Abstract
The interaction between obesity and bone metabolism is complex. The effects of fat on the skeleton are mediated by both mechanical and biochemical factors. Though obesity is characterized by higher bone mineral density, studies conducted on bone microarchitecture have produced conflicting results. The majority of studies indicate that obesity has a positive effect on skeletal strength, even though most likely the effects are site-dependent and, in fact, obese individuals might be at risk of certain types of fractures. Mechanical loading and higher lean mass are associated with improved outcomes, whereas systemic inflammation, observed especially with abdominal obesity, may exert negative effects. Weight loss interventions likely lead to bone loss over time. Pharmacological treatment options seem to be safe in terms of skeletal health; however, the skeletal effects of bariatric surgery are dependent on the type of surgical procedure. Malabsorptive procedures are associated with higher short-term adverse effects on bone health. In this narrative review, we discuss the effects of obesity and weight loss interventions on skeletal health.
Similar content being viewed by others
Introduction
Obesity is becoming a global epidemic, with 2.8 million people estimated to die each year as a result of being overweight or obese [1]. The worldwide prevalence of obesity virtually doubled between 1980 and 2008 and the numbers are expected to increase further. In Europe, more than 20% of men and women were obese in 2008, while, alarmingly, rates of obesity and overweight are very high among children as well [2].
The interaction of obesity with bone metabolism is complex and not as yet fully elucidated. Traditionally, it was thought that obesity, as demonstrated by high body mass index (BMI), has protective effects on the skeleton [3]. BMI is incorporated in the fracture risk assessment tool (FRAX), and higher BMI is associated with lower future fracture risk. However, this notion has recently been challenged, with studies showing that obesity is associated with lower risk for certain fractures but higher risk for others [4]. Results from animal studies have also resulted in conflicting findings. Moreover, medical and surgical management of obesity can also directly affect bone metabolism.
In this narrative review, we discuss the molecular mechanisms associated with the interaction between obesity and the skeleton and discuss the effects of obesity on the risk of fractures and on bone mineral density (BMD). We also review the effects of treatment interventions for obesity on skeletal health.
Pathophysiology
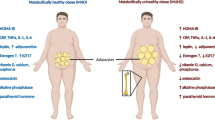
Various molecular pathways have been proposed by which adipose tissue communicates with the bone microenvironment (Fig. 1). This involves systemic factors such as vitamin D, leptin and proinflammatory cytokines, and local factors mainly associated with local changes in the bone marrow microenvironment.
Principal central and peripheral molecular signaling between bone, adipose tissue, and SNSLeptin action has, through the hypothalamus, direct and indirect effects on osteoblast and osteoclast activity that alters bone metabolism. IGF-1 and inflammation increase cortisol response of fat tissue and proinflammatory cytokines, such as TNF-a, and increase cortisol action on bone by increasing the expression of 11β-HSD1. Insulin promotes the differentiation of osteoblasts through the insulin receptor and also promotes the production of osteocalcin. Osteocalcin, a non-collagenous bone matrix protein, regulates energy and glucose metabolism, closing the loop of calcium and glucose metabolism. Inflammation has both systemic and local actions.SNS: sympathetic nervous system, IGF-1: insulin growth factor 1, TNF-a: tumor necrosis factor a, 11β-HSD1: 11β-hydroxysteroid dehydrogenase type 1
Leptin
Leptin, a cytokine-like hormone, is the protein product of the ob (Lep) gene. It is produced primarily by adipocytes and is involved in the regulation of appetite and energy homeostasis by inducing satiety signals in the hypothalamus (Fig. 1). Systemic levels of leptin increase with increased fat content. Leptin plays an important role in bone metabolism with both direct and indirect effects, by peripheral and central (hypothalamic) pathways, though in vivo studies have produced seemingly discrepant results, depending on the experimental design. In vitro, leptin stimulates the differentiation of stromal cells to osteoblasts [5], increases proliferation of osteoblasts, and inhibits osteoclastogenesis, without affecting mature osteoclasts [6]. Deficiency in leptin signaling, through knockout of the leptin receptor gene, decreases bone volume and BMD [7], indicating an important role of leptin in bone homeostasis. In mice, peripheral action through the administration of low doses of leptin seems to promote bone formation, without inducing anorexigenic actions of the hormone to the central nervous system [8]. In animal models, increased leptin levels caused by increased adipose tissue seem to have a protective role in / effect on bone tissue [9]. By contrast, leptin-deficient models have increased cancellous bone volume fraction [10] and increased trabecular content (volume and thickness), indicating a possible antiosteogenic role of leptin [11]. The negative effects of leptin in bone homeostasis seem to be mediated through its central hypothalamic action, as intracerebroventricular infusion of leptin in both leptin-deficient and wild-type mice induces bone loss [12]. This effect seems to be mediated by activation of the sympathetic nervous system (Fig. 1) [13]. Data in humans are also conflicting, indicating either a beneficial role of leptin [14, 15] or a detrimental one [16, 17], this probably being due to limitations of association studies. Moreover, obesity is characterized by leptin tolerance, at least as concerns the hypothalamus, as administration of leptin has not proved to be an effective treatment for obesity [18]. Overall, the high levels of leptin observed in obese individuals are unlikely to have negative effects on bone metabolism.
High-fat diet
There are data from animal studies implying possible negative effects of obesity on bone metabolism. These effects are likely to be mediated through local alterations in the bone microenvironment or through systemic effects of obesity, mainly through inflammation. One of the most commonly used models to study the effects of adiposity on bone metabolism is obesity caused by a high-fat diet (HFD). Trabecular BMD decreased in mice that were fed with HFD [19], while obesity induced by HFD is associated with higher bone tissue quantity but worse bone quality [20]. Obesity induced by HFD causes significant bone resorption [21] and can increase bone marrow adiposity leading to alteration of trabecular architecture. The bone marrow (BM) microenvironment in obesity seems to be associated with bone resorption; meanwhile, accumulation of adipocytes in the BM microenvironment promotes inflammation that leads to increased bone resorption by enhancing osteoclastogenesis and inhibiting osteoblast development [22]. Adiposity is associated with proinflammatory cytokines such as TNF-a and IL-6. TNF-α stimulates osteoclastogenesis via the activation of NFκB in hyperphagia-induced obesity by increasing the expression of c-fms, RANK, and RANKL [23]. Several studies have demonstrated a role of TNF-α in obesity-related bone loss through its enhancement of adipogenesis and osteoclastogenesis and suppression of osteoblastogenesis [24, 25]. In addition, HFD-induced obesity, through IL-6, suppresses osteoblasts, upregulates osteoclasts, and inhibits osteoclast apoptosis [26]. Acetoacetyl-CoA synthetase (AACS) is a ketone body-utilizing enzyme that converts acetoacetate to acetoacetyl-CoA in the cytosol and consequently provides acetyl units as the precursors for lipogenesis [27]. AACS mRNA expression in the adult femur is increased in HFD, in the differentiated osteoclast cells (RAW 264), and upregulated by IL-6 only in osteoclasts. These results indicate that bone resorption is induced by HFD through bone inflammation and increased ketone utilization [28].
11β-hydroxysteroid dehydrogenase type 1
The negative effects of glucocorticoids on bone metabolism are well recognized. 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1) is an enzyme that converts the inactive glucocorticoid cortisone to the active glucocorticoid cortisol and is expressed in both osteoblasts and adipocytes [29]. Its expression is affected by local factors and activation results in higher local exposure to active cortisol. Local activity of 11β-HSD1 is believed to determine the skeletal response to different types of glucocorticoids [30]. The local expression of 11β-HSD1 in osteoblasts is upregulated by proinflammatory cytokines (IL-1β and TNF-a) (Fig. 1) [31]. This constitutes another mechanism by which adipocyte accumulation in the bone marrow can have detrimental effects on bone metabolism.
