Abstract
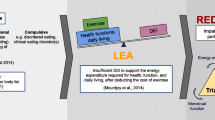
In a high-performance sports environment, athletes can present with low energy availability (LEA) for a variety of reasons, ranging from not consuming enough food for their specific energy requirements to disordered eating behaviors. Both male and female high-performance athletes are at risk of LEA. Longstanding LEA can cause unfavorable physiological and psychological outcomes which have the potential to impair an athlete’s health and sports performance. This narrative review summarizes the prevalence of LEA and its associations with athlete health and sports performance. It is evident in the published scientific literature that the methods used to determine LEA and its associated health outcomes vary. This contributes to poor recognition of the condition and its sequelae. This review also identifies interventions designed to improve health outcomes in athletes with LEA and indicates areas which warrant further investigation. While return-to-play guidelines have been developed for healthcare professionals to manage LEA in athletes, behavioral interventions to prevent the condition and manage its associated negative health and performance outcomes are required.


Similar content being viewed by others
References
Loucks AB, Kiens B, Wright HH. Energy availability in athletes. J Sports Sci. 2011;29(Suppl 1):S7–15.
Melin A, Tornberg AB, Skouby S, et al. Energy availability and the female athlete triad in elite endurance athletes. Scand J Med Sci Sports. 2015;25(5):610–22.
Nattiv A, Loucks AB, Manore MM, et al. American College of Sports Medicine position stand. The female athlete triad. Med Sci Sports Exerc. 2007;39(10):1867–82.
De Souza MJ, Nattiv A, Joy E, et al. 2014 Female Athlete Triad Coalition consensus statement on treatment and return to play of the female athlete triad: 1st International Conference held in San Francisco, CA, May 2012, and 2nd International Conference held in Indianapolis, IN, May 2013. Clin J Sport Med. 2014;24(2):96–119.
Otis CL, Drinkwater B, Johnson M, et al. American College of Sports Medicine position stand. The Female Athlete Triad. Med Sci Sports Exerc. 1997;29(5):i–ix.
Mountjoy M, Sundgot-Borgen J, Burke L, et al. The IOC consensus statement: beyond the Female Athlete Triad-Relative Energy Deficiency in Sport (RED-S). Br J Sports Med. 2014;48(7):491–7.
Tenforde AS, Barrack MT, Nattiv A, et al. Parallels with the female athlete triad in male athletes. Sports Med. 2016;46(2):171–82.
Slater J, Brown R, McLay-Cooke R, et al. Low energy availability in exercising women: historical perspectives and future directions. Sports Med. 2017;47(2):207–20.
Mountjoy M, Sundgot-Borgen J, Burke L, et al. Authors’ 2015 additions to the IOC consensus statement: Relative Energy Deficiency in Sport (RED-S). Br J Sports Med. 2015;49(7):417–20.
Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323(7308):334–6.
Loucks AB, Verdun M, Heath EM. Low energy availability, not stress of exercise, alters LH pulsatility in exercising women. J Appl Physiol. 1998;84(1):37–46.
Loucks AB, Thuma JR. Luteinizing hormone pulsatility is disrupted at a threshold of energy availability in regularly menstruating women. J Clin Endocrinol Metab. 2003;88(1):297–311.
Loucks AB. Physical health of the female athlete: observations, effects, and causes of reproductive disorders. Can J Appl Physiol. 2001;26(Suppl):S176–85.
Ihle R, Loucks AB. Dose-response relationships between energy availability and bone turnover in young exercising women. J Bone Miner Res. 2004;19(8):1231–40.
Bullen BA, Skrinar GS, Beitins IZ, et al. Induction of menstrual disorders by strenuous exercise in untrained women. N Engl J Med. 1985;312(21):1349–53.
Williams NI, Helmreich DL, Parfitt DB, et al. Evidence for a causal role of low energy availability in the induction of menstrual cycle disturbances during strenuous exercise training. J Clin Endocrinol Metab. 2001;86(11):5184–93.
