust TA, et al. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995–2014 (ICBP SURVMARK-2): a population-based study. Lancet Oncol. 2019;20:1493–505.
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Niksic M, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–75.
Conroy T, Hammel P, Hebbar M, Ben Abdelghani M, Wei AC, Raoul JL, et al. FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N. Engl J Med. 2018;379:2395–406.
Jang JY, Han Y, Lee H, Kim SW, Kwon W, Lee KH, et al. Oncological benefits of neoadjuvant chemoradiation with gemcitabine versus upfront surgery in patients with borderline resectable pancreatic cancer: a prospective, randomized, open-label, multicenter phase 2/3 trial. Ann Surg. 2018;268:215–22.
Latenstein AEJ, van der Geest LGM, Bonsing BA, Groot Koerkamp B, Haj Mohammad N, de Hingh I, et al. Nationwide trends in incidence, treatment and survival of pancreatic ductal adenocarcinoma. Eur J Cancer. 2020;125:83–93.
Ahola R, Sand J, Laukkarinen J. Centralization of pancreatic surgery improves results: review. Scand J Surg. 2020;109:4–10.
Latenstein AEJ, Mackay TM, van der Geest LGM, van Eijck CHJ, de Meijer VE, Stommel MWJ, et al. Effect of centralization and regionalization of pancreatic surgery on resection rates and survival. Br J Surg. 2021;108:826–33.
Gooiker GA, Lemmens VE, Besselink MG, Busch OR, Bonsing BA, Molenaar IQ, et al. Impact of centralization of pancreatic cancer surgery on resection rates and survival. Br J Surg. 2014;101:1000–5.
Huang L, Jansen L, Balavarca Y, Babaei M, van der Geest L, Lemmens V, et al. Stratified survival of resected and overall pancreatic cancer patients in Europe and the USA in the early twenty-first century: a large, international population-based study. BMC Med. 2018;16:125.
Madley-Dowd P, Hughes R, Tilling K, Heron J. The proportion of missing data should not be used to guide decisions on multiple imputation. J Clin Epidemiol. 2019;110:63–73.
Ro C, Chai W, Yu VE, Yu R. Pancreatic neuroendocrine tumors: biology, diagnosis,and treatment. Chin J Cancer. 2013;32:312–24.
Cabasag CJ, Arnold M, Piñeros M, Morgan E, Brierley J, Hofferkamp J, et al. Population-based cancer staging for oesophageal, gastric, and pancreatic cancer 2012–2014: International Cancer Benchmarking Partnership SurvMark-2. Int J Cancer. 2021. https://doi.org/10.1002/ijc.33679.
US Preventive Services Task Force. Screening for Pancreatic Cancer: US Preventive Services Task Force Reaffirmation Recommendation Statement. JAMA. 2019;322:438–44.
Klein AP. Identifying people at a high risk of developing pancreatic cancer. Nat Rev Cancer. 2013;13:66–74.
Del Chiaro M, Segersvard R, Lohr M, Verbeke C. Early detection and prevention of pancreatic cancer: is it really possible today? World J Gastroenterol. 2014;20:12118–31.
Tas F, Sen F, Keskin S, Kilic L, Yildiz I. Prognostic factors in metastatic pancreatic cancer: older patients are associated with reduced overall survival. Mol Clin Oncol. 2013;1:788–92.
He J, Edil BH, Cameron JL, Schulick RD, Hruban RH, Herman JM, et al. Young patients undergoing resection of pancreatic cancer fare better than their older counterparts. J Gastrointest Surg. 2013;17:339–44.
Amin S, Lucas AL, Frucht H. Evidence for treatment and survival disparities by age in pancreatic adenocarcinoma: a population-based analysis. Pancreas. 2013;42:249–53.
Conroy T, Desseigne F, Ychou M, Bouche O, Guimbaud R, Becouarn Y, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N. Engl J Med. 2011;364:1817–25.
Williet N, Saint A, Pointet AL, Tougeron D, Pernot S, Pozet A, et al. Folfirinox versus gemcitabine/nab-paclitaxel as first-line therapy in patients with metastatic pancreatic cancer: a comparative propensity score study. Ther Adv Gastroenterol. 2019;12:1756284819878660.
Latenstein AEJ, Mackay TM, Creemers GJ, van Eijck CHJ, de Groot JWB, Haj Mohammad N, et al. Implementation of contemporary chemotherapy for patients with metastatic pancreatic ductal adenocarcinoma: a population-based analysis. Acta Oncol. https://doi.org/10.1080/0284186X.2020.1725241 (2020).
