Abstract
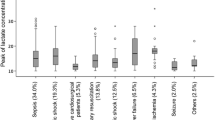
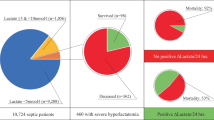
This study aimed to assess the incidence, persistence, and associated mortality of severe hyperlactatemia in a large cohort of unselected critically ill patients. Also, we evaluated the association between 12 h lactate clearance, the timing of severe hyperlactatemia, and the maximum lactate levels with ICU mortality. In this retrospective, single-center study, we used data from the Multiparameter Intelligent Monitoring in Intensive Care III (MIMIC-III) database. Data extracted to screen 23,598 ICU patients for severe hyperlactatemia. A total of 23,598 critically ill patients were eligible for this study. Overall, ICU mortality in the 23,598 ICU patients was 12.1%. Of these, 760 patients had lactate concentration \(\ge\) 10 mmol/L and ICU mortality in this group was 65%. Our findings confirm the association between hyperlactatemia and ICU mortality [odds ratio 1.42 (95% CI 1.35; 1.49; P < 0.001)]. Data for 12 h lactate clearance was available for 443 patients (276 nonsurvivable vs. 167 survival). 12 h lactate clearance yielded a high area under the curve (AUC) of 0.78, (95% CI 0.74 and 0.83). Severe hyperlactatemia is associated with extremely high ICU mortality in a heterogeneous ICU population. Lactate derived variables (the timing and persistence of severe hyperlactatemia, maximum level, and 12 h clearance) are shown to be associated with ICU mortality in patients with severe hyperlactatemia. Our results suggest that maximum lactate level and 12 h lactate clearance were clinically useful prognostic parameters for patients with severe hyperlactatemia.



Similar content being viewed by others
References
Gutierrez G, Wulf M (1996) Lactic acidosis in sepsis: a commentary. Intensive Care Med 22(1):6–16
Mizock BA (2000) Redox pairs, tissue hypoxia, organ dysfunction, and mortality. Crit Care Med 28(1):270–272
Day NP, Phu NH, Bethell DP, Mai NT, Chau TT, Hien TT, White NJ (1996) The effects of dopamine and adrenaline infusions on acid-base balance and systemic haemodynamics in severe infection. Lancet 348(9022):219–223
Levy B, Bollaert P-E, Charpentier C, Nace L, Audibert G, Bauer P, Nabet P, Larcan A (1997) Comparison of norepinephrine and dobutamine to epinephrine for hemodynamics, lactate metabolism, and gastric tonometric variables in septic shock: a prospective, randomized study. Intensive Care Med 23(3):282–287
Druml W, Grimm G, Laggner AN, Lenz K, Schneeweiss B (1991) Lactic acid kinetics in respiratory alkalosis. Crit Care Med 19(9):1120–1124
Levraut J, Ciebiera J-P, Chave S, Rabary O, Jambou P, Carles M, Grimaud D (1998) Mild hyperlactatemia in stable septic patients is due to impaired lactate clearance rather than overproduction. Am J Respir Crit Care Med 157(4):1021–1026
Kraut JA, Madias NE (2014) Lactic acidosis. N Engl J Med 371(24):2309–2319
Cady LD, Weil MH, Afifi AA, Michaels SF, Liu VY, Shubin H (1973) Quantization of severity of critical illness with special reference to blood lactate. Crit Care Med 1(2):75–80
Kaplan LJ, Kellum JA (2004) Initial pH, base deficit, lactate, anion gap, strong ion difference, and strong ion gap predict outcome from major vascular injury. Crit Care Med 32(5):1120–1124
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL (2014) Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med 40(12):1795–1815
Malmir J, Bolvardi E, Afzal Aghaee M (2014) Serum lactate is a useful predictor of death in severe sepsis and septic shock. Rev Clin Med 1(3):97–104. https://doi.org/10.17463/rcm.2014.03.002