Visceral adipose tissue (VAT) is metabolically more active than subcutaneous adipose tissue (SAT), and this might be why some human studies have indicated that VAT might be associated with a less favorable skeletal phenotype, though most studies do not find a negative association between SAT and bones.
Vitamin D
Vitamin D deficiency is very common among obese individuals and may have significant implications for skeletal health. Supplementation with vitamin D is more effective in increasing its serum levels in non-obese children and adults compared to obese, possibly due to sequestration of vitamin D in the body fat stores [32, 33]. It has been noted that vitamin D deficiency is common in morbidly obese individuals and up to 43% of those with vitamin D deficiency also suffer from secondary hyperparathyroidism [34].
Conjugated linoleic acids and calcium supplementation
Poor calcium intake during adolescence, especially in the presence of vitamin D deficiency, might contribute to fracture risk; however, obese and overweight adolescents have increased calcium retention (as assessed by calcium intake, fecal, and urinary calcium) when compared with healthy-weight subjects of the same age, and this is correlated positively with calcium intake [35]. In animal models, co-supplementation of conjugated linoleic acids (CLA) and calcium has beneficial effects on bone and energy-related metabolic markers in tibia in obese animals fed with HFD. It prevents bone loss induced by HF feeding and increases the expression of bone formation markers, such as bone gamma-carboxyglutamate protein 2 (Bglap2) and collagen Iα1 (Col1a1) [36].
Fat and bone molecular crosstalk
Interestingly, the crosstalk between fat and bone seems to be more complicated and to also involve effects of bone metabolism on energy homeostasis. In animal models, there are data showing positive effects of calcium on energy homeostasis. Supplementation with CLAs and calcium in adult obese mice decreases body weight and body fat [37, 38]. It also modulates the expression of genes involved in energy metabolism, insulin receptor (Insr), and leptin receptor (Lepr) [36]. Osteocalcin is a bone matrix protein and is considered a marker of bone formation. Animal studies have indicated that the undercarboxylated form of osteocalcin regulates energy homeostasis by enhancing B cell proliferation, insulin secretion, and sensitivity (Fig. 1) [39]. Emerging evidence shows that there is also crosstalk between bone and adipose tissue through central signals. For example, osteoblast-derived lipocalin 2 (LCN2), a protein that was previously known as an adipokine, suppresses appetite and decreases food intake by signaling directly to melanocortin 4 receptor-expressing hypothalamic neurons [40].
Bone density and microarchitecture
Obese individuals have higher BMD than the normal weight population, though it has been postulated that this might be an artifact due to overlying soft tissue. Moreover, the coefficient of variation between repeat measurements is higher in obesity [41] and therefore longitudinal BMD monitoring in obese individuals might be challenging.
BMD measurements using quantitative computed tomography (QCT) and peripheral QCT (pQCT) are not as affected by overlying soft tissue, providing a more reliable way to assess bone density in obesity. Moreover, they provide separate information about the cortical and trabecular compartment of the bone. In a cross-sectional case-control study, it was demonstrated that obese women had higher volumetric BMD (vBMD) at the lumbar spine and that both obese men and women had higher vBMD at the distal radius and distal tibia when compared to normal weight individuals [42]. This suggests that the higher BMD is a true effect and not an artifact caused by overlying soft tissue. Moreover, parameters of bone microarchitecture were better in obese compared to normal weight individuals, suggesting higher skeletal strength.
Lean mass, which is usually higher in obese individuals along with fat mass, correlates positively with BMD and parameters of bone microarchitecture, as measured by pQCT [43, 44]. This is especially relevant to cortical thickness and area, whereas total fat mass has a positive correlation with trabecular number and density even after adjusting for lean mass [44]. It seems that fat mass is not the main contributing factor to increased bone strength, while muscle force (represented by lean mass) is associated with osteogenic adaptation [45]. Fat mass does not seem to have a positive association with BMD in obese adults [46] and adolescents [47]. A case control study has shown that excess weight or higher BMI does not have a proportional positive effect on bone strength parameters. Moreover, lean mass seems to be an important determinant of bone microarchitecture, geometry, and metabolism when compared to fat mass [48].
As VAT is metabolically active and associated with inflammation, there has been growing interest in the differential effects of VAT and SAT. In a study investigating the correlation of visceral fat with skeletal parameters in the peripheral skeleton, VAT was measured using CT scans, and skeletal bone microarchitecture parameters were measured by high-resolution pQCT (HR-pQCT) at the distal radius and tibia. The investigators found that higher visceral fat was associated with higher BMD and improved microarchitecture with the exception of higher cortical porosity at the distal radius. When findings were adjusted for BMI, they were no longer significant, suggesting that the effect is mostly associated with obesity in general rather than with visceral fat [49].
In contrast, in another study examining the correlation of VAT with vBMD using data from CT scans, researchers found that VAT had an inverse correlation with vBMD at the spine and that there was an inverse correlation with low muscle attenuation (a marker of fat infiltration in the muscle) even after adjusting for age, sex, and BMI [50].
The trabecular bone score (TBS) is a dual-energy x-ray absorptiometry (DXA)-derived variable which has a good correlation with bone microarchitecture and predicts vertebral fracture risk independent of BMD [51]. However, TBS seems to be affected by overlying soft tissue [52]. TBS has been shown to have a negative correlation with body size variables, and this correlation is higher for waist circumference than for other variables and for trunk fat mass [53, 54]. However, the latter finding is probably not reflective of higher fracture risk. In older men, obesity variables were positively associated with lumbar spine vBMD, but had a negative correlation with TBS, while the association between vBMD and TBS was variable and depended significantly on BMI and lean trunk mass [55]. It is therefore postulated that TBS might not predict fracture risk in individuals with high BMIs or high trunk lean mass as accurately as in normal weight subjects.
It has been postulated that the effects of fat on the skeleton might differ according to age and that they might have more pronounced negative effects during growth. In a pQCT study in girls post- adolescence where girls were divided into groups according to the percentage body fat rather than their weight, the girls with higher fat content were found to have lower total CSA and cortical CSA and lower bone strength after adjusting for body weight [56]. In a longitudinal study in adolescents, VAT was inversely associated with bone strength at the tibia and radius, as measured by pQCT, in girls but not in boys, and the association was more significant for younger rather than older girls, indicating that early obesity might have more pronounced effects on bone accrual [57].
In young adults with a history of early onset severe obesity at a young age, both obese men and women had improved bone parameters as compared to normal weight controls, but after adjustment for BMI, the findings were attenuated [58]. However, obese men had lower radius cross-sectional area after adjustment for BMI. Interestingly, even though as expected, obese individuals had lower levels of physical activity, there was no correlation between bone parameters and physical activity. Overall, these findings suggest that obesity during skeletal growth might interrupt the skeletal adaptation to mechanical forces. This might either be associated with decreased physical activity in obese individuals, with direct effects of fat on bone metabolism, or come about through negative effects on the muscles. Interestingly, in young girls, researchers found a negative association between SAT and bone strength in the weight bearing tibia, and this finding was correlated with higher fat infiltration in the calf and thigh muscles [59].
Obesity is associated with low bone turnover as measured by bone turnover markers [60]. To our knowledge, there are no histomorphometric data on bone mineralization in obese humans, apart from occasional reports showing abnormal mineralization compatible with mild osteomalacia, these, however, in the context of vitamin D deficiency and secondary hyperparathyroidism [61]. Data from animal studies indicate that obesity induced by HFD, despite inducing higher bone mass probably caused by an increase in mechanical loading, leads to reduced bone formation [62]. This is associated with an increase in bone marrow adiposity. In histomorphometric studies, obesity has been shown to induce lower osteoblast surface, osteoid surface, and osteoid volume, indicating low osteoblastic activity, though with no change in the mineralization process [63].