Versteijne E, Suker M, Groothuis K, Akkermans-Vogelaar JM, Besselink MG, Bonsing BA, et al. Preoperative chemoradiotherapy versus immediate surgery for resectable and borderline resectable pancreatic cancer: results of the Dutch randomized phase III PREOPANC trial. J Clin Oncol. 2020;38:1763–73.
Makar M, Worple E, Dove J, Hunsinger M, Arora T, Oxenberg J, et al. Disparities in care: impact of socioeconomic factors on pancreatic surgery: exploring the National Cancer Database. Am Surg. 2019;85:327–34.
Wennervaldt K, Kejs AM, Lipczak H, Bartels P, Borre M, Fristrup CW, et al. Regional variation in surgery for pancreatic cancer in Denmark 2011–2015. Dan Med J. 2018;65:A5503.
Cancer Council. Optimal care pathway for people with pancreatic cancer. https://www.cancer.org.au/ocp (2021).
Reames BN, Blair AB, Krell RW, Groot VP, Gemenetzis G, Padussis JC, et al. Management of locally advanced pancreatic cancer: results of an international survey of current practice. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003568.
Andersson TM, Rutherford MJ, Myklebust TA, Moller B, Soerjomataram I, Arnold M, et al. Exploring the impact of cancer registry completeness on international cancer survival differences: a simulation study. Br J Cancer. 2021;124:1026–32.
Rutherford MJ, Moller H, Lambert PC. A comprehensive assessment of the impact of errors in the cancer registration process on 1- and 5-year relative survival estimates. Br J Cancer. 2013;108:691–8.
Bray F, Ferlay J. Chapter 5: Data comparability and quality. In: Bray F, et al. editors. CI5: cancer incidence in five continents, volume XI. Lyon: International Agency for Research on Cancer; 2017. p. 101–19.
Yadav S, Sharma P, Zakalik D. Comparison of demographics, tumor characteristics, and survival between pancreatic adenocarcinomas and pancreatic neuroendocrine tumors: a population-based study. Am J Clin Oncol 2018;41:485–91.
Genus TSE, Bouvier C, Wong KF, Srirajaskanthan R, Rous BA, Talbot DC, et al. Impact of neuroendocrine morphology on cancer outcomes and stage at diagnosis: a UK nationwide cohort study 2013–2015. Br J Cancer. 2019;121:966–72.
Acknowledgements
The authors would like to thank the ICBP management team of Cancer Research UK for managing the programme, the ICBP SURVMARK-2 Local Leads for advice to understand the data, for their contributions to the study protocol, and interpretation of the results, as well as, the ICBP Clinical Committees for their advice. We are grateful to the ICBP SurvMark-2 Academic Reference Group for providing independent peer review and advice for the study protocol and analysis plan development. Finally, we thank the ICBP Program Board for their oversight and direction. A complete list of all investigators can be found in Supplementary Information Table 8. ICBP is funded by the Canadian Partnership Against Cancer; Cancer Council Victoria; Cancer Institute New South Wales; Cancer Research UK; Danish Cancer Society; National Cancer Registry Ireland; The Cancer Society of New Zealand; NHS England; Norwegian Cancer Society; Public Health Agency Northern Ireland on behalf of the Northern Ireland Cancer Registry; DG Health and Social Care, Scottish Government; Western Australia Department of Health; Public Health Wales NHS Trust.
Author information
Authors and Affiliations
Contributions
Conceptualisation: CJC, IS, FB, and MA; data curation: MA, AB, and JF; formal analysis and visualisation: CJC and MR; funding acquisition: IS, FB, and MA; roles/writing—original draft: CJC; writing—review and editing: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the IARC Ethics Committee, and where needed approval was also given by local (or national) ethical committees. This study was conducted according to the guidelines of the Declaration of Helsinki and used secondary cancer data from the cancer registries, thus not requiring individual re-consenting for the purpose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Cabasag, C.J., Arnold, M., Rutherford, M. et al. Pancreatic cancer survival by stage and age in seven high-income countries (ICBP SURVMARK-2): a population-based study. Br J Cancer 126, 1774–1782 (2022). https://doi.org/10.1038/s41416-022-01752-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01752-3
This article is cited by
-
Short-term serial circulating tumor DNA assessment predicts therapeutic efficacy for patients with advanced pancreatic cancer
Journal of Cancer Research and Clinical Oncology (2024)
-
Erhöhter Blutzucker und Gewichtsverlust: Frühzeichen für ein Pankreaskarzinom
Schweizer Gastroenterologie (2023)