Abstract
All living organisms have evolutionarily adapted themselves to the Earth’s gravity, and failure to adapt to gravity changes may lead to pathological conditions. This perspective may also apply to abnormal aging observed in bedridden elderly patients with aging-associated diseases such as osteoporosis and sarcopenia. Given that bedridden elderly patients are partially analogous to astronauts in that both cannot experience the beneficial effects of gravity on the skeletal system and may suffer from bone loss and muscle weakness, one may wonder whether there are gravity-related mechanisms underlying diseases among the elderly. In contrast to numerous studies of the relevance of microgravity in skeletal disorders, little attention has been paid to neurodegenerative diseases. Therefore, the objective of this paper is to discuss the possible relevance of microgravity in these diseases. We particularly noted a proteomics paper showing that levels of hippocampal proteins, including β-synuclein and carboxyl-terminal ubiquitin hydrolase L1, which have been linked to familial neurodegenerative diseases, were significantly decreased in the hippocampus of mice subjected to hindlimb suspension, a model of microgravity. We suggest that microgravity-induced neurodegeneration may be further exacerbated by diabetes and other factors. On the basis of this view, prevention of neurodegenerative diseases through ‘anti-diabetes’ and ‘hypergravity’ approaches may be important as a common therapeutic approach on Earth and in space. Collectively, neurodegenerative diseases and space medicine may be linked to each other more strongly than previously thought.
Similar content being viewed by others
Introduction
In our aging society, an increasing number of elderly people are becoming bedridden owing to frailty derived from age-related disorders, such as osteoporosis and sarcopenia. As these patients are forced to be in a supine-immobilized posture combined with no axial loading, they cannot experience the beneficial effects of gravity on the skeletal system.1 Accordingly, they are often compared with astronauts who suffer from muscle weakness and bone fragility upon return to Earth because their skeletal systems are not used to microgravity and degenerate in space. Thus, geriatrics and space medicine, two seemingly different fields, may be linked to each other.
There have been numerous studies of the effect of microgravity on degeneration of the skeletal system,2,3 but few on the relevance of microgravity to age-related neurodegenerative diseases, such as Alzheimer’s disease (AD) and Parkinson’s disease (PD). However, it is recognized empirically that dementia in elderly patients may accelerate after they become bedridden. If skeletal unloading in bedridden patients is partially analogous to the effect of microgravity in space, then there is a possibility that neurodegenerative disease may be accelerated in astronauts.
In this paper, we discuss the possible relevance of microgravity in neurodegenerative disease. First, neurons may be predisposed to degenerate under microgravity, based on a proteomics paper showing marked changes in protein expression levels in the hippocampus of mice subjected to hindlimb suspension.4 In addition, microgravity-induced neurodegeneration may be amplified by cosmic rays5 and other factors, such as alteration of behaviors and diabetes, in space. We propose that preventive strategies for neurodegenerative diseases will be important on Earth and in space.
Mouse hindlimb suspension as a model for neurodegeneration in space
To investigate the effect of microgravity on protein expression in the hippocampus, Sarkar et al.4 carried out a proteomic analysis on hippocampal tissues from mice subjected to hindlimb suspension. Interestingly, the levels of some proteins that are abundantly expressed in the normal hippocampus were significantly decreased4 (Figure 1a). These proteins included β-synuclein (βS), the non-amyloidogenic homolog of α-synuclein (αS), which has a central role in PD and related neurodegenerative diseases.6 Neurodegeneration in mice expressing αS is ameliorated by cross-breeding with mice expressing αS and βS,7 and viral delivery of βS reduces neurodegeneration in mice expressing αS.8 Moreover, the ratio of βS to αS at the mRNA level is significantly decreased in post-mortem brains of patients with PD, dementia with Lewy bodies, and AD, compared with the ratio in control brains.9 These results suggest that loss of function of βS may be involved in the pathogeneses of neurodegenerative diseases.
A hypothetical mechanism for promotion of neurodegenerative disease by microgravity. (a) In response to microgravity, expression of proteins in the hippocampus, including β-synuclein, ubiquitin carboxyterminal hydrolase L1 (UCHL1), pyruvate dehydrogenase, and tubulin, may result in enhanced protein aggregation, mitochondrial dysregulation, and impairment of the cytoskeleton, leading to initiation or stimulation of neurodegenerative diseases. (b) Neurodegeneration induced by microgravity may be potentiated by factors such as diabetes, altered behaviors and cosmic rays in space.