In conclusion, the existing data seem to differ depending on the technique employed to estimate BMD and microarchitecture and the methods used to assess fat mass, VAT and SAT, age, and bone compartment (cortical vs trabecular). In general, obesity results in higher BMD and improved bone microarchitecture parameters, albeit it might be associated with negative effects (mostly VAT), especially during bone accrual, resulting in impaired adaptation of the skeleton to the increased weight.
Fracture risk in obesity
Data regarding fracture risk in obese people are somewhat contradictory (Table 1). Originally, it was thought that fracture rates in obese individuals were lower compared to normal weight individuals due to the higher areal BMD (aBMD) and local fat padding. The association of BMI with fracture risk, however, is more complex and seems to be different depending on the skeletal site [64, 65]. Data from a multisite, multiethnic cohort of 1924 women were analyzed and demonstrated that obesity is associated with increased aBMD but lower bone strength relative to load, with increased fracture hazard and increased impact forces in falls [66]. Higher applied loads from higher body weight may contribute to increased fracture risk during certain activities [67].
In a study in older men (> 65 years), it was demonstrated that overweight/obese men had a lower risk of hip, clinical vertebral, and upper limb fractures, although there was no association between BMI and the risk for proximal humerus and tibial fractures [65]. However, it should be noted that in the above study, the control group consisted of men with BMI < 25 kg/m2; therefore, men with lower BMI and thus higher fracture risk were apparently included. In a large, multinational, prospective study of postmenopausal women, obese women were shown to have a higher risk of ankle and upper leg fractures and a lower risk of wrist fractures as compared to non-obese women [4].
In a meta-analysis of 25 prospective cohorts, including 398,610 women with an average age of 63 years and a follow-up for approximately 2.26 million person-years, it was demonstrated that even though osteoporotic fractures as a whole were observed less often in obese compared to non-obese women (HR 0.85, 95% CI 0.82–0.88), upper arm fractures were observed more often, while there was no association between BMI and lower leg fractures [64]. As previously demonstrated, low BMI was associated with a higher risk of all osteoporotic fractures but was, however, protective against lower leg fractures. The differences in the effects of obesity at different skeletal sites are thought to be related to differences in the pattern of falls and the characteristics of mechanical forces induced by a fall. However, it should be noted that differences among studies might also be related to the control population. Including subjects with low BMI as controls might mask the increased fracture risk associated with obesity or increased risk for certain fractures.
Interestingly, differences in fat distribution seem to be important for skeletal health. Two separate recent meta-analyses showed that abdominal obesity might in fact be associated with higher hip fracture rates [68, 69]. Higher waist circumference and higher waist to hip ratio conferred a higher risk of hip fracture and individuals with a waist circumference higher than 105 cm had a 55% higher risk by comparison with those with a waist circumference of less than 80 cm [68]. The differential effects of visceral fat and subcutaneous fat to systemic inflammation might be the causal factor behind this finding.
Effects of weight loss interventions on bone
Diet
The effects of restricted diet (RD) on body composition and musculoskeletal health in middle-aged obese female rats were evaluated and show that RD after prolonged HFD has a detrimental impact on bone matrix, remodeling, and microstructure (suppressed bone formation and increased bone resorption), probably through decreased insulin-like growth factor-1 and leptin, elevated adiponectin and proinflammatory mechanisms (increased expression of TNF-α messenger RNA) [70].
Diet-induced weight loss in obese patients is accompanied by increased bone loss [71, 72]. It is also associated with an increase in markers of bone formation (serum osteocalcin) and bone resorption (serum N-telopeptide of type I collagen, pyridinoline, deoxypyridinoline) [73]. Another interesting finding is that a history of chronic dieting behavior is associated with detrimental effects on bone health, even in obese women [74]. Weight loss is associated with higher calcium intake requirements. In a study evaluating true fractional calcium absorption, women randomized to energy-restricted diet for weight loss had lower calcium absorption compared to women randomized to a weight maintenance diet [75].
Conversely, in premenopausal women, mild-to-moderate weight reduction for a period of 3 months did not seem to have detrimental effects on bone strength, as assessed by pQCT [76], even after a 9-month weight maintenance period [77]. Moreover, during a 1-year weight loss maintenance program following weight loss by restricted-energy-diet, there were no negative effects on BMD and bone mineral content (BMC) [78].
Potential strategies to avoid bone loss associated with diet-induced weight loss include higher calcium intake and exercise. Energy restriction is associated with reduced urinary calcium excretion; however, a high-protein diet rich in calcium prevents increases in bone resorption markers and minimizes bone loss when compared to a high-protein diet alone [79]. In healthy overweight premenopausal women who lost 7.2 ± 3.3% of body weight (5.5 ± 3.2 kg) after 6 months, intake of 1 g Ca/day prevented bone loss and intake 1.8 g Ca/day increased BMD [80].
Exercise during weight loss
In animal models, exercise during weight loss seems to protect from bone loss. Combinations of diet and exercise appear to be of great importance for losing weight without affecting bone mass [81]. The moderate intensity exercise improved the tibia BMD of obese rats and was associated with preservation of microarchitecture parameters as compared to weight loss alone. Another study has shown that the voluntary wheel running exercise under a high-fat diet increases metaphyseal trabecular density and decreases marrow cavity, while eventually decreasing maximum flexure load in the femoral neck, this showing the complex interaction between physical activity and obesity [82]. Moderate treadmill exercise reduced the body weight of obese Zucker rats without causing significant differences in femoral or tibial bone mass [83].
In humans, the data are somewhat contradictory. A 1-year randomized, controlled trial showed that exercise training with diet-induced weight loss cannot prevent hip bone loss and the associated high bone turnover [84]. These changes persist after partial weight regain independently of continued weight-bearing aerobic exercise [85]. However, in another randomized trial, older obese individuals who lost weight with a combination of diet and exercise rather than diet alone did not exhibit increases in bone turnover, and this was associated with an attenuation of the observed hip BMD loss [86]. Even though it seems that exercise is unlikely to be enough to prevent bone loss induced by weight loss, it seems that it attenuates the effects of weight loss and should therefore be encouraged alongside weight management strategies in order to minimize bone loss.
Pharmacological management of obesity
Orlistat, a gastrointestinal lipase inhibitor, an agent that has been approved for the treatment of obesity for many years, had no significant effect on biomarkers of bone formation and resorption when given for 21 days to obese men [87]. A relative increase in bone resorption but no changes in bone mass and density were observed when it was administered for 1 year [88].
Liraglutide is a GLP-1 analog, initially licensed for the management of T2DM, that was recently licensed both by the Food and Drug Administration (FDA) and European Medicines Agency (EMA) for the management of obesity, albeit at a different dose (3 mg daily) to that used to treat T2DM. There are some data on the effects of liraglutide on bone metabolism in both animal and human studies. In animal studies, liraglutide has been shown to exert anabolic effects on bone [89, 90]. In humans, in a randomized control trial, liraglutide (1.2 mg) was administered for 52 weeks in healthy obese women after achieving weight loss of 12% with a low-calorie diet [91]. Administration of liraglutide resulted in preservation of BMC and increase in bone formation markers as compared to the control group that experienced loss of BMC and no change in bone formation. Both the liraglutide and control groups maintained their initial weight loss. In two different meta-analyses of RCTs conducted in patients with T2DM (and using the lower dose), the use of liraglutide was associated with either similar or lower risk of fractures compared to controls [92, 93]. Even though there are no data on skeletal effects from the weight loss studies with liraglutide, results so far are reassuring.
A combination of phentermine and topiramate is licensed by the FDA for the treatment of obesity in the USA. The effects of the combination on bone metabolism have not been investigated in trials; however, its use has been associated with metabolic acidosis [94] which could potentially have negative effects on bones. This is a theoretical concern and investigations into the issue are warranted.
