Abstract
Teriflunomide is a once-daily oral agent that has been licensed in the EU since August 2013 for the treatment of adult patients with relapsing–remitting multiple sclerosis (RRMS). More recently (September 2014), the EU summary of product characteristics (SmPC) was updated to include data from patients with a first clinical demyelinating event. This review examines the EU SmPC for teriflunomide, with reference to key clinical and safety outcomes and practical considerations for prescribing physicians. In two phase III trials (TEMSO and TOWER) in patients with relapsing forms of MS, teriflunomide 14 mg significantly reduced the annualized relapse rate and the risk of confirmed disability progression sustained for at least 12 weeks. Magnetic resonance imaging (MRI) total lesion volume, gadolinium-enhancing lesions, and unique active lesions were reduced with teriflunomide treatment in TEMSO. In the TOPIC study, in patients with a first clinical demyelinating event, teriflunomide treatment significantly reduced the time to a second clinical episode (relapse). Across the clinical studies, teriflunomide was generally well tolerated; adverse events reported in ≥10 % of teriflunomide-treated patients were diarrhea, nausea, increased alanine aminotransferase, and alopecia. Data from the clinical development program support the use of teriflunomide in a broad spectrum of patients with RRMS.
Similar content being viewed by others
Teriflunomide is a once-daily oral treatment approved for relapsing–remitting multiple sclerosis. |
Teriflunomide has pleiotropic and novel mechanisms of action, specifically targeting activated T and B cells. |
Teriflunomide demonstrated consistent efficacy in reducing the risk of disability progression and the annualized relapse rate in two independent phase III trials (TEMSO, TOWER) as well as positive outcomes on several magnetic resonance imaging (MRI) parameters of disease activity (TEMSO). |
1 Introduction
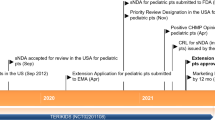
Teriflunomide (Aubagio®, sanofi-aventis groupe, Paris, France) is a once-daily oral agent that was approved in the EU in August 2013 for the treatment of adult patients with relapsing–remitting multiple sclerosis (RRMS) [1]. It was the second oral disease-modifying therapy (DMT), following fingolimod (Gilenya®, Novartis Europharm Ltd, UK), approved in the EU for the treatment of RRMS in March 2011 [2]. Fingolimod is approved for use in patients with high disease activity despite treatment with at least one DMT, or in patients with rapidly evolving severe RRMS. The 14-mg dose of teriflunomide is licensed in the EU and several other countries. BG-12 (Tecfidera®, Biogen Idec Ltd, UK) has also been approved for patients with RRMS [3].
Teriflunomide’s mechanism of action is considered to be related to its effect on rapidly dividing lymphocytes. Teriflunomide selectively and reversibly inhibits a key mitochondrial enzyme, dihydroorotate dehydrogenase (DHODH), required for de novo pyrimidine synthesis. As a consequence of limited de novo pyrimidine production, teriflunomide reduces the proliferation of activated T and B cells, which are thought to participate in the inflammatory process in the central nervous system [4]. In vitro, teriflunomide causes cell-cycle arrest without cell death [5, 6], and the cytostatic effects of teriflunomide can be reversed by the addition of exogenous uridine [6], which supports DHODH inhibition as the primary mechanism. However, pleiotropic effects independent from DHODH inhibition have also been reported [4]. Investigation of the effects of teriflunomide on peripheral blood mononuclear cells in vitro have shown little or no impact on lymphocyte activation and no cytotoxicity associated with teriflunomide [7]. Resting lymphocytes rely on the salvage pathway, which is unaffected by teriflunomide, to meet their pyrimidine needs, thereby preserving these cells for normal immune surveillance. In a study of teriflunomide’s effect on the immune response to seasonal influenza vaccine, patients with relapsing forms of MS (RMS) receiving teriflunomide generally mounted appropriate memory immune responses to influenza vaccination [8]. In a separate study, teriflunomide-treated healthy volunteers were able to make a seroprotective response to neoantigen (rabies vaccine) [9]. Together, these results argue against a clinically relevant immunosuppressive effect.