Innocenti F, Meo F, Giacomelli I, Tozzi C, Ralli ML, Donnini C, Tassinari I, Caldi F, Zanobetti M, Pini R (2019) Prognostic value of serial lactate levels in septic patients with and without shock. Intern Emerg Med 14(8):1321–1330
Porzio M, Baldini G, Di Maggio C, di Autoformazione MG (2019) Targeting peripheral perfusion versus serum lactate levels in septic shock. Intern Emerg Med 14(6):999–1001
Swenson KE, Dziura JD, Aydin A, Reynolds J, Wira CR (2018) Evaluation of a novel 5-group classification system of sepsis by vasopressor use and initial serum lactate in the emergency department. Intern Emerg Med 13(2):257–268
Callaway DW, Shapiro NI, Donnino MW, Baker C, Rosen CL (2009) Serum lactate and base deficit as predictors of mortality in normotensive elderly blunt trauma patients. J Trauma Acute Care Surg 66(4):1040–1044
Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA, Tomlanovich MC (2004) Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med 32(8):1637–1642
Donnino MW, Miller J, Goyal N, Loomba M, Sankey SS, Dolcourt B, Sherwin R, Otero R, Wira C (2007) Effective lactate clearance is associated with improved outcome in post-cardiac arrest patients. Resuscitation 75(2):229–234
Van Beest PA, Brander L, Jansen SP, Rommes JH, Kuiper MA, Spronk PE (2013) Cumulative lactate and hospital mortality in ICU patients. Ann Intensiive Care 3(1):6
Nguyen HB, Loomba M, Yang JJ, Jacobsen G, Shah K, Otero RM, Suarez A, Parekh H, Jaehne A, Rivers EP (2010) Early lactate clearance is associated with biomarkers of inflammation, coagulation, apoptosis, organ dysfunction and mortality in severe sepsis and septic shock. J Inflamm 7(1):6
Bakker J, Coffernils M, Leon M, Gris P, Vincent J-L (1991) Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock. Chest 99(4):956–962
Bakker J, Gris P, Coffernils M, Kahn RJ, Vincent J-L (1996) Serial blood lactate levels can predict the development of multiple organ failure following septic shock. Am J Surg 171(2):221–226
Arnold RC, Shapiro NI, Jones AE, Schorr C, Pope J, Casner E, Parrillo JE, Dellinger RP, Trzeciak S, Investigators EMSRN (2009) Multicenter study of early lactate clearance as a determinant of survival in patients with presumed sepsis. Shock 32(1):35–39
Falk J (1985) Delayed lactate clearance in patients surviving circulatory shock. Acute Care 11:212–215
Vincent J-l, Dufaye P, Berré J, Leeman M, Degaute J-P, Kahn RJ (1983) Serial lactate determinations during circulatory shock. Crit Care Med 11(6):449–451
Marik P, Bellomo R, Demla V (2013) Lactate clearance as a target of therapy in sepsis: a flawed paradigm. OA Crit Care 1(1):3
Gu WJ, Zhang Z, Bakker J (2015) Early lactate clearance-guided therapy in patients with sepsis: a meta-analysis with trial sequential analysis of randomized controlled trials. Intensive Care Med 41(10):1862
Jansen TC, van Bommel J, Schoonderbeek FJ, Sleeswijk Visser SJ, van der Klooster JM, Lima AP, Willemsen SP, Bakker J (2010) Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med 182(6):752–761
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345(19):1368–1377
Ferreruela M, Raurich JM, Ayestarán I, Llompart-Pou JA (2017) Hyperlactatemia in ICU patients: incidence, causes and associated mortality. J Crit Care 42:200–205
Haas SA, Lange T, Saugel B, Petzoldt M, Fuhrmann V, Metschke M, Kluge S (2016) Severe hyperlactatemia, lactate clearance and mortality in unselected critically ill patients. Intensive Care Med 42(2):202–210