Expression of carboxyl-terminal ubiquitin hydrolase L1 (UCHL1) was also decreased in mice after hindlimb suspension4 (Figure 1a). UCHL1 is a deubiquitinating enzyme that is critical in recycling of ubiquitin, and impairment of this molecule has been implicated in various neurodegenerative diseases, including AD, PD, and Huntington’s disease (HD).10 Notably, a missense mutation of UCHL1 has been linked to an autosomal dominant familial PD (PARK5).11 Furthermore, the UCHL1 gene is naturally deleted in gracile axonal dystrophy (gad) mice, which are characterized by accumulation of βS and γ-synuclein in spheroids in the gracile nucleus of the brain,12,13 suggesting a possible link between βS and UCHL1 in neurodegeneration. Collectively, these findings suggest that dysfunction of UCHL1 may result in impaired proteolysis by the ubiquitin proteasome system, leading to protein aggregation.
Expression levels of other proteins, including pyruvate dehydrogenase and tubulin, were also decreased in the same mice4 (Figure 1a). Pyruvate is the end product of glycolysis in the cytoplasm and is transported into mitochondria to drive ATP production by oxidative phosphorylation.14 Thus, a decrease in pyruvate dehydrogenase may lead to dysregulation of pyruvate metabolism in mitochondria in neurodegenerative diseases. The importance of tubulin in the pathogenesis of neurodegenerative disease is underscored by the fact that mutations of the microtubule-associated protein tau are linked to AD and related tauopathies.15 A decrease in expression of tubulin might reduce neuronal functions and thus stimulate neurodegeneration.
Further studies are needed to elucidate the mechanisms through which the levels of the above proteins are decreased in the hippocampus in the hindlimb suspension model, but the results suggest that neurons may be predisposed to degenerate in response to altered gravity in mouse brain, as protein aggregation, mitochondrial dysfunction, and cytoskeleton disorder are all major pathological phenotypes of neurodegenerative diseases. Given the analogy between bedridden elderly patients and astronauts in microgravity, similar pathogenic mechanisms may underlie neurodegeneration in these populations.
Differential diagnosis of cognitive dysfunction
Impairment of vestibular function is a serious symptom stimulated by time in space1 and is also a neuropathological feature of AD.16 Vestibular dysfunction may influence multiple biological processes, including bone integrity,17 sense of self,18 and even cognition in space;19 therefore, it is difficult to distinguish cognitive dysfunctions due to vestibular effects from neurodegenerative diseases on Earth and in space.
It is also possible that cognitive dysfunction may be stimulated by other non-dementia conditions. These include the relative lack of mental stimulation and motor activity during bed rest, and the relative monotony of sensory stimulation while in a spacecraft, both of which might contribute to neural decline, especially in the cognitive area. Thus, differential diagnosis of dementia is important in space.
Exacerbation of neurodegeneration by other factors in space
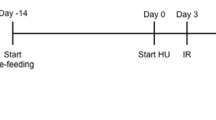
It may be argued that the effects of microgravity on neurodegeneration are too small to be observed as a disease in astronauts. However, even if neurodegeneration induced by microgravity is minimal by itself, it might be potentiated by cosmic rays,5 altered behaviors and diseases such as diabetes in space (Figure 1b).
Concerns have often been raised about the risk of cosmic rays in space.1 In particular, galactic cosmic radiation consisting of high-energy, highly charged particles may pose a significant threat to astronauts. Such cosmic rays may promote development of cancers, as well as neurodegenerative diseases. Indeed, cognitive impairment and Aβ plaque formation have been shown to be enhanced in an AD mouse model irradiated with high-energy 56Fe particles.5 Furthermore, psychological and behavioral changes, such as depression and sleep disorders, are frequently associated with spaceflight,20 and various cohort studies have shown that depression may increase the risk of neurodegenerative diseases, including AD and PD.21,22 Sleep and neurodegenerative disease may influence each other,23 given that the circadian rhythm tends to be irregular in space.1 In this context, it is of a note that the sleep-wake cycle directly influences the Aβ level in the brain.24 An abnormal autonomic nerve reflex also occurs in space, including non-coordinated heart rates, reduction of blood pressure and syncope.25 These symptoms may predispose an individual to neurodegenerative diseases, and symptoms of abnormal autonomic nerve reflex have been described in α-synucleinopathies, such as PD and multiple system atrophy.26
Other diseases might also exacerbate microgravity-induced neurodegeneration on Earth and in space. Among these, diabetes may be of a particular importance (Figure 1b), since it is associated with an increased risk of neurodegenerative diseases, including AD, PD, and HD.27,28 Indeed, several studies suggest that neurodegenerative diseases have aspects of lifestyle diseases and are associated with metabolic dysfunction.27,29 In space, microgravity may stimulate diabetes because it is predicted that muscle atrophy due to microgravity may result in a failure of energy consumption, leading to metabolic dysfunction.