Teriflunomide is the active metabolite of leflunomide (ARAVA®, Sanofi-Aventis Deutschland GmbH, Germany), a disease-modifying antirheumatic drug (DMARD) licensed in the EU since 1999 for the treatment of adult patients with active rheumatoid arthritis (RA) [10]. Post-marketing experience with leflunomide has informed the EU summary of product characteristics (SmPC) for teriflunomide, specifically regarding safety as reflected in warnings and precautions for use. However, there are a number of challenges when comparing the safety of teriflunomide with its parent compound; leflunomide has only been evaluated in patients with RA, who often have comorbidities and are prescribed concomitant medications, which may impact the safety observations on leflunomide and confound comparisons with teriflunomide. There are also pharmacological differences between leflunomide and teriflunomide, which are discussed below.
This review summarizes key efficacy and safety data that supported the approval of teriflunomide 14 mg for the once-daily treatment of RRMS. It specifically focuses on recommendations in the EU SmPC in the context of clinical practice, with the aim of providing a practical reference for treatment.
2 Key Data from Teriflunomide Trials
2.1 Efficacy Outcomes
The efficacy of teriflunomide was demonstrated in three phase III, placebo-controlled trials, TEMSO (NCT00134563) [1, 11], TOWER (NCT00751881) [1, 12], and TOPIC (NCT00622700) [1, 13] (Table 1), and in one active comparator phase III trial, TENERE (NCT00883337) [1, 14]. Data pertaining to the 14-mg dose have been emphasized here as it is the dose licensed in the EU.
In the TEMSO trial, 1088 patients with RMS (McDonald 2001 criteria [15]) were randomized to receive once-daily oral teriflunomide 14 mg, teriflunomide 7 mg, or placebo for 108 weeks [1, 11]. Teriflunomide 14 mg significantly reduced annualized relapse rate (ARR) (primary endpoint) by 31.5 % (p < 0.001) and reduced the risk of disability progression (key secondary endpoint) by 30.0 % (p < 0.05) versus placebo (Table 2). Teriflunomide 14 mg also reduced total lesion volume [key magnetic resonance imaging (MRI) endpoint] by 67 % versus placebo at week 108 (p < 0.001), the mean number of T1 gadolinium (Gd)-enhancing lesions per scan by a change relative to placebo of 0.80 (p < 0.0001) and the number of unique active lesions per scan by 69 % (p < 0.0001) (Table 2).
In a post hoc analysis of a subgroup of patients from the TEMSO study with high disease activity (two or more relapses in 1 year and with one or more Gd-enhancing lesion on baseline brain MRI; n = 127), a consistent treatment effect of teriflunomide 14 mg compared with placebo was observed for ARR and disability progression [1, 16].
In TOWER, 1169 patients with RMS (McDonald 2005 criteria [17]) were randomized to receive teriflunomide 14 mg, 7 mg, or placebo (Table 1) [1, 12]. The 14-mg dose significantly reduced ARR by 36.0 % (p < 0.0001) and the risk of confirmed disability progression sustained for 3 months by 32.0 % (p < 0.05) versus placebo (Table 2).
In TOPIC, 618 patients with a first clinical demyelinating event were randomized to receive teriflunomide 14 mg, 7 mg, or placebo for up to 108 weeks. Teriflunomide 14 mg significantly reduced the risk of a second relapse by 43 % compared with placebo (p = 0.0087), and the risk of relapse or new MRI lesion, whichever occurred first, by 35 % (p = 0.0003). Significant efficacy on MRI outcomes (total lesion volume, number and volume of Gd-enhancing lesions, and volume of post-Gd T1 lesion component) was also demonstrated [1, 13].
The effectiveness of teriflunomide was compared with that of subcutaneous interferon (IFN)-β-1a in the phase III TENERE study, in which 324 randomized patients were treated for at least 48 weeks. No difference was found between teriflunomide and IFNβ on the primary endpoint of time to failure, defined as confirmed relapse or permanent treatment discontinuation, whichever came first. Overall, patients reported greater treatment satisfaction and less fatigue with teriflunomide than with IFNβ [1, 14, 16].
2.2 Safety and Tolerability Outcomes
The safety analysis included 2047 teriflunomide-treated patients from four placebo-controlled trials: phase II (NCT00475865) [18], TEMSO, TOWER, and TOPIC. Adverse events reported in ≥10 % of patients treated with teriflunomide were diarrhea, nausea, increased alanine aminotransferase (ALT), and alopecia (reported as hair thinning). In general, diarrhea, nausea, and hair thinning were mild to moderate in intensity, transient, and only infrequently led to treatment discontinuation (Table 3) [1].