Williams NI, Leidy HJ, Hill BR, et al. Magnitude of daily energy deficit predicts frequency but not severity of menstrual disturbances associated with exercise and caloric restriction. Am J Physiol Endocrinol Metab. 2015;308(1):E29–39.
Reed JL, De Souza MJ, Williams NI. Changes in energy availability across the season in Division I female soccer players. J Sports Sci. 2013;31(3):314–24.
Viner RT, Harris M, Berning JR, et al. Energy availability and dietary patterns of adult male and female competitive cyclists with lower than expected bone mineral density. Int J Sport Nutr Exerc Metab. 2015;25(6):594–602.
Koehler K, Achtzehn S, Braun H, et al. Comparison of self-reported energy availability and metabolic hormones to assess adequacy of dietary energy intake in young elite athletes. Appl Physiol Nutr Metab. 2013;38(7):725–33.
Gibbs JC, Williams NI, De Souza MJ. Prevalence of individual and combined components of the female athlete triad. Med Sci Sports Exerc. 2013;45(5):985–96.
Woodruff SJ, Meloche RD. Energy availability of female varsity volleyball players. Int J Sport Nutr Exerc Metab. 2013;23(1):24–30.
Vanheest JL, Rodgers CD, Mahoney CE, et al. Ovarian suppression impairs sport performance in junior elite female swimmers. Med Sci Sports Exerc. 2014;46(1):156–66.
Muia EN, Wright HH, Onywera VO, et al. Adolescent elite Kenyan runners are at risk for energy deficiency, menstrual dysfunction and disordered eating. J Sports Sci. 2016;34(7):598–606.
Silva MR, Paiva T. Low energy availability and low body fat of female gymnasts before an international competition. Eur J Sport Sci. 2015;15(7):591–9.
Dolan E, O’Connor H, McGoldrick A, et al. Nutritional, lifestyle, and weight control practices of professional jockeys. J Sports Sci. 2011;29(8):791–9.
Doyle-Lucas AF, Akers JD, Davy BM. Energetic efficiency, menstrual irregularity, and bone mineral density in elite professional female ballet dancers. J Dance Med Sci. 2010;14(4):146–54.
Hoch AZ, Pajewski NM, Moraski L, et al. Prevalence of the female athlete triad in high school athletes and sedentary students. Clin J Sport Med. 2009;19(5):421–8.
Thong FS, McLean C, Graham TE. Plasma leptin in female athletes: relationship with body fat, reproductive, nutritional, and endocrine factors. J Appl Physiol. 2000;88(6):2037–44.
De Souza MJ, Miller BE, Loucks AB, et al. High frequency of luteal phase deficiency and anovulation in recreational women runners: blunted elevation in follicle-stimulating hormone observed during luteal-follicular transition. J Clin Endocrinol Metab. 1998;83(12):4220–32.
Magkos F, Yannakoulia M. Methodology of dietary assessment in athletes: concepts and pitfalls. Curr Opin Clin Nutr Metab Care. 2003;6(5):539–49.
Reed JL, De Souza MJ, Kindler JM, et al. Nutritional practices associated with low energy availability in Division I female soccer players. J Sports Sci. 2014;32(16):1499–509.
Burke L, Deakin V. Clinical sports nutrition. North Ryde: McGraw-Hill Education; 2015.
Schaal K, Tiollier E, Le Meur Y, et al. Elite synchronized swimmers display decreased energy availability during intensified training. Scand J Med Sci Sports. 2016;1(27):925–34.
Koehler K, Hoerner NR, Gibbs JC, et al. Low energy availability in exercising men is associated with reduced leptin and insulin but not with changes in other metabolic hormones. J Sports Sci. 2016;34(20):1921–9.
Hagmar M, Berglund B, Brismar K, et al. Body composition and endocrine profile of male Olympic athletes striving for leanness. Clin J Sport Med. 2013;23(3):197–201.
Melin A, Tornberg AB, Skouby S, et al. The LEAF questionnaire: a screening tool for the identification of female athletes at risk for the female athlete triad. Br J Sports Med. 2014;48(7):540–5.