‘Anti-diabetes’ strategies to protect neurons
Given the importance of diabetes on Earth and in space,1 an ‘anti-diabetes’ approach may be a common therapeutic strategy in neurodegenerative disease. In this regard, increasing attention has been paid to the therapeutic potential of anti-diabetic hormones, such as incretins and adiponectin (APN), for neurodegenerative disease. Glucagon-like peptide 1 (GLP-1) is a member of the incretin family that is secreted by the small intestine in response to food intake.30 GLP-1 improves insulin resistance without hypoglycemia,30 and thus may be useful to replace the neuroprotective effects of insulin.31 Analogs of GLP-1, such as exenatide and liraglutide, have been shown to be effective in a pilot study in PD.32,33 These drugs are already used for treatment of type II diabetes mellitus without any side effects.32
Accumulating evidence suggests that APN, a multifunctional adipocytokine,34 may be protective for brain disorders, such as ischemia and depression, in addition to other diseases, including type II diabetes, atherosclerosis, osteoporosis, and chronic pulmonary obstructive disease.35 Owing to the beneficial effects of APN on a wide range of diseases, APN signaling has been suggested as a mimetic of exercise. APN binds to APN receptors, AdipoR1 and AdipoR2,36 and exerts anti-diabetic effects via activation of signaling molecules, including AMPK and PPAR-α.34 As APN receptors are abundant in the brain,36 stimulation of APN signaling may be an approach to prevention of neurodegenerative diseases. In support of the therapeutic potential of APN, we recently showed that APN-ameliorated neuropathological features, such as aggregation of αS and impaired motor function, in a transgenic mouse model of α-synucleinopathies35 (Figure 2). Subsequently, osmotin, the plant homolog of APN, was shown to attenuate Aβ42-induced neurotoxicity and tau hyperphosphorylation in the mouse hippocampus.37 Furthermore, it is of note that AdipoRon, an AdipoR agonist, was isolated as a small molecule that ameliorates diabetes in a genetic mouse model,38 raising the possibility that AdipoR agonists may be promising as therapy for type II diabetes. Similarly, it will be intriguing to determine whether AdipoR agonists are effective for protection against neurodegenerative diseases on Earth and in space.
APN ameliorates neurodegeneration in a mouse model of α-synucleinopathies. (a) Globular APN (gAPN, 0.1 mg/ml in 10 μl phosphate buffered saline (PBS)) or PBS alone (10 μl) was given intranasally to αS transgenic (tg) mice (male, 3 months old) or wild-type littermates every 3 days for 2 months. Motor performance was evaluated by the rotarod test (mean±s.e.m., n=8–9, *P<0.05, **P<0.01). (b) Mice were killed and their brains were analyzed immunohistochemically (anti-phospho-αS). Representative images of the cortex and olfactory bulb are shown. Insets show a higher magnification of the cortex. Reprinted from Sekiyama et al.35 APN, adiponectin.
At this time, follow-up of a large number of astronauts who have been in space for long periods is required to determine whether neurodegenerative diseases are manifested or exacerbated by microgravity in space. Furthermore, it is unclear whether protective drugs against neurodegenerative diseases are needed on a regular basis in space. The astronaut population is thoroughly screened for preexisting conditions, such as diabetes, and regular exercise is successfully performed by most astronauts in space. However, it would be wise to have such an intervention on hand in an emergency or as a contingency, should there be an inability to exercise due to injury or equipment breakdown, or in excursions in small spacecraft without adequate exercise facilities.
‘Hypergravity therapy’ against neurodegenerative diseases?
Given the negative effect of microgravity on aging-associated disorders, including osteoporosis, sarcopenia, and diabetes, it is possible that hypergravity may be beneficial for these disorders (Figure 3). Interestingly, such a concept goes back >200 years to Dr Erasmus Darwin, a British physician who was the grandfather of Charles Darwin.1 Metabolic rates may be upregulated because of increased energy consumption under hypergravity conditions, which may be compared with the beneficial effects of exercise. Therefore, ‘hypergravity therapy’ may be regarded as an ‘anti-diabetes’ strategy. Naturally, a similar view is applicable to prevention of neurodegenerative diseases on Earth and in space. Thus, now is the time for us to demonstrate Darwin’s hypothesis in the therapy of neurodegenerative diseases. In support of ‘hypergravity therapy’, it has been shown that hypergravity may be beneficial in aging diseases, such as bone atrophy39 and ischemia.40 However, hypergravity may also cause side effects, and it has been suggested that the circadian system is disrupted by chronic centrifugation, possibly due to hypergravity.41
A hypothetic model for the effects of gravity on aging-associated diseases. Aging-associated diseases, such as osteoporosis, sarcopenia, diabetes, and neurodegenerative diseases, may be exacerbated under microgravity conditions (e.g., bedridden patients and astronauts), whereas these diseases may be improved by hypergravity (e.g., therapeutic applications). G, gravity.