Mild increases in ALT ≤3× the upper limit of normal (ULN) were more frequently observed in patients receiving teriflunomide (49.6 %) than in those receiving placebo (29.5 %). According to study protocols, patients with confirmed ALT >3× ULN were required to discontinue treatment permanently [14]. The frequency of ALT increase >3× ULN was similar across treatment groups. Increases in ALT occurred mainly within the first 6 months of treatment, and the majority of these increases were reversible following discontinuation of treatment [1].
Minor reductions (<15 % decrease from baseline levels) in white blood cells (WBCs), mainly neutrophils and lymphocytes, have been observed in patients receiving teriflunomide in clinical trials. Most reductions were observed during the first 6 weeks of treatment with no further decrease while patients remained on therapy [1].
No increase in the incidence of serious infections was observed for teriflunomide (2.7 %) compared with placebo (2.2 %); serious opportunistic infections occurred in 0.2 % of patients per group [1]. There was no increased risk of malignancy with teriflunomide treatment [1].
Peripheral neuropathy, including both polyneuropathy and mononeuropathy (e.g., carpal tunnel syndrome), was reported more frequently in patients receiving teriflunomide than in placebo patients. In the pivotal studies, the incidence of peripheral neuropathy confirmed by nerve conduction studies was 1.4 % (13 of 1002 patients) in the teriflunomide group compared with 0.4 % (4 of 997 patients) in the placebo group [1].
Systolic blood pressure >140 and >160 mmHg was observed in 19.9 and 3.8 % of patients receiving teriflunomide compared with 15.5 and 2.0 % of those receiving placebo, respectively. Diastolic blood pressure >90 mmHg was observed in 21.4 % of patients receiving teriflunomide compared with 13.6 % of patients receiving placebo [1].
3 Practical Considerations for Physicians Prescribing Teriflunomide
Physicians must be aware of required assessments before initiation of treatment and monitoring requirements during teriflunomide therapy, as well as contraindications for its use (Tables 4, 5). In addition to the EU SmPC recommendations referred to in this article, national recommendations and guidelines have been issued.
3.1 Considerations Before Initiation of Teriflunomide Therapy
Elevations in liver enzymes have been observed in patients receiving teriflunomide in clinical trials, and teriflunomide treatment is contraindicated in patients with severe hepatic impairment [Child–Pugh class C, where A (5–6 points) is the least severe and C (10–15 points) is the most severe] [1, 19]. ALT/serum glutamic pyruvic transaminase (SGPT) should be assessed before initiation of teriflunomide treatment [1].
Due to the effect of teriflunomide on WBC counts, a complete blood count, including differential WBC and platelet count, should be assessed [1].
Teriflunomide treatment was associated with increases in systolic and diastolic blood pressure in clinical trials [1, 11, 12] and, therefore, blood pressure should be checked [1].
Teriflunomide is contraindicated in women who are pregnant or of childbearing potential if not using reliable contraception, or breast feeding (Table 5). Pregnancy must be excluded before initiation of teriflunomide in women of childbearing potential [1].
For a full list of considerations before initiating teriflunomide, see Table 4.
3.2 Recommendations During Teriflunomide Therapy
During treatment with teriflunomide, liver enzymes should be assessed every 2 weeks during the first 6 months of treatment and every 8 weeks thereafter. In the US prescribing information, monitoring is required at least monthly for 6 months after starting treatment [20]. If ALT/SGPT increases 2–3× ULN, weekly monitoring is advised. Patients with pre-existing liver disease may be at increased risk of developing elevated liver enzymes when receiving teriflunomide and should be monitored closely for signals of liver disease; therapy should be discontinued if liver injury is suspected and/or if elevated liver enzymes >3× ULN are confirmed [1]. It is advised to check patients’ blood pressure periodically during treatment and any blood pressure elevation should be appropriately managed [1]. Teriflunomide treatment should be delayed in patients with severe active infection. Two clinical studies have demonstrated that vaccination with inactive neoantigen (rabies vaccine) or recall antigen (influenza vaccine) were safe and effective during treatment with teriflunomide. The use of live attenuated vaccines may carry an infection risk and should therefore be avoided, as is generally suggested in MS (Table 5) [1].