Johnson AE, Pollard TJ, Shen L, Li-wei HL, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG (2016) MIMIC-III, a freely accessible critical care database. Sci Data 3:160035
Mizutani T, Umemoto N, Taniguchi T, Ishii H, Hiramatsu Y, Arata K, Takuya H, Inoue S, Sugiura T, Asai T (2018) The lactate clearance calculated using serum lactate level 6 h after is an important prognostic predictor after extracorporeal cardiopulmonary resuscitation: a single-center retrospective observational study. J Intensive care 6(1):33
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3(1):32–35
Gernardin G, Pradier C, Tiger F, Deloffre P, Mattei M (1996) Blood pressure and arterial lactate level are early indicators of short-term survival in human septic shock. Intensive Care Med 22(1):17–25
Marecaux G, Pinsky M, Dupont E, Kahn R, Vincent J-L (1996) Blood lactate levels are better prognostic indicators than TNF and IL-6 levels in patients with septic shock. Intensive Care Med 22(5):404–408
Moomey CB, Melton SM, Croce MA, Fabian TC, Proctor KG (1999) Prognostic value of blood lactate, base deficit, and oxygen-derived variables in an LD50 model of penetrating trauma. Crit Care Med 27(1):154–161
Schreiber J, Nierhaus A, Vettorazzi E, Braune SA, Frings DP, Vashist Y, Izbicki JR, Kluge S (2014) Rescue bedside laparotomy in the intensive care unit in patients too unstable for transport to the operating room. Crit Care 18(3):R123
Khosravani H, Shahpori R, Stelfox HT, Kirkpatrick AW, Laupland KB (2009) Occurrence and adverse effect on outcome of hyperlactatemia in the critically ill. Crit Care 13(3):R90
McNelis J, Marini CP, Jurkiewicz A, Szomstein S, Simms HH, Ritter G, Nathan IM (2001) Prolonged lactate clearance is associated with increased mortality in the surgical intensive care unit. Am J Surg 182(5):481–485
Abramson D, Scalea TM, Hitchcock R, Trooskin SZ, Henry SM, Greenspan J (1993) Lactate clearance and survival following injury. J Trauma 35(4):584–588
Andersen LW, Mackenhauer J, Roberts JC, Berg KM, Cocchi MN, Donnino MW (2013) Etiology and therapeutic approach to elevated lactate levels. Mayo Clinic Proceedings. Elsevier, Amsterdam, pp 1127–1140
Casserly B, Phillips GS, Schorr C, Dellinger RP, Townsend SR, Osborn TM, Reinhart K, Selvakumar N, Levy MM (2015) Lactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign database. Crit Care Med 43(3):567–573
Hajjar LA, Almeida JP, Fukushima JT, Rhodes A, Vincent J-L, Osawa EA, Galas FR (2013) High lactate levels are predictors of major complications after cardiac surgery. J Thorac Cardiovas Surg 146(2):455–460
Kogan A, Preisman S, Bar A, Sternik L, Lavee J, Malachy A, Spiegelstein D, Berkenstadt H, Raanani E (2012) The impact of hyperlactatemia on postoperative outcome after adult cardiac surgery. J Anesth 26(2):174–178
Vincent J-L, Silva AQ, Couto L, Taccone FS (2016) The value of blood lactate kinetics in critically ill patients: a systematic review. Crit Care 20(1):257
Donnino MW, Carney E, Cocchi MN, Barbash I, Chase M, Joyce N, Chou PP, Ngo L (2010) Thiamine deficiency in critically ill patients with sepsis. J Crit Care 25(4):576–581
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
In this substudy, no patient care was directly involved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gharipour, A., Razavi, R., Gharipour, M. et al. The incidence and outcome of severe hyperlactatemia in critically ill patients. Intern Emerg Med 16, 115–123 (2021). https://doi.org/10.1007/s11739-020-02337-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-020-02337-9