McNulty KY, Adams CH, Anderson JM, et al. Development and validation of a screening tool to identify eating disorders in female athletes. J Am Diet Assoc. 2001;101(8):886–92 (quiz 93–4).
Folscher LL, Grant CC, Fletcher L, et al. Ultra-marathon athletes at risk for the female athlete triad. Sports Med Open. 2015;1(1):29.
De Souza MJ, Hontscharuk R, Olmsted M, et al. Drive for thinness score is a proxy indicator of energy deficiency in exercising women. Appetite. 2007;48(3):359–67.
Byrne S, McLean N. Elite athletes: effects of the pressure to be thin. J Sci Med Sport. 2002;5(2):80–94.
Sundgot-Borgen J, Torstveit MK. Prevalence of eating disorders in elite athletes is higher than in the general population. Clin J Sport Med. 2004;14(1):25–32.
Sundgot-Borgen J, Torstveit MK. Aspects of disordered eating continuum in elite high-intensity sports. Scand J Med Sci Sport. 2010;20(2):112–21.
Goltz FR, Stenzel LM, Schneider CD. Disordered eating behaviors and body image in male athletes. Rev Bras Psiquiatr. 2013;35(3):237–42.
Torstveit MK, Rosenvinge JH, Sundgot-Borgen J. Prevalence of eating disorders and the predictive power of risk models in female elite athletes: a controlled study. Scand J Med Sci Sports. 2008;18(1):108–18.
Gibbs JC, Williams NI, Mallinson RJ, et al. Effect of high dietary restraint on energy availability and menstrual status. Med Sci Sports Exerc. 2013;45(9):1790–7.
Schaal K, Van Loan MD, Casazza GA. Reduced catecholamine response to exercise in amenorrheic athletes. Med Sci Sports Exerc. 2011;43(1):34–43.
Martinsen M, Holme I, Pensgaard AM, et al. The development of the brief eating disorder in athletes questionnaire. Med Sci Sports Exerc. 2014;46(8):1666–75.
Warren MP. Endocrine manifestations of eating disorders. J Clin Endocrinol Metab. 2011;96(2):333–43.
Hilton LK, Loucks AB. Low energy availability, not exercise stress, suppresses the diurnal rhythm of leptin in healthy young women. Am J Physiol Endocrinol Metab. 2000;278(1):E43–9.
Scheid JL, De Souza MJ, Leidy HJ, et al. Ghrelin but not peptide YY is related to change in body weight and energy availability. Med Sci Sports Exerc. 2011;43(11):2063–71.
Hill BR, De Souza MJ, Wagstaff DA, et al. The impact of weight loss on the 24-h profile of circulating peptide YY and its association with 24-h ghrelin in normal weight premenopausal women. Peptides. 2013;49:81–90.
Leidy HJ, Gardner JK, Frye BR, et al. Circulating ghrelin is sensitive to changes in body weight during a diet and exercise program in normal-weight young women. J Clin Endocrinol Metab. 2004;89(6):2659–64.
Leidy HJ, Dougherty KA, Frye BR, et al. Twenty-four-hour ghrelin is elevated after calorie restriction and exercise training in non-obese women. Obesity (Silver Spring). 2007;15(2):446–55.
Melin A, Tornberg AB, Skouby S, et al. Low-energy density and high fiber intake are dietary concerns in female endurance athletes. Scand J Med Sci Sports. 2016;26(9):1060–71.
Burke LM, Hawley JA, Wong SH, et al. Carbohydrates for training and competition. J Sports Sci. 2011;29(Suppl 1):S17–27.
Lagowska K, Kapczuk K. Testosterone concentrations in female athletes and ballet dancers with menstrual disorders. Eur J Sport Sci. 2016;16(4):490–7.
Poslusna K, Ruprich J, de Vries JH, et al. Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br J Nutr. 2009;101(Suppl 2):S73–85.
Dwyer J, Eisenberg A, Prelack K, et al. Eating attitudes and food intakes of elite adolescent female figure skaters: a cross sectional study. J Int Soc Sports Nutr. 2012;9(1):53.