Women of childbearing age must be advised to use effective contraception during teriflunomide treatment and after treatment until teriflunomide plasma concentration is below 0.02 mg/l [1].
3.3 Recommendations for Treatment-Emergent Situations During Teriflunomide Therapy
A list of recommended management approaches for treatment-emergent clinical situations during teriflunomide therapy is summarized in Table 5.
3.3.1 Pregnancy
Teriflunomide is contraindicated in pregnant women, or women of childbearing potential not using reliable contraception, based on observations of teratogenicity and embryo-lethality in the offspring of teriflunomide-treated rats and rabbits. However, in vitro teriflunomide studies showed no evidence for increased frequency of mutations, and teriflunomide did not cause chromosome breakage in vivo [1]. In rats, teriflunomide administration resulted in a lower sperm count, but fertility was unaffected. No external malformations were observed in the offspring of male rats administered teriflunomide before mating with untreated female rats [1].
In a prospective trial conducted by The Organization of Teratology Information Specialists (OTIS) comparing pregnancies in leflunomide-treated RA patients, RA patients not exposed to leflunomide, and healthy volunteers, leflunomide did not demonstrate any evidence of increased risk for major birth defects, a specific pattern of major or minor anomalies, or an increased risk of spontaneous abortions [21]. Global teriflunomide pregnancy registries are collecting prospective data from pregnancies in the post-marketing setting.
During teriflunomide treatment, women of childbearing potential should discuss plans to stop or change contraception with their treating physician and notify their physician if pregnancy is suspected. If the pregnancy test is positive, the physician and patient must discuss the risk to the pregnancy, and should discuss initiation of the accelerated elimination procedure [1]. Teriflunomide US prescribing information recommends that men wishing to father a child should discontinue and undergo an accelerated elimination procedure [20], although no such recommendation is made in the EU SmPC.
4 Pharmacokinetics of Teriflunomide
There are pharmacological differences between leflunomide and its major metabolite teriflunomide, which also form the basis for the designation of teriflunomide as a new active substance by the European Medicines Agency [16]. Metabolism of leflunomide does not only generate teriflunomide, but other metabolites that may contribute to the leflunomide-specific safety profile. Teriflunomide is only moderately metabolized and is the only component detected in plasma. The primary biotransformation pathway for teriflunomide is hydrolysis, with oxidation as a minor pathway [1]; therefore, no dosage adjustment is necessary for patients with mild, moderate, or severe renal impairment not undergoing dialysis, or patients with mild or moderate hepatic impairment [mild, Child–Pugh class A (score 5–6); moderate, Child–Pugh class B (score 7–9)] [1].
A population pharmacokinetic analysis demonstrated that there is a slow approach to steady-state concentration (~100 days). In patients with MS, the median half-life of teriflunomide was approximately 19 days after repeated 14-mg doses. Teriflunomide is extensively bound to plasma protein (>99 %) and is mainly distributed in plasma. Severe hypoproteinemia (e.g., due to nephrotic syndrome) is therefore a contraindication for treatment with teriflunomide. Food does not have a clinically relevant effect on the pharmacokinetics of teriflunomide [1].
5 Accelerated Elimination of Teriflunomide
Teriflunomide is slowly eliminated from plasma; it takes an average of 8 months to reach plasma concentration less than 0.02 mg/L, although individual variation means it may take up to 2 years. Teriflunomide undergoes enterohepatic circulation, and the accelerated elimination process is thought to interrupt reabsorption of teriflunomide at the intestinal level [1].
Several clinical situations may warrant accelerated elimination of teriflunomide. It should be implemented after discontinuation of teriflunomide in instances where (1) pregnancy is confirmed or (2) skin and/or mucosal reactions develop that raise suspicions of severe generalized major skin reactions (e.g., Stevens–Johnson syndrome or toxic epidermal necrolysis), which have been reported with leflunomide but not in clinical trials with teriflunomide [1]. Accelerated elimination of teriflunomide should also be considered after discontinuation of teriflunomide in cases where a serious infection develops, hematologic disorders or severe hematologic reactions occur, confirmed peripheral neuropathy develops, a woman wishes to become pregnant, or a clinically significant overdose or toxicity of teriflunomide occurs [1].