Conclusions
Given the possibility of long-term stays in space in the near future, improved understanding of microgravity-induced neurodegeneration is important. In particular, an ‘anti-diabetes’ strategy, a current paradigm for therapy of neurodegenerative diseases on Earth, may be applicable to protection against possible neurodegenerative diseases in space. In turn, hypergravity may be promising for treatment of diseases of aging, including neurodegenerative diseases, in space and on Earth. Thus, geriatrics and space medicine may be mutually supportive in the context of treatment of neurodegenerative diseases.
References
Vernikos, J . G-Connection: Harness Gravity and Reverse Aging (iUniverse, Inc.: Lincoln, NE, USA, 2004).
Booth, F. W. Terrestrial applications of bone and muscle research in microgravity. Adv. Space Res. 14, 373–376 (1994).
White, R. J. & Averner, M. Humans in space. Nature 409, 1115–1118 (2001).
Sarkar, P. et al. Proteomic analysis of mice hippocampus in simulated microgravity environment. J. Proteome Res. 5, 548–553 (2006).
Cherry, J. D. et al. Galactic cosmic radiation leads to cognitive impairment and increased abeta plaque accumulation in a mouse model of Alzheimer's disease. PLoS ONE 7, e53275 (2012).
Hashimoto, M. & La Spada, A. R. Review β-synuclein in the pathogenesis of Parkinson's disease and related α-synucleinopathies: emerging roles and new directions Future. Neurology 7, 155–163 (2012).
Hashimoto, M., Rockenstein, E., Mante, M., Mallory, M. & Masliah, E. beta-Synuclein inhibits alpha-synuclein aggregation: a possible role as an anti-parkinsonian factor. Neuron 32, 213–223 (2001).
Hashimoto, M. et al. An antiaggregation gene therapy strategy for Lewy body disease utilizing beta-synuclein lentivirus in a transgenic model. Gene Ther. 11, 1713–1723 (2004).
Rockenstein, E. et al. Altered expression of the synuclein family mRNA in Lewy body and Alzheimer's disease. Brain Res. 914, 48–56 (2001).
Gong, B. & Leznik, E. The role of ubiquitin C-terminal hydrolase L1 in neurodegenerative disorders. Drug News Perspect. 20, 365–370 (2007).
Leroy, E. et al. The ubiquitin pathway in Parkinson's disease. Nature 395, 451–452 (1998).
Saigoh, K. et al. Intragenic deletion in the gene encoding ubiquitin carboxy-terminal hydrolase in gad mice. Nat Genet. 23, 47–51 (1999).
Wang, Y. L. et al. Accumulation of beta- and gamma-synucleins in the ubiquitin carboxyl-terminal hydrolase L1-deficient gad mouse. Brain Res. 1019, 1–9 (2004).
Hitosugi, T. et al. Tyrosine phosphorylation of mitochondrial pyruvate dehydrogenase kinase 1 is important for cancer metabolism. Mol. Cell 44, 864–877 (2011).
Ballatore, C., Lee, V. M. & Trojanowski, J. Q. Tau-mediated neurodegeneration in Alzheimer's disease and related disorders. Nat. Rev. Neurosci. 8, 663–672 (2007).
Nakamagoe, K. et al. Vestibular function impairment in Alzheimer's disease. J. Alzheimers Dis. 47, 185–196 (2015).
Vignaux, G. et al. Bone remodeling is regulated by inner ear vestibular signals. J. Bone Miner. Res. 28, 2136–2144 (2013).
Lenggenhager B., Lopez C . in Open MIND, Vol. 23(T) (eds Metzinger T. & Windt J. M.) (Frankfurt am Main: MIND Group, 2015).
Smith P. F., Zheng Y., Horii A., Darlington C. L. Does vestibular damage cause cognitive dysfunction in humans? J. Vestib. Res. 2005; 15: 1–9.