Martin B, Golden E, Carlson OD, et al. Caloric restriction: impact upon pituitary function and reproduction. Ageing Res Rev. 2008;7(3):209–24.
Hoch AZ, Papanek P, Szabo A, et al. Association between the female athlete triad and endothelial dysfunction in dancers. Clin J Sport Med. 2011;21(2):119–25.
Lagowska K, Kapczuk K, Friebe Z, et al. Effects of dietary intervention in young female athletes with menstrual disorders. J Int Soc Sports Nutr. 2014;11:21.
Hackney AC. Effects of endurance exercise on the reproductive system of men: the “exercise-hypogonadal male condition”. J Endocrinol Investig. 2008;31(10):932–8.
Hagmar M, Berglund B, Brismar K, et al. Hyperandrogenism may explain reproductive dysfunction in olympic athletes. Med Sci Sports Exerc. 2009;41(6):1241–8.
Cashman KD. Diet, nutrition, and bone health. J Nutr. 2007;137(11 Suppl):2507s–12s.
Nana A, Slater GJ, Hopkins WG, et al. Importance of standardized DXA protocol for assessing physique changes in athletes. Int J Sport Nutr Exerc Metab. 2016;26(3):259–67.
Barrack MT, Rauh MJ, Barkai H-S, et al. Dietary restraint and low bone mass in female adolescent endurance runners. Am J Clin Nutr. 2008;87(1):36–43.
Barrack MT, Rauh MJ, Nichols JF. Prevalence of and traits associated with low BMD among female adolescent runners. Med Sci Sports Exerc. 2008;40(12):2015–21.
Tenforde AS, Fredericson M, Sayres LC, et al. Identifying sex-specific risk factors for low bone mineral density in adolescent runners. Am J Sports Med. 2015;43(6):1494–504.
Duckham RL, Peirce N, Meyer C, et al. Risk factors for stress fracture in female endurance athletes: a cross-sectional study. BMJ Open. 2012;2(6):e001920.
Mallinson RJ, Williams NI, Hill BR, et al. Body composition and reproductive function exert unique influences on indices of bone health in exercising women. Bone. 2013;56(1):91–100.
Vanderschueren D, Laurent MR, Claessens F, et al. Sex steroid actions in male bone. Endo Rev. 2014;35(6):906–60.
Moran JM, Martin RR, Pedrera-Canal M, et al. Low testosterone levels are associated with poor peripheral bone mineral density and quantitative bone ultrasound at phalanges and calcaneus in healthy elderly men. Biol Res Nurs. 2015;17(2):169–74.
Dolan E, McGoldrick A, Davenport C, et al. An altered hormonal profile and elevated rate of bone loss are associated with low bone mass in professional horse-racing jockeys. J Bone Miner Metab. 2012;30(5):534–42.
Pepper M, Akuthota V, McCarty EC. The pathophysiology of stress fractures. Clin Sports Med. 2006;25(1):1–16, vii.
Rauh MJ, Nichols JF, Barrack MT. Relationships among injury and disordered eating, menstrual dysfunction, and low bone mineral density in high school athletes: a prospective study. J Athl Train. 2010;45(3):243–52.
Thein-Nissenbaum JM, Rauh MJ, Carr KE, et al. Associations between disordered eating, menstrual dysfunction, and musculoskeletal injury among high school athletes. J Orthop Sports Phys Ther. 2011;41(2):60–9.
Thein-Nissenbaum JM, Rauh MJ, Carr KE, et al. Menstrual irregularity and musculoskeletal injury in female high school athletes. J Athl Train. 2012;47(1):74–82.
Tenforde AS, Sayres LC, McCurdy ML, et al. Overuse injuries in high school runners: lifetime prevalence and prevention strategies. PM R. 2011;3(2):125–31 (quiz 31).
Beals KA, Manore MM. Disorders of the female athlete triad among collegiate athletes. Int J Sport Nutr Exerc Metab. 2002;12(3):281–93.