Lorcacerin is a 5-HT2C receptor agonist approved by the FDA for the treatment of obesity. In a double-blind, randomized, placebo-controlled trial, lorcacerin had no effects on total BMC and total BMD [95].
A combination of naltrexone hydrochloride and bupropion hydrochloride is approved for obesity by the FDA and EMA. To date, there are no data on its effects on bone metabolism.
Bariatric surgery
Bariatric surgery leads to weight loss by restricting the capacity of the stomach (restricting procedures) or causing malabsorption of calories and nutrients (malabsorptive procedures), or by a combination of both. In addition, bariatric procedures often cause hormonal changes which are thought to promote weight loss. There are four major types of bariatric surgery, Roux-en-Y gastric bypass (RYGB), laparoscopic adjustable gastric banding (AGB), sleeve gastrectomy (SG), and duodenal switch with biliopancreatic diversion. These procedures lead to different results, especially as regards average excess weight loss and the improvement of obesity-related comorbidities. Bariatric surgery patients show rapid weight reduction for the first 4 months following surgery. Slower weight loss is observed for the remaining follow-up of 4 years.
Gastric bypass and sleeve gastrectomy are associated with greater initial weight reduction rate than gastric banding [96]. Trends in body weight post-surgically show that patients undergoing RYGB exhibit the greatest weight loss, patients undergoing SG experience less weight loss and patients undergoing AGB have the least weight loss [97].
Several studies have investigated the effects of bariatric surgery on BMD and bone turnover markers. The results are somewhat conflicting as regards investigation of bone loss after bariatric surgery, and again, there are differences among the types of procedures and methods of BMD measurement, while there are also differences associated with baseline vitamin D and parathyroid function status.
Effects of bariatric surgery on bone turnover
Bariatric surgery has been associated with increased bone turnover [98, 99]. RYGB in morbidly obese patients increases bone resorption 1-year postoperatively [100] and this is independent of weight loss [101]. Bone resorption can predict bone loss, a longitudinal study having demonstrated that morbidly obese patients have an increase in bone resorption markers as early as 3 months after RYGB associated with a decrease in BMD after 9 months [98]. Bone resorption is increased also after LSG, as demonstrated by a significant increase in N-telopeptide crosslinks (NTx) [102]. Marked weight loss after long limb-biliopancreatic diversion (BPD-LL) increases bone turnover [103] and increases in bone turnover are associated with percentage of lost BMI in patients who underwent biliopancreatic diversion [104].
Effects of bariatric surgery on BMD
A decrease in BMD occurred during weight loss in morbidly obese patients undergoing vertical banded gastroplasty (VBG). The change in BMD was evident 1 year post-surgery and was associated with the degree of weight reduction [105]. The marked weight loss after long limb-biliopancreatic diversion (BPD-LL) has been associated with decrease in BMD 1 year after surgery [103], RYGB in morbidly obese patients decreases BMC and BMD 1 year postoperatively [106] and, similarly, in a study with follow-up for a year after gastric bypass surgery there was total hip BMD decrease as well as at the lumbar spine [107]. Fewer data are available for the relatively newer sleeve gastrectomy. A longitudinal study shows that laparoscopic sleeve gastrectomy (LSG) may lead to a significant decline in BMD at the spine and proximal femur [71] and in a study comparing the effects of RYGB and SG on age- and BMI-matched morbidly obese women, BMD at the femoral neck and the lumbar spine 1 year after bariatric surgery was similar between the two groups [108], suggesting that even if SG is not a typical malabsorptive procedure, it might have effects that are similar to RYGB. In contrast, in another 2-year follow-up study of patients undergoing LSG, a significant increase in BMD of the lumbar spine was demonstrated mainly during the first year post-surgery [109]. However, in this study, patients at baseline had vitamin D deficiency and secondary hyperparathyroidism which were corrected during follow-up. In a meta-analysis of studies evaluating LS and FN BMD post-bariatric surgery, it was shown that bariatric surgery was associated with lower FN but not LS BMD [110]. As DXA can be affected by overlying soft tissue, it has been suggested that weight loss can result in factitious loss of BMD. In a study comparing QCT and DXA post-RYGB, there was loss of LS BMD with both modalities, whereas at the femur, the loss of aBMD observed with DXA was not confirmed with QCT [111]. Studies in the peripheral skeleton using HR-pQCT indicate that post-bariatric surgery, the cortical compartment of bone is affected and this results in decreased bone strength, which is more significant for the tibia than for the radius [112, 113]. In longer follow-up studies (2 years), even though cortical bone loss stabilized after 12 months, further deterioration in trabecular parameters was observed at 24 months [114]. Results, however, have not been unanimous, with occasional studies showing preservation of bone strength [115].
Effects of bariatric surgery on fracture risk
There are some data concerning the effects of bariatric surgery on fracture risk, with most studies reporting a higher risk of fracture post-surgery [116,117,118]. The type of surgical procedure seems to play a very important role, malabsorptive procedures being associated with a higher risk and restrictive ones having minimal, if any, effect on the risk of fracture [116, 118].
In a historical cohort of patients who had undergone bariatric surgery (mostly gastric bypass, a malabsorptive procedure), a 2.3-fold risk of any fracture was demonstrated after a median follow-up of 7.7 years [117]. Interestingly, there was no correlation between the pre-operative history of fracture and fracture risk post-surgery, indicating that the higher risk was not due to a higher baseline risk but rather to the effect of the bariatric procedure itself. A study with a mean follow-up of 4.8 years, in which most patients had undergone a restrictive procedure, a 1.21-fold risk of any fracture was observed post-surgery, while there was a trend towards more fractures around 1 to 2 years after the procedure [116]. Another study showed a change in the pattern of fractures post-bariatric surgery, shifting from a pattern typically associated with obesity with a high risk of distal lower limb fractures and lower risk of upper limb fractures to a pattern associated with osteoporosis and more fractures of the upper limb, vertebral pelvic, hip, and femur [118]. A single study did not demonstrate any difference in the rates of fracture between patients who had undergone bariatric surgery and controls; however, in this study, mean follow-up was only 2.2 years [119]. Moreover, the most common procedure was AGB (60% of patients).
Patients who had undergone RYGB exhibited a 43% higher risk of non-vertebral fractures compared to patients who had undergone AGB, and the higher risk was observed at least 2 years post-surgery [120].
Mechanisms of skeletal effects of bariatric surgery and prevention strategies
Possible explanations for the bone loss post-bariatric surgery include unloading, malabsorption of calcium and vitamin D with secondary hyperparathyroidism, malabsorption of other nutrients, and alteration in the gut hormone profile. Bone loss after surgery for morbid obesity could be an adaptation of the skeleton to the reduction of mechanical loading [121], and this is why in studies evaluating the peripheral skeleton the effects of bariatric surgery are more pronounced in the weight bearing tibia. This is probably the mechanism underlying the changes seen after purely restrictive procedures. However, in malabsorptive procedures, nutrient deficiency and secondary hyperparathyroidism probably play a significant role. Low serum 25OHD levels and poor absorption of calcium seem to be related to secondary hyperparathyroidism observed in women who had undergone RYGB [122], and there is association between changes in the cortical bone parameters and changes in PTH post-surgery [112]. A 6-month prospective clinical trial in obese patients who underwent RYGB showed a decrease in Ca absorption without alteration of the Ca-PTH axis, suggesting the implication of other regulating hormones [123].
Early studies have shown that jejunoileal bypass (end-to-side jejunoileostomy) for the management of morbid obesity increases the possibility of 25OHD deficiency, with vitamin D supplementation restoring it to normal levels [124], while others observed that vitamin D levels returned to postoperative levels without the need for supplementation, possibly due to much higher mobilization of fat stores [125].