For accelerated elimination, use of cholestyramine 8 g administered three times daily for 11 days or 50 g of activated powdered charcoal every 12 h for 11 days are recommended. Cholestyramine 4 g three times daily can be used if the higher dose is not well tolerated. All described regimens have been shown to decrease teriflunomide plasma concentrations by >98 %, with cholestyramine being faster than charcoal.
It should be noted that patients receiving oral contraceptives while undergoing accelerated elimination should use alternative contraceptive methods because cholestyramine and activated charcoal may negatively affect the absorption of estrogens and progestogens [1].
6 Interaction with Other Medicinal Products
Metabolism studies conducted in vitro have demonstrated that teriflunomide is not directly metabolized by cytochrome P450 (CYP) or flavine monoxidase enzymes [1], which limits the potential for drug–drug interactions. This is a significant factor differentiating teriflunomide from leflunomide. Furthermore, polymorphisms in CYP 2C19 in patients with RA were associated with different levels of metabolism of leflunomide, and poor metabolizers frequently discontinued their treatment due to adverse events [16, 22]. However, teriflunomide co-administration with potent CYP and transport inducers may decrease the amount of teriflunomide exposure and therefore should be used with caution [1]. A list of pharmacokinetic interactions of teriflunomide on other substances is shown in Table 6.
No waiting period is required when initiating teriflunomide after IFNβ or glatiramer acetate, provided there are no laboratory abnormalities. Due to the relatively long-lasting biological activity of natalizumab, concomitant exposure could occur for up to 2–3 months following discontinuation of natalizumab if teriflunomide therapy were initiated immediately. Therefore, caution is required when switching patients from natalizumab to teriflunomide. Based on the half-life of fingolimod, a 6-week interval is needed for clearance from the circulation, and a period of 1–2 months is commonly needed for lymphocytes to return to normal range. Starting teriflunomide within this interval will result in concomitant exposure to fingolimod, which may lead to an additive effect on the immune system [1].
7 Conclusions
Data from the teriflunomide clinical development program support the positive benefit : risk profile of teriflunomide 14 mg in patients with RRMS when prescribed according to the SmPC. Teriflunomide demonstrated significant and consistent efficacy in TEMSO and TOWER. In addition, positive outcomes on several MRI parameters were observed in the TEMSO study. In the TOPIC study, teriflunomide significantly reduced the risk of relapse in patients with a first clinical episode suggestive of MS. These data support the use of teriflunomide in patients in the early stages of relapsing MS. Teriflunomide has a well-characterized safety and tolerability profile. An understanding of pre-treatment evaluations and on-treatment monitoring will ensure optimal outcomes when using teriflunomide in the clinical setting and facilitate identification of potential safety concerns as well as provide guidance for treatment-emergent clinical situations.
References
European Medicines Agency. Aubagio EU summary of product characteristics. 2014. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002514/WC500148682.pdf. Accessed 20 May 2015.
European Medicines Agency. Gilenya EU summary of product characteristics. 2014. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002202/WC500104528.pdf. Accessed 20 May 2015.
European Medicines Agency. Tecfidera EU summary of product characteristics. 2014.http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002601/WC500162069.pdf. Accessed 12 Oct 2015.
Bar-Or A, Pachner A, Menguy-Vacheron F, Kaplan J, Wiendl H. Teriflunomide and its mechanism of action in multiple sclerosis. Drugs. 2014;74:659–74.
Cherwinski HM, McCarley D, Schatzman R, Devens B, Ransom JT. The immunosuppressant leflunomide inhibits lymphocyte progression through cell cycle by a novel mechanism. J Pharmacol Exp Ther. 1995;272:460–8.
Ringshausen I, Oelsner M, Bogner C, Peschel C, Decker T. The immunomodulatory drug Leflunomide inhibits cell cycle progression of B-CLL cells. Leukemia. 2008;22:635–8.
Li L, Liu J, Delohery T, Zhang D, Arendt C, Jones C. The effects of teriflunomide on lymphocyte subpopulations in human peripheral blood mononuclear cells in vitro. J Neuroimmunol. 2013;265:82–90.
