Abstract
Purpose
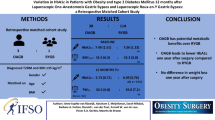
UK guidelines recommend an HbA1c < 8.5% prior to elective surgery. Optimisation of pre-operative glycaemic control can be often difficult. Aim to correlate the effect of pre-operative HbA1c on the peri-operative complication rates and whether elective bariatric surgery should be delayed in poorly controlled diabetics.
Material and Methods
Retrospective data of consecutive patients who underwent laparoscopic Roux-en-Y gastric bypass, one-anastomosis gastric bypass and laparoscopic sleeve gastrectomy during January 2014 and April 2018. Patients were categorised into group 1, non-diabetics with an HbA1c < 6.5%; group 2, well-controlled diabetics with HbA1c between 6.5 and 8.4%; and group 3, poorly controlled diabetics with HbA1c ≥ 8.5%. Primary outcome was peri-operative complication rates.
Results
Group 1 (n = 978), 81.8% female, median (i.q.r.) age 44.0 (34–52) years, median (i.q.r.) BMI 42.0 (38.7–46.7); group 2 (n = 350), 66.3% female, age 51.0 (45–59) years, BMI 41.8 (37.5–46.5); and group 3 (n = 90), 60% female, age 52.0 (45–56) years and BMI 41.4(36.9–44.8). Early complication rates in each group were low, 1.0% vs 1.7% vs 1.1% (p = 0.592). Mean length of stay was 2 days across the groups (p > 0.05). There was no difference in 30-day re-admission rates between groups 2.8%, 2.9% and 3.3% (p = 0.983). At 6 months and 1 year, there was sustained and equal reduction in HbA1c in all groups (p < 0.05).
Conclusion
Patients undergoing metabolic surgery for poorly controlled diabetes achieve non-inferior peri-operative outcomes. Hence, delaying metabolic surgery in an attempt to optimise diabetic control is not justifiable.
Graphical Abstract

Similar content being viewed by others
References
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth IFSO Global Registry Report 2018. Obes Surg. 2019;29(3):782–95.
Schwarz AC, Billeter AT, Scheurlen KM, et al. Comorbidities as an indication for metabolic surgery. Visceral Med. 2018;34(5):381–7.
Landau Z, Kowen-Sandbank G, Jakubowicz D, et al. Bariatric surgery in patients with type 1 diabetes: special considerations are warranted. Ther Adv Endocrinol Metab. 2019;10:2042018818822207.
Membership of the Working P, Barker P, Creasey PE, Dhatariya K, et al. Peri-operative management of the surgical patient with diabetes 2015: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2015;70(12):1427–40.
Butt A, Srivastava V, Sinclair M, et al. Highs and lows: perioperative management of surgical patients with diabetes mellitus. Br J Hosp Med. 2019;80(10):560–1.
Stegenga H, Haines A, Jones K, et al. Identification, assessment, and management of overweight and obesity: summary of updated NICE guidance. Bmj. 2014;349:g6608.
American Diabetes A. 14. Diabetes care in the hospital: standards of medical care in diabetes-2018. Diabetes care. 2018;41(Suppl 1):S144–51.
Steven S, Carey PE, Small PK, et al. Reversal of type 2 diabetes after bariatric surgery is determined by the degree of achieved weight loss in both short- and long-duration diabetes. Diabetic Med. 2015;32(1):47–53.
Jurowich C, Thalheimer A, Hartmann D, et al. Improvement of type 2 diabetes mellitus (T2DM) after bariatric surgery–who fails in the early postoperative course? Obes Surg. 2012;22(10):1521–6.
Mingrone G, Panunzi S, Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386(9997):964–73.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248-56 e5.
Obesity: identification, assessment and management. Clinical guideline [CG189]. 2014; Available from: https://www.nice.org.uk/guidance/cg189/chapter/1-recommendations#surgical-interventions.
Weight loss surgery for Type 2 diabetes.
Zhou K, Wolski K, Malin SK, et al. Impact of weight loss trajectory following randomization to bariatric surgery on long-term diabetes glycemic and cardiometabolic parameters. Endocr Pract. 2019;25(6):572–9.
Panunzi S, Carlsson L, Gaetano A, et al. Determinants of diabetes remission and glycemic control after bariatric surgery. Diabetes Care. 2016;39(1):166–74.
Perna M, Romagnuolo J, Morgan K, et al. Preoperative hemoglobin A1c and postoperative glucose control in outcomes after gastric bypass for obesity. Surg Obes Relat Dis. 2012;8(6):685–90.
Rottenstreich A, Keidar A, Yuval JB, et al. Outcome of bariatric surgery in patients with type 1 diabetes mellitus: our experience and review of the literature. Surg Endosc. 2016;30(12):5428–33.
Maraka S, Kudva YC, Kellogg TA, et al. Bariatric surgery and diabetes: implications of type 1 versus insulin-requiring type 2. Obesity. 2015;23(3):552–7.
Brethauer SA, Aminian A, Rosenthal RJ, et al. Bariatric surgery improves the metabolic profile of morbidly obese patients with type 1 diabetes. Diabetes Care. 2014;37(3):e51–2.
Lannoo M, Dillemans B, Van Nieuwenhove Y, et al. Bariatric surgery induces weight loss but does not improve glycemic control in patients with type 1 diabetes. Diabetes Care. 2014;37(8):e173–4.
Faucher P, Poitou C, Carette C, et al. Bariatric surgery in obese patients with type 1 diabetes: effects on weight loss and metabolic control. Obes Surg. 2016;26(10):2370–8.
Vilarrasa N, Rubio MA, Minambres I, et al. Long-term outcomes in patients with morbid obesity and type 1 diabetes undergoing bariatric surgery. Obes Surg. 2017;27(4):856–63.
Vetter ML, Cardillo S, Rickels MR, et al. Narrative review: effect of bariatric surgery on type 2 diabetes mellitus. Ann Intern Med. 2009;150(2):94–103.
Torquati A, Lutfi R, Abumrad N, et al. Is Roux-en-Y gastric bypass surgery the most effective treatment for type 2 diabetes mellitus in morbidly obese patients? J Gastrointest Surg. 2005;9(8):1112–6; discussion 7-8.
Acknowledgements
The authors would like to specially acknowledge and thank Bariatric Dietitians and Bariatric Nurse Specialists for their dedication and relentless efforts to achieve seamless patient care. They have been instrumental in collection and up keep of the department’s data registry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Statement
For this type of study, formal consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Patients undergoing bariatric/metabolic surgery for poorly controlled diabetes can achieve comparable peri-operative outcomes as patients with optimal diabetes control.
• Post-operative diabetic control may be a better predictor of patient outcomes than pre-operative diabetic control.
• Delaying bariatric/metabolic surgery to optimise diabetic control in refractory cases may not be justifiable.
Presentations
IFFSO 2019, Madrid, Spain.
Rights and permissions
About this article
Cite this article
Samuel, N., Mustafa, A., Hawkins, H. et al. Influence of Pre-operative HbA1c on Bariatric Surgery Outcomes—the Sunderland (UK) Experience. OBES SURG 32, 42–47 (2022). https://doi.org/10.1007/s11695-021-05741-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05741-y