Serum OPG levels negatively correlated with the bone remodeling markers osteocalcin, β-CTX, and P1NP, suggesting a possible role of the OPG/RANKL system in bone metabolism after biliopancreatic diversion or laparoscopic RYGB [126]. Sclerostin, an endogenous inhibitor of the Wnt pathway which plays an important role in bone formation and remodeling, is correlated with the ongoing loss of BMD and this is independent of the type of bariatric surgery (RYGB or SG) [127]. The increase in the sclerostin levels could in theory be due to unloading from weight loss; however, interestingly, marked increases were observed from the first month post-surgery and were independent of weight loss.
Lifelong adequate supplementation with calcium and vitamin D after malabsorptive procedures is extremely important. Also, as with diet-induced weight loss, there have been some attempts to attenuate bone loss with physical exercise. In a 24-month, randomized, controlled study evaluating the effects of an intervention including a combination of high vitamin D and calcium supplementation with exercise post-bariatric surgery, the intervention group had attenuated increase in bone turnover markers and less pronounced bone loss as compared with the non-intervention group [128]. In another study, a weight-bearing and aerobic exercise intervention program post-bariatric surgery resulted in less pronounced bone loss which was associated with preservation of muscle mass [129].
The American Association of Clinical Endocrinologists (AACE), The Obesity Society (TOS), and the American Society for Metabolic and Bariatric Surgery (ASBMS) guidelines recommend supplementation with vitamin D, at least 3000 IU per day. Preoperative determination of calcium is preferred and supplementation with 1200–1500 mg of essential, dietary, or citrate, calcium is also recommended [130].
Conclusions
The relationship between obesity and bone metabolism is complex and includes several factors. Mechanical loading, as expected, exerts positive effects; however, low-grade systemic inflammation is potentially harmful. Effects might differ depending on the age and children, and adolescents are probably at higher risk of negative effects. Weight loss interventions are very important to treat obesity, and strategies to prevent the associated bone loss are needed.
Abbreviations
- 11β-HSD1:
-
11β-hydroxysteroid dehydrogenase type 1
- 5-HT2C:
-
5-hydroxytryptamine 2c
- AACE:
-
American Association of Clinical Endocrinologists
- AACS:
-
acetoacetyl-CoA synthetase
- aBMD:
-
areal bone mineral density
- AGB:
-
adjustable gastric band
- ASBMS:
-
American Society for Metabolic and Bariatric Surgery
- Bglap2:
-
bone gamma-carboxyglutamate protein 2
- BM:
-
bone marrow
- BMC:
-
bone mineral content
- BMI:
-
body mass index
- BPD-LL:
-
long limb-biliopancreatic diversion
- Ca:
-
calcium
- c-fms:
-
colony-stimulating factor
- CLA:
-
conjugated linoleic acid
- Col1a1:
-
collagen Iα1
- CSA:
-
cross-sectional area
- CT:
-
computed tomography
- DXA:
-
dual energy x-ray absorptiometry
- EMA:
-
European Medicines Agency
- FDA:
-
Food and Drug Administration
- FN:
-
femoral neck
- FRAX:
-
Fracture Risk Assessment Tool
- HFD:
-
high-fat diet
- HR-pQCT:
-
high-resolution pQCT
- IGF-1:
-
insulin-like growth factor-1
- IL-6:
-
interleukin 6
- Insr:
-
insulin receptor
- LCN2:
-
lipocalin 2
- Lepr:
-
leptin receptor
- LS:
-
lumbar spine
- LSG:
-
laparoscopic sleeve gastrectomy
- MC4R:
-
melanocortin 4 receptor
- NFκB:
-
nuclear factor kappa-light-chain-enhancer of activated B cells
- NTx:
-
N-telopeptide crosslinks
- OPG:
-
osteoprotegerin
- pQCT:
-
peripheral QCT
- QCT:
-
quantitative computed tomography
- RANK:
-
receptor activator of nuclear factor kappa-B
- RANKL:
-
RANK ligand
- RD:
-
restricted diet
- RYGB:
-
Roux-en-Y gastric bypass
- SAT:
-
subcutaneous adipose tissue
- T2DM:
-
type 2 diabetes mellitus
- TBS:
-
trabecular bone score
- TNFα:
-
tumor necrosis factor-a
- TOS:
-
The Obesity Society
- VAT:
-
visceral adipose tissue
- VBG:
-
vertical banded gastroplasty
- vBMD:
-
volumetric BMD
- β-CTX:
-
beta C-terminal telopeptide
References
World Health Organization Global Health Observatory. Obesity:situation and trends. 2017. http://www.who.int/gho/ncd/risk_factors/obesity_text/en/.
European Association for the Study of Obesity. Facts & Statistics: Definitions of overweight and obese. 2017. http://easo.org/task-forces/childhood-obesity-cotf/facts-statistics/.
De Laet C, Kanis JA, Oden A et al (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int England 16:1330–1338
Compston JE, Watts NB, Chapurlat R et al (2011) Obesity is not protective against fracture in postmenopausal women: GLOW. Am J Med United States 124:1043–1050
Thomas T, Gori F, Khosla S, Jensen MD, Burguera B, Riggs BL (1999) Leptin acts on human marrow stromal cells to enhance differentiation to osteoblasts and to inhibit differentiation to adipocytes 1. Endocrinology 140:1630–1638
Cornish J, Callon KE, Bava U et al (2002) Leptin directly regulates bone cell function in vitro and reduces bone fragility in vivo. J Endocrinol 175:405–415
Bao D, Ma Y, Zhang X et al (2015) Preliminary characterization of a leptin receptor knockout rat created by CRISPR/Cas9 system. Sci Rep England 5:15942
Philbrick KA, Wong CP, Branscum AJ, Turner RT, Iwaniec UT (2017) Leptin stimulates bone formation in Ob/Ob mice at doses having minimal impact on energy metabolism. J Endocrinol England 232:461–474
de Albuquerque Maia L, Lisboa PC, de Oliveira E et al (2014) Bone metabolism in obese rats programmed by early weaning. Metabolism United States 63:352–364
Turner RT, Philbrick KA, Wong CP, Olson DA, Branscum AJ, Iwaniec UT (2014) Morbid obesity attenuates the skeletal abnormalities associated with leptin deficiency in mice. J Endocrinol England 223:M1–M15
Vaira S, Yang C, McCoy A et al (2012) Creation and preliminary characterization of a leptin knockout rat. Endocrinology United States 153:5622–5628
Ducy P, Amling M, Takeda S et al (2000) Leptin inhibits bone formation through a hypothalamic relay: a central control of bone mass. Cell United States 100:197–207
Hamrick MW, Ferrari SL (2008) Leptin and the sympathetic connection of fat to bone. Osteoporos Int England 19:905–912
Pasco JA, Henry MJ, Kotowicz MA et al (2001) Serum leptin levels are associated with bone mass in nonobese women. J Clin Endocrinol Metab United States 86:1884–1887
Yamauchi M, Sugimoto T, Yamaguchi T et al (2001) Plasma leptin concentrations are associated with bone mineral density and the presence of vertebral fractures in postmenopausal women. Clin Endocrinol (Oxf) England 55:341–347
Ruhl CE, Everhart JE (2002) Relationship of serum leptin concentration with bone mineral density in the United States population. J Bone Miner Res United States 17:1896–1903
Odabasi E, Ozata M, Turan M et al (2000) Plasma leptin concentrations in postmenopausal women with osteoporosis. Eur J Endocrinol England 142:170–173
Farr OM, Gavrieli A, Mantzoros CS (2015) Leptin applications in 2015: what have we learned about leptin and obesity? Curr Opin Endocrinol Diabetes Obes England 22:353–359
Fujita Y, Watanabe K, Maki K (2012) Serum leptin levels negatively correlate with trabecular bone mineral density in high-fat diet-induced obesity mice. J Musculoskelet Neuronal Interact Greece 12:84–94