Basner, M. et al. Psychological and behavioral changes during confinement in a 520-day simulated interplanetary mission to mars. PLoS ONE 9, e93298 (2014).
Weiner, M. W. & Veitch, D. P. Introduction to special issue: overview of Alzheimer's Disease Neuroimaging Initiative. Alzheimers Dement. 11, 730–733 (2015).
Leentjens, A. F. Parkinson disease: depression-risk factor or early symptom in Parkinson disease? Nat. Rev. Neurol. 11, 432–433 (2015).
Videnovic, A., Lazar, A. S., Barker, R. A. & Overeem, S. 'The clocks that time us'--circadian rhythms in neurodegenerative disorders. Nat. Rev. Neurol. 10, 683–693 (2014).
Kang, J. E. et al. Amyloid-beta dynamics are regulated by orexin and the sleep-wake cycle. Science 326, 1005–1007 (2009).
Cox, J. F. et al. Influence of microgravity on astronauts' sympathetic and vagal responses to Valsalva's manoeuvre. J. Physiol. 538, 309–320 (2002).
Pilleri, M. et al. Heart rate circadian profile in the differential diagnosis between Parkinson disease and multiple system atrophy. Parkinsonism Relat. Disord. 20, 217–221 (2014).
Cai, H. et al. Metabolic dysfunction in Alzheimer's disease and related neurodegenerative disorders. Curr. Alzheimer Res. 9, 5–17 (2012).
Mayeux, R. & Stern, Y. Epidemiology of Alzheimer disease. Cold Spring Harb. Perspect. Med. 2, a006239 (2012).
Barnes, D. E. & Yaffe, K. The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol. 10, 819–828 (2011).
Duarte, A. I. et al. Crosstalk between diabetes and brain: glucagon-like peptide-1 mimetics as a promising therapy against neurodegeneration. Biochim. Biophys. Acta 1832, 527–541 (2013).
Craft, S. et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: a pilot clinical trial. Arch. Neurol. 69, 29–38 (2012).
Holscher, C. Potential role of glucagon-like peptide-1 (GLP-1) in neuroprotection. CNS Drugs 26, 871–882 (2012).
Aviles-Olmos, I. et al. Exenatide and the treatment of patients with Parkinson's disease. J. Clin. Invest. 123, 2730–2736 (2013).
Kadowaki, T. & Yamauchi, T. Adiponectin receptor signaling: a new layer to the current model. Cell Metab. 13, 123–124 (2011).
Sekiyama, K. et al. Disease-Modifying Effect of Adiponectin in Model of alpha-Synucleinopathies. Ann. Clin. Transl. Neurol. 1, 479–489 (2014).
Yamauchi, T. et al. Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature 423, 762–769 (2003).
Ali, T., Yoon, G. H., Shah, S. A., Lee, H. Y. & Kim, M. O. Osmotin attenuates amyloid beta-induced memory impairment, tau phosphorylation and neurodegeneration in the mouse hippocampus. Sci. Rep. 5, 11708 (2015).
Okada-Iwabu, M. et al. A small-molecule AdipoR agonist for type 2 diabetes and short life in obesity. Nature 503, 493–499 (2013).
Morita, S. et al. Hypergravity stimulates osteoblast phenotype expression: a therapeutic hint for disuse bone atrophy. Ann. N. Y. Acad. Sci. 1030, 158–161 (2004).
Sang, H. et al. Preconditioning with +Gz acceleration (head-to-foot inertial load) produces neuroprotection against transient focal cerebral ischemia in rats. Neurosci. Lett. 445, 78–82 (2008).
Holley, D. C., DeRoshia, C. W., Moran, M. M. & Wade, C. E. Chronic centrifugation (hypergravity) disrupts the circadian system of the rat. J. Appl. Physiol. 95, 1266–1278 (2003).
Acknowledgements
We are grateful for the encouragement of Kaori Hashimoto (Tokyo Metropolitan Institute of Medical Science), and Eliezer Masliah and Albert R. La Spada (University of California, San Diego). This work was supported in part by a grant-in-aid (Basic Science Research B 25290019) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan.
Author information
Authors and Affiliations
Contributions
YT, WK and MH wrote the paper. TT, SS, JW, MW and KS discussed the idea of the paper. All authors have approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Takamatsu, Y., Koike, W., Takenouchi, T. et al. Protection against neurodegenerative disease on Earth and in space. npj Microgravity 2, 16013 (2016). https://doi.org/10.1038/npjmgrav.2016.13
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/npjmgrav.2016.13
This article is cited by
-
Sarcopenia
Wiener Medizinische Wochenschrift (2019)