Bar-Or A, Freedman MS, Kremenchutzky M, Menguy-Vacheron F, Bauer D, Jodl S, et al. Teriflunomide effect on immune response to influenza vaccine in patients with multiple sclerosis. Neurology. 2013;81:552–8.
Bar-Or A, Wiendl H, Miller B, Benamor M, Truffinet P, Church M, et al. Randomized study of teriflunomide effects on immune responses to neoantigen and recall antigens. Neurol Neuroimmunol Neuroinflamm. 2015;2:e70. doi:10.1212/NXI.0000000000000070.
European Medicines Agency. Arava EU summary of product characteristics. 2009. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000235/WC500026289.pdf. Accessed 12 Oct 2015.
O’Connor P, Wolinsky JS, Confavreux C, Comi G, Kappos L, Olsson TP, et al. Randomized trial of oral teriflunomide for relapsing multiple sclerosis. N Engl J Med. 2011;365:1293–303.
Confavreux C, O’Connor P, Comi G, Freedman MS, Miller AE, Olsson TP, et al. Oral teriflunomide for patients with relapsing multiple sclerosis (TOWER): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13:247–56.
Miller AE, Wolinsky JS, Kappos L, Comi G, Freedman MS, Olsson TP, et al. Oral teriflunomide for patients with a first clinical episode suggestive of multiple sclerosis (TOPIC): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13:977–86.
Vermersch P, Czlonkowska A, Grimaldi LM, Confavreux C, Comi G, Kappos LK, et al. Teriflunomide versus subcutaneous interferon beta-1a in patients with relapsing multiple sclerosis: a randomised, controlled phase 3 trial. Mult Scler. 2014;20:705–16.
McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin F, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001;50:121–7.
European Medicines Agency. Aubagio assessment report. 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002514/WC500148684.pdf. Accessed 12 Oct 2015.
Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol. 2005;58:840–6.
O’Connor PW, Li D, Freedman MS, Bar-Or A, Rice GPA, Confavreux C, et al. A phase II study of the safety and efficacy of teriflunomide in multiple sclerosis with relapses. Neurology. 2006;66:894–900.
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–9.
FDA. Teriflunomide (Aubagio) prescribing information. 2014. http://www.fda.gov/Safety/MedWatch/SafetyInformation/ucm423101.htm. Accessed 12 Oct 2015.
Chambers CD, Johnson DL, Robinson LK, Braddock SR, Xu R, Lopez-Jimenez J, et al. Birth outcomes in women who have taken leflunomide during pregnancy. Arthritis Rheum. 2010;62:1494–503.
Wiese MD, Schnabl M, O’Doherty C, Spargo LD, Sorich M, Cleland LG, et al. Polymorphisms in cytochrome P450 2C19 enzyme and cessation of leflunomide in patients with rheumatoid arthritis. Arthritis Res Ther. 2012;14:R163.
Poser CM, Paty DW, Scheinberg L, McDonald I, Davis FA, Ebers GC, et al. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol. 1983;13:227–31.
Acknowledgments
Clinical studies were supported by Genzyme, a Sanofi company. This manuscript was reviewed by Stephanie Jurgensen, MPH, and Regine Buffels, MD, of Genzyme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors received no funding for their work on this manuscript. Payment for open access was funded by Genzyme. Writing assistance and editorial support was provided by Catherine Simonson of Fishawack Communications Ltd., and was funded by Genzyme.
Conflicts of interest
A. Chan has received compensation for consulting services and speaking honoraria from Allmiral, Bayer Schering Pharma, Biogen Idec, Genzyme, Merk Serono, Novartis Pharma, Sanofi-Aventis, and Teva Pharmaceuticals, and he currently receives research funds from Biogen Idec, Genzyme, and Novartis Pharma. He has served as the country lead investigator (Germany) for TEMSO and TENERE trials (sponsor: Sanofi).
J. de Seze has received compensation for consulting services and participation in advisory boards from Genzyme.
M. Comabella has received compensation for consulting services and speaking honoraria from Bayer Schering, Biogen Idec, Genzyme, Merck Serono, Novartis, Sanofi, and Teva.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Chan, A., de Seze, J. & Comabella, M. Teriflunomide in Patients with Relapsing–Remitting Forms of Multiple Sclerosis. CNS Drugs 30, 41–51 (2016). https://doi.org/10.1007/s40263-015-0299-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-015-0299-y