Palmer-Green D, Fuller C, Jaques R, et al. The Injury/Illness Performance Project (IIPP): a novel epidemiological approach for recording the consequences of sports injuries and illnesses. J Sports Med (Hindawi Publ Corp). 2013;2013:523974.
Walsh NP, Gleeson M, Pyne DB, et al. Position statement. Part two: maintaining immune health. Exerc Immunol Rev. 2011;17:64–103.
Gleeson M, Pyne DB. Respiratory inflammation and infections in high-performance athletes. Immunol Cell Biol. 2016;94(2):124–31.
Gleeson M. Immunological aspects of sport nutrition. Immunol Cell Biol. 2016;94(2):117–23.
Raysmith BP, Drew MK. Performance success or failure is influenced by weeks lost to injury and illness in elite Australian track and field athletes: a 5-year prospective study. J Sci Med Sport. 2016;19(10):778–83.
Flierl MA, Rittirsch D, Huber-Lang M, et al. Catecholamines-crafty weapons in the inflammatory arsenal of immune/inflammatory cells or opening Pandora’s box? Mol Med. 2008;14(3–4):195–204.
Zouhal H, Jacob C, Delamarche P, et al. Catecholamines and the effects of exercise, training and gender. Sports Med. 2008;38(5):401–23.
Abedelmalek S, Chtourou H, Souissi N, et al. Caloric restriction effect on proinflammatory cytokines, growth hormone, and steroid hormone concentrations during exercise in judokas. Oxid Med Cell Longev. 2015;2015:809492.
Shimizu K, Aizawa K, Suzuki N, et al. Influences of weight loss on monocytes and T-cell subpopulations in male judo athletes. J Strength Cond Res. 2011;25(7):1943–50.
Imai T, Seki S, Dobashi H, et al. Effect of weight loss on T-cell receptor-mediated T-cell function in elite athletes. Med Sci Sports Exerc. 2002;34(2):245–50.
Kowatari K, Umeda T, Shimoyama T, et al. Exercise training and energy restriction decrease neutrophil phagocytic activity in judoists. Med Sci Sports Exerc. 2001;33(4):519–24.
Suzuki M, Nakaji S, Umeda T, et al. Effects of weight reduction on neutrophil phagocytic activity and oxidative burst activity in female judoists. Luminescence. 2003;18(4):214–7.
Yaegaki M, Umeda T, Takahashi I, et al. Change in the capability of reactive oxygen species production by neutrophils following weight reduction in female judoists. Br J Sports Med. 2007;41(5):322–7.
Tsai ML, Chou KM, Chang CK, et al. Changes of mucosal immunity and antioxidation activity in elite male Taiwanese taekwondo athletes associated with intensive training and rapid weight loss. Br J Sports Med. 2011;45(9):729–34.
Marcotte H, Lavoie MC. Oral microbial ecology and the role of salivary immunoglobulin A. Microbiol Mol Biol Rev. 1998;62(1):71–109.
Tsai ML, Ko MH, Chang CK, et al. Impact of intense training and rapid weight changes on salivary parameters in elite female Taekwondo athletes. Scand J Med Sci Sports. 2011;21(6):758–64.
Schachinger V, Britten MB, Zeiher AM. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation. 2000;101(16):1899–906.
Dusting GJ, Fennessy P, Yin ZL, et al. Nitric oxide in atherosclerosis: vascular protector or villain? Clin Exp Pharmacol Physiol Suppl. 1998;25:S34–41.
Zeni Hoch A, Dempsey RL, Carrera GF, et al. Is there an association between athletic amenorrhea and endothelial cell dysfunction? Med Sci Sports Exerc. 2003;35(3):377–83.
Rickenlund A, Eriksson MJ, Schenck-Gustafsson K, et al. Amenorrhea in female athletes is associated with endothelial dysfunction and unfavorable lipid profile. J Clin Endocrinol Metab. 2005;90(3):1354–9.