Ionova-Martin SS, Do SH, Barth HD et al (2010) Reduced size-independent mechanical properties of cortical bone in high-fat diet-induced obesity. Bone United States 46:217–225
Patsch JM, Kiefer FW, Varga P et al (2011) Increased bone resorption and impaired bone microarchitecture in short-term and extended high-fat diet-induced obesity. Metabolism United States 60:243–249
Halade GV, El Jamali A, Williams PJ, Fajardo RJ, Fernandes G (2011) Obesity-mediated inflammatory microenvironment stimulates osteoclastogenesis and bone loss in mice. Exp Gerontol England 46:43–52
Ootsuka T, Nakanishi A, Tsukamoto I (2015) Increase in osteoclastogenesis in an obese Otsuka long-Evans Tokushima fatty rat model. Mol Med Rep Greece 12:3874–3880
Peric Kacarevic Z, Snajder D, Maric A et al (2016) High-fat diet induced changes in lumbar vertebra of the male rat offsprings. Acta Histochem Germany 118:711–721
Zhang K, Wang C, Chen Y et al (2015) Preservation of high-fat diet-induced femoral trabecular bone loss through genetic target of TNF-alpha. Endocrine United States 50:239–249
Feng W, Liu B, Liu D et al (2016) Long-term Administration of High-fat Diet Corrects Abnormal Bone Remodeling in the tibiae of Interleukin-6-deficient mice. J Histochem Cytochem United States 64:42–53
Laffel L (1999) Ketone bodies: a review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab Res Rev England 15:412–426
Yamasaki M, Hasegawa S, Imai M, Takahashi N, Fukui T (2016) High-fat diet-induced obesity stimulates ketone body utilization in osteoclasts of the mouse bone. Biochem Biophys Res Commun United States 473:654–661
Tomlinson JW, Bujalska I, Stewart PM, Cooper MS (2000) The role of 11 beta-hydroxysteroid dehydrogenase in central obesity and osteoporosis. Endocr Res England 26:711–722
Cooper MS, Walker EA, Bland R, Fraser WD, Hewison M, Stewart PM (2000) Expression and functional consequences of 11beta-hydroxysteroid dehydrogenase activity in human bone. Bone United States 27:375–381
Cooper MS, Bujalska I, Rabbitt E et al (2001) Modulation of 11beta-hydroxysteroid dehydrogenase isozymes by proinflammatory cytokines in osteoblasts: an autocrine switch from glucocorticoid inactivation to activation. J Bone Miner Res United States 16:1037–1044
Rajakumar K, Fernstrom JD, Holick MF, Janosky JE, Greenspan SL (2008) Vitamin D status and response to vitamin D(3) in obese vs. non-obese African American children. Obesity (Silver Spring) United States 16:90–95
Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF (2000) Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr United States 72:690–693
Grace C, Vincent R, Aylwin SJ (2014) High prevalence of vitamin D insufficiency in a United Kingdom urban morbidly obese population: implications for testing and treatment. Surg Obes Relat Dis United States 10:355–360
Hill KM, Braun MM, Egan KA et al (2011) Obesity augments calcium-induced increases in skeletal calcium retention in adolescents. J Clin Endocrinol Metab United States 96:2171–2177
Chaplin A, Palou A, Serra F (2015) Body fat loss induced by calcium in co-supplementation with conjugated linoleic acid is associated with increased expression of bone formation genes in adult mice. J Nutr Biochem United States 26:1540–1546
Parra P, Bruni G, Palou A, Serra F (2008) Dietary calcium attenuation of body fat gain during high-fat feeding in mice. J Nutr Biochem 19:109–117
Parra P, Palou A, Serra F (2010) Moderate doses of conjugated linoleic acid reduce fat gain, maintain insulin sensitivity without impairing inflammatory adipose tissue status in mice fed a high-fat diet. Nutr {&} Metab 7:5
Lee NK, Sowa H, Hinoi E et al (2007) Endocrine regulation of energy metabolism by the skeleton. Cell United States 130:456–469
Mosialou I, Shikhel S, Liu J-M et al (2017) MC4R-dependent suppression of appetite by bone-derived lipocalin 2. Nature England 543:385–390
Knapp KM, Welsman JR, Hopkins SJ, Fogelman I, Blake GM (2012) Obesity increases precision errors in dual-energy X-ray absorptiometry measurements. J Clin Densitom United States 15:315–319
Evans AL, Paggiosi MA, Eastell R, Walsh JS (2015) Bone density, microstructure and strength in obese and normal weight men and women in younger and older adulthood. J Bone Miner Res United States 30:920–928
Madeira E, Mafort TT, Madeira M et al (2014) Lean mass as a predictor of bone density and microarchitecture in adult obese individuals with metabolic syndrome. Bone United States 59:89–92
Edwards MH, Ward KA, Ntani G et al (2015) Lean mass and fat mass have differing associations with bone microarchitecture assessed by high resolution peripheral quantitative computed tomography in men and women from the Hertfordshire cohort study. Bone United States 81:145–151
Petit MA, Beck TJ, Shults J, Zemel BS, Foster BJ, Leonard MB (2005) Proximal femur bone geometry is appropriately adapted to lean mass in overweight children and adolescents. Bone United States 36:568–576
Kim W, Chung SG, Kim K et al (2014) The relationship between body fat and bone mineral density in Korean men and women. J Bone Miner Metab Japan 32:709–717
Mosca LN, Goldberg TBL, da Silva VN et al (2014) Excess body fat negatively affects bone mass in adolescents. Nutrition United States 30:847–852
Sornay-Rendu E, Boutroy S, Vilayphiou N, Claustrat B, Chapurlat RD (2013) In obese postmenopausal women, bone microarchitecture and strength are not commensurate to greater body weight: the Os des femmes de Lyon (OFELY) study. J Bone Miner Res 28:1679–1687
Liu C-T, Broe KE, Zhou Y et al (2017) Visceral adipose tissue is associated with bone microarchitecture in the Framingham osteoporosis study. J Bone Miner Res United States 32:143–150
Zhang P, Peterson M, Su GL, Wang SC (2015) Visceral adiposity is negatively associated with bone density and muscle attenuation. Am J Clin Nutr United States 101:337–343
Silva BC, Leslie WD, Resch H et al (2014) Trabecular bone score: a noninvasive analytical method based upon the DXA image. J Bone Miner Res 29:518–530
Amnuaywattakorn S, Sritara C, Utamakul C et al (2016) Simulated increased soft tissue thickness artefactually decreases trabecular bone score: a phantom study. BMC Musculoskelet Disord BioMed Central 17:17
Looker AC, Sarafrazi Isfahani N, Fan B, Shepherd JA (2016) Trabecular bone scores and lumbar spine bone mineral density of US adults: comparison of relationships with demographic and body size variables. Osteoporos Int 27:2467–2475
Kim JH, Choi HJ, Ku EJ et al (2016) Regional body fat depots differently affect bone microarchitecture in postmenopausal Korean women. Osteoporos Int 27:1161–1168
Langsetmo L, Vo TN, Ensrud KE et al (2016) The association between trabecular bone score and lumbar spine volumetric BMD is attenuated among older men with high body mass index. J Bone Miner Res 31:1820–1826
Pollock NK, Laing EM, Hamrick MW, Baile CA, Hall DB, Lewis RD (2011) Bone and fat relationships in postadolescent black females: a pQCT study. Osteoporos Int 22:655–665
Glass NA, Torner JC, Letuchy EM et al (2017) Do visceral or subcutaneous fat influence peripheral cortical bone strength during adolescence? A longitudinal study. J Bone Miner Res. https://doi.org/10.1002/jbmr.3325.