Misra M, Miller KK, Tsai P, et al. Uncoupling of cardiovascular risk markers in adolescent girls with anorexia nervosa. J Pediatr. 2006;149(6):763–9.
Ohwada R, Hotta M, Oikawa S, et al. Etiology of hypercholesterolemia in patients with anorexia nervosa. Int J Eat Disord. 2006;39(7):598–601.
Filaire E, Maso F, Degoutte F, et al. Food restriction, performance, psychological state and lipid values in judo athletes. Int J Sports Med. 2001;22(6):454–9.
Fogelholm M. Effects of bodyweight reduction on sports performance. Sports Med. 1994;18(4):249–67.
El Ghoch M, Soave F, Calugi S, et al. Eating disorders, physical fitness and sport performance: a systematic review. Nutrients. 2013;5(12):5140–60.
Lacey JM. Disordered eating among athletes: a comprehensive guide for health professionals. Middletown: American Library Association CHOICE; 2005. p. 2021.
Armstrong LE, VanHeest JL. The unknown mechanism of the overtraining syndrome: clues from depression and psychoneuroimmunology. Sports Med. 2002;32(3):185–209.
Mackinnon LT. Overtraining effects on immunity and performance in athletes. Immunol Cell Biol. 2000;78(5):502–9.
Garthe I, Raastad T, Refsnes PE, et al. Effect of nutritional intervention on body composition and performance in elite athletes. Eur J Sport Sci. 2013;13(3):295–303.
Cialdella-Kam L, Guebels CP, Maddalozzo GF, et al. Dietary intervention restored menses in female athletes with exercise-associated menstrual dysfunction with limited impact on bone and muscle health. Nutrients. 2014;6(8):3018–39.
Guebels CP, Kam LC, Maddalozzo GF, et al. Active women before/after an intervention designed to restore menstrual function: resting metabolic rate and comparison of four methods to quantify energy expenditure and energy availability. Int J Sport Nutr Exerc Metab. 2014;24(1):37–46.
Dueck CA, Matt KS, Manore MM, et al. Treatment of athletic amenorrhea with a diet and training intervention program. Int J Sport Nutr. 1996;6(1):24–40.
Molina-Lopez J, Molina JM, Chirosa LJ, et al. Implementation of a nutrition education program in a handball team; consequences on nutritional status. Nutr Hosp. 2013;28(4):1065–76.
Valliant MW, Emplaincourt HP, Wenzel RK, et al. Nutrition education by a registered dietitian improves dietary intake and nutrition knowledge of a NCAA female volleyball team. Nutrients. 2012;4(6):506–16.
Day J, Wengreen H, Heath E, et al. Prevalence of low energy availability in collegiate female runners and implementation of nutrition education intervention. Sports Nutr Ther. 2015;1:101.
Garthe I, Raastad T, Sundgot-Borgen J. Long-term effect of nutritional counselling on desired gain in body mass and lean body mass in elite athletes. Appl Physiol Nutr Metab. 2011;36(4):547–54.
Kopp-Woodroffe SA, Manore MM, Dueck CA, et al. Energy and nutrient status of amenorrheic athletes participating in a diet and exercise training intervention program. Int J Sport Nutr. 1999;9(1):70–88.
Slater J, McLay-Cooke R, Brown R, et al. Female recreational exercisers at risk for low energy availability. Int J Sport Nutr Exerc Metab. 2016;26(5):421–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research is funded by the Irish Research Council (IRC) and Sport Ireland (Grant number: EPS-PG-2015-99).
Conflict of interest
Danielle Logue, Sharon Madigan, Eamonn Delahunt, Mirjam Heinen, Sarah-Jane McDonnell, and Clare Corish declare that they have no conflicts of interest relevant to the content of this review.
Rights and permissions
About this article
Cite this article
Logue, D., Madigan, S.M., Delahunt, E. et al. Low Energy Availability in Athletes: A Review of Prevalence, Dietary Patterns, Physiological Health, and Sports Performance. Sports Med 48, 73–96 (2018). https://doi.org/10.1007/s40279-017-0790-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-017-0790-3