Viljakainen HT, Valta H, Lipsanen-Nyman M et al (2015) Bone characteristics and their determinants in adolescents and young adults with early-onset severe obesity. Calcif Tissue Int 97:364–375
Farr JN, Funk JL, Chen Z et al (2011) Skeletal muscle fat content is inversely associated with bone strength in young girls. J Bone Miner Res 26:2217–2225
Viljakainen H, Ivaska KK, Paldanius P et al (2014) Suppressed bone turnover in obesity: a link to energy metabolism? A case-control study. J Clin Endocrinol Metab United States 99:2155–2163
Compston JE, Vedi S, Ledger JE, Webb A, Gazet JC, Pilkington TR (1981) Vitamin D status and bone histomorphometry in gross obesity. Am J Clin Nutr United States 34:2359–2363
Lecka-Czernik B, Stechschulte LA, Czernik PJ, Dowling AR (2015) High bone mass in adult mice with diet-induced obesity results from a combination of initial increase in bone mass followed by attenuation in bone formation; implications for high bone mass and decreased bone quality in obesity. Mol Cell Endocrinol Ireland 410:35–41
Wong SK, Chin K-Y, Suhaimi FH, Ahmad F, Ima-Nirwana S (2018) Effects of metabolic syndrome on bone mineral density, histomorphometry and remodelling markers in male rats. PLoS One United States 13:e0192416
Johansson H, Kanis JA, Oden A et al (2014) A meta-analysis of the association of fracture risk and body mass index in women. J Bone Miner Res United States 29:223–233
Premaor MO, Compston JE, Fina Aviles F et al (2013) The association between fracture site and obesity in men: a population-based cohort study. J Bone Miner Res United States 28:1771–1777
Ishii S, Cauley JA, Greendale GA et al (2014) Pleiotropic effects of obesity on fracture risk: the study of Women’s health across the nation. J Bone Miner Res United States 29:2561–2570
Bachmann KN, Bruno AG, Bredella MA et al (2016) Vertebral strength and estimated fracture risk across the BMI Spectrum in women. J Bone Miner Res United States 31:281–288
Li X, Gong X, Jiang W (2017) Abdominal obesity and risk of hip fracture: a meta-analysis of prospective studies. Osteoporos Int England 28:2747–2757
Sadeghi O, Saneei P, Nasiri M, Larijani B, Esmaillzadeh A (2017) Abdominal obesity and risk of hip fracture: a systematic review and meta-analysis of prospective studies. Adv Nutr United States 8:728–738
Shen C-L, Zhu W, Gao W, Wang S, Chen L, Chyu M-C (2013) Energy-restricted diet benefits body composition but degrades bone integrity in middle-aged obese female rats. Nutr Res United States 33:668–676
Pluskiewicz W, Buzga M, Holeczy P, Bortlik L, Smajstrla V, Adamczyk P (2012) Bone mineral changes in spine and proximal femur in individual obese women after laparoscopic sleeve gastrectomy: a short-term study. Obes Surg United States 22:1068–1076
Noakes M, Keogh JB, Foster PR, Clifton PM (2005) Effect of an energy-restricted, high-protein, low-fat diet relative to a conventional high-carbohydrate, low-fat diet on weight loss, body composition, nutritional status, and markers of cardiovascular health in obese women. Am J Clin Nutr United States 81:1298–1306
Riedt CS, Buckley BT, Brolin RE, Ambia-Sobhan H, Rhoads GG, Shapses SA (2009) Blood lead levels and bone turnover with weight reduction in women. J Expo Sci Environ Epidemiol United States 19:90–96
Bacon L, Stern JS, Keim NL, Van Loan MD (2004) Low bone mass in premenopausal chronic dieting obese women. Eur J Clin Nutr England 58:966–971
Cifuentes M, Riedt CS, Brolin RE, Field MP, Sherrell RM, Shapses SA (2004) Weight loss and calcium intake influence calcium absorption in overweight postmenopausal women. Am J Clin Nutr United States 80:123–130
Uusi-Rasi K, Sievanen H, Kannus P, Pasanen M, Kukkonen-Harjula K, Fogelholm M (2009) Influence of weight reduction on muscle performance and bone mass, structure and metabolism in obese premenopausal women. J Musculoskelet Neuronal Interact Greece 9:72–80
Uusi-Rasi K, Rauhio A, Kannus P et al (2010) Three-month weight reduction does not compromise bone strength in obese premenopausal women. Bone United States 46:1286–1293
Christensen P, Frederiksen R, Bliddal H et al (2013) Comparison of three weight maintenance programs on cardiovascular risk, bone and vitamins in sedentary older adults. Obesity (Silver Spring) United States 21:1982–1990
Bowen J, Noakes M, Clifton PM (2004) A high dairy protein, high-calcium diet minimizes bone turnover in overweight adults during weight loss. J Nutr United States 134:568–573
Riedt CS, Schlussel Y, von Thun N et al (2007) Premenopausal overweight women do not lose bone during moderate weight loss with adequate or higher calcium intake. Am J Clin Nutr United States 85:972–980
Gerbaix M, Metz L, Mac-Way F et al (2013) A well-balanced diet combined or not with exercise induces fat mass loss without any decrease of bone mass despite bone micro-architecture alterations in obese rat. Bone United States 53:382–390
Ma H, Torvinen S, Silvennoinen M et al (2010) Effects of diet-induced obesity and voluntary wheel running on bone properties in young male C57BL/6J mice. Calcif Tissue Int United States 86:411–419
Ip TY, Peterson J, Byrner R, Tou JC (2009) Bone responses to body weight and moderate treadmill exercising in growing male obese (fa/fa) and lean Zucker rats. J Musculoskelet Neuronal Interact Greece 9:155–166
Villareal DT, Shah K, Banks MR, Sinacore DR, Klein S (2008) Effect of weight loss and exercise therapy on bone metabolism and mass in obese older adults: a one-year randomized controlled trial. J Clin Endocrinol Metab United States 93:2181–2187
Hinton PS, Rector RS, Linden MA et al (2012) Weight-loss-associated changes in bone mineral density and bone turnover after partial weight regain with or without aerobic exercise in obese women. Eur J Clin Nutr England 66:606–612
Shah K, Armamento-Villareal R, Parimi N et al (2011) Exercise training in obese older adults prevents increase in bone turnover and attenuates decrease in hip bone mineral density induced by weight loss despite decline in bone-active hormones. J Bone Miner Res United States 26:2851–2859
Pace DG, Blotner S, Guerciolini R (2001) Short-term orlistat treatment does not affect mineral balance and bone turnover in obese men. J Nutr United States 131:1694–1699
Gotfredsen A, Westergren Hendel H, Andersen T (2001) Influence of orlistat on bone turnover and body composition. Int J Obes Relat Metab Disord England 25:1154–1160
Sun H, Lu N, Luo X, Zhao L, Liu J (2015) Liraglutide, the glucagon-like peptide-1 receptor agonist, has anabolic bone effects in diabetic Goto-Kakizaki rats. J Diabetes Australia 7(4):584–588
Lu N, Sun H, Yu J et al (2015) Glucagon-like peptide-1 receptor agonist Liraglutide has anabolic bone effects in ovariectomized rats without diabetes. PLoS One United States e0132744:10
Iepsen EW, Lundgren JR, Hartmann B et al (2015) GLP-1 receptor agonist treatment increases bone formation and prevents bone loss in weight-reduced obese women. J. Clin. Endocrinol. Metab. In: United States
Su B, Sheng H, Zhang M et al (2015) Risk of bone fractures associated with glucagon-like peptide-1 receptor agonists’ treatment: a meta-analysis of randomized controlled trials. Endocrine United States 48:107–115
Mabilleau G, Mieczkowska A, Chappard D (2014) Use of glucagon-like peptide-1 receptor agonists and bone fractures: a meta-analysis of randomized clinical trials. J Diabetes Australia 6:260–266
Shin JH, Gadde KM (2013) Clinical utility of phentermine/topiramate (Qsymia) combination for the treatment of obesity. Diabetes Metab Syndr Obes New Zealand 6:131–139
Martin CK, Redman LM, Zhang J et al (2011) Lorcaserin, a 5-HT(2C) receptor agonist, reduces body weight by decreasing energy intake without influencing energy expenditure. J Clin Endocrinol Metab United States 96:837–845
Douglas IJ, Bhaskaran K, Batterham RL, Smeeth L (2015) Bariatric surgery in the United Kingdom: a cohort study of weight loss and clinical outcomes in routine clinical care. Neal B, editor. PLoS med San Francisco, CA USA. Public Libr Sci 12:e1001925
Maciejewski ML, Arterburn DE, Van Scoyoc L et al (2016) Bariatric surgery and long-term durability of weight loss. JAMA Surg United States 151:1046–1055
Coates PS, Fernstrom JD, Fernstrom MH, Schauer PR, Greenspan SL (2004) Gastric bypass surgery for morbid obesity leads to an increase in bone turnover and a decrease in bone mass. J Clin Endocrinol Metab United States 89:1061–1065
Bruno C, Fulford AD, Potts JR et al (2010) Serum markers of bone turnover are increased at six and 18 months after roux-En-Y bariatric surgery: correlation with the reduction in leptin. J Clin Endocrinol Metab The Endocrine Society 95:159–166
Casagrande DS, Repetto G, Mottin CC et al (2012) Changes in bone mineral density in women following 1-year gastric bypass surgery. Obes Surg United States 22:1287–1292
Yu EW, Wewalka M, Ding S-A et al (2016) Effects of gastric bypass and gastric banding on bone remodeling in obese patients with type 2 diabetes. J Clin Endocrinol Metab United States 101:714–722
Schollenberger AE, Heinze JM, Meile T, Peter A, Konigsrainer A, Bischoff SC (2015) Markers of bone metabolism in obese individuals undergoing laparoscopic sleeve gastrectomy. Obes Surg United States 25:1439–1445
Tsiftsis DDA, Mylonas P, Mead N, Kalfarentzos F, Alexandrides TK (2009) Bone mass decreases in morbidly obese women after long limb-biliopancreatic diversion and marked weight loss without secondary hyperparathyroidism. A physiological adaptation to weight loss? Obes Surg United States 19:1497–1503
Balsa JA, Botella-Carretero JI, Peromingo R et al (2010) Chronic increase of bone turnover markers after biliopancreatic diversion is related to secondary hyperparathyroidism and weight loss. Relation with bone mineral density. Obes Surg United States 20:468–473
Guney E, Kisakol G, Ozgen G, Yilmaz C, Yilmaz R, Kabalak T (2003) Effect of weight loss on bone metabolism: comparison of vertical banded gastroplasty and medical intervention. Obes Surg United States 13:383–388
Mahdy T, Atia S, Farid M, Adulatif A (2008) Effect of roux-en Y gastric bypass on bone metabolism in patients with morbid obesity: Mansoura experiences. Obes Surg United States 18:1526–1531
Vilarrasa N, Gomez JM, Elio I et al (2009) Evaluation of bone disease in morbidly obese women after gastric bypass and risk factors implicated in bone loss. Obes Surg United States 19:860–866
Vilarrasa N, de Gordejuela AGR, Gomez-Vaquero C et al (2013) Effect of bariatric surgery on bone mineral density: comparison of gastric bypass and sleeve gastrectomy. Obes Surg United States 23:2086–2091
Ruiz-Tovar J, Oller I, Priego P et al (2013) Short- and mid-term changes in bone mineral density after laparoscopic sleeve gastrectomy. Obes Surg United States 23:861–866
Ko B-J, Myung SK, Cho K-H et al (2016) Relationship between bariatric surgery and bone mineral density: a meta-analysis. Obes Surg United States 26:1414–1421
Yu EW, Bouxsein ML, Roy AE et al (2014) Bone loss after bariatric surgery: discordant results between DXA and QCT bone density. J Bone Miner Res United States 29:542–550
Stein EM, Carrelli A, Young P et al (2013) Bariatric surgery results in cortical bone loss. J Clin Endocrinol Metab United States 98:541–549
Frederiksen KD, Hanson S, Hansen S et al (2016) Bone structural changes and estimated strength after gastric bypass surgery evaluated by HR-pQCT. Calcif Tissue Int United States 98:253–262
Shanbhogue VV, Stoving RK, Frederiksen KH et al (2017) Bone structural changes after gastric bypass surgery evaluated by HR-pQCT: a two-year longitudinal study. Eur J Endocrinol England 176:685–693
Scibora LM, Buchwald H, Petit MA, Hughes J, Ikramuddin S (2015) Bone strength is preserved following bariatric surgery. Obes Surg United States 25:263–270
Lu C-W, Chang Y-K, Chang H-H et al (2015) Fracture risk after bariatric surgery: a 12-year Nationwide cohort study. Medicine (Baltimore) United States e2087:94
Nakamura KM, Haglind EGC, Clowes JA et al (2014) Fracture risk following bariatric surgery: a population-based study. Osteoporos Int England 25:151–158
Rousseau C, Jean S, Gamache P et al (2016) Change in fracture risk and fracture pattern after bariatric surgery: nested case-control study. BMJ England i3794:354
Lalmohamed A, de Vries F, Bazelier MT et al (2012) Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ England e5085:345
Yu EW, Lee MP, Landon JE, Lindeman KG, Kim SC (2017) Fracture risk after bariatric surgery: roux-en-Y gastric bypass versus adjustable gastric banding. J Bone Miner Res United States 32:1229–1236
Krolner B, Ranlov PJ, Clemmesen T, Nielsen SP (1982) Bone loss after gastroplasty for morbid obesity: side-effect or adaptive response to weight reduction? Lancet 1(8278):956–957
de Vasconcelos RS, Viegas M, Marques TF et al (2010) Factors associated with secondary hyperparathyroidism in premenopausal women undergoing roux-en-Y gastric bypass for the treatment of obesity. Arq Bras Endocrinol Metabol Brazil 54:233–238
Riedt CS, Brolin RE, Sherrell RM, Field MP, Shapses SA (2006) True fractional calcium absorption is decreased after roux-en-Y gastric bypass surgery. Obesity (Silver Spring) United States 14:1940–1948
Hey H, Lund B, Sorensen OH, Lund B, Christensen MS (1979) Impairment of vitamin D and bone metabolism in patients with bypass operation for obesity. Acta Med Scand Suppl Sweden 624:73–78
Rickers H, Christiansen C, Balslev I, Foltved H, Rodbro P, Christensen MS (1983) Vitamin D and bone mineral content after intestinal bypass operation for obesity. Gut England 24:67–72
Balsa JA, Lafuente C, Gomez-Martin JM et al (2016) The role of serum osteoprotegerin and receptor-activator of nuclear factor-kappaB ligand in metabolic bone disease of women after obesity surgery. J Bone Miner Metab Japan 34:655–661
Muschitz C, Kocijan R, Marterer C et al (2015) Sclerostin levels and changes in bone metabolism after bariatric surgery. J Clin Endocrinol Metab United States 100:891–901
Muschitz C, Kocijan R, Haschka J et al (2016) The impact of vitamin D, calcium, protein supplementation, and physical exercise on bone metabolism after bariatric surgery: the BABS study. J Bone Miner Res United States 31:672–682
Campanha-Versiani L, Pereira DAG, Ribeiro-Samora GA et al (2017) The effect of a muscle weight-bearing and aerobic exercise program on the body composition, muscular strength, biochemical markers, and bone mass of obese patients who have undergone gastric bypass surgery. Obes Surg United States 27:2129–2137
Mechanick J, Youdim A, Jones D et al (2013) Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American society fo. Endocr Pract American Association of Clinical Endocrinologists 19:337–372
Acknowledgments
The authors would like to thank Dimitri Koutsomitis for his kind support with the illustrations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they do not have conflict of interest.