Abstract
Background
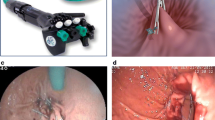
Pose SM is an endolumenal weight-loss intervention in which suture anchors are placed endoscopically in the gastric fundus/distal gastric body. Observational studies of pose have shown safe, effective weight loss. Twelve-month results of a randomized controlled trial comparing weight loss and satiety after pose vs. conventional medical therapy are reported.
Methods
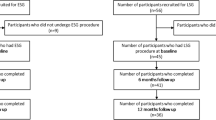
Subjects with classes I–II obesity were randomized in a 3:1 ratio to pose or diet/exercise guidance only (control). Pose subjects received gastric fundus and distal body suture-anchor plications with diet/exercise counseling. Total body (%TBWL) and excess weight loss (%EWL) were assessed at 6 and 12 months. Analysis of covariance (ANCOVA) was used to analyze 12-month %TBWL. Satiety changes were assessed at 6 and 12 months.
Results
From November 2013 to July 2014, 44 subjects were randomized (34, 77.3 % female; mean age, 38.3 ± 10.7 years; body mass index, 36.5 ± 3.4 kg/m2) to pose (n = 34) or control (n = 10) groups in three centers. Mean pose procedure time was 51.8 ± 14.5 min; pose subjects received a mean 8.8 ± 1.3 fundal and 4.2 ± 0.7 distal body plications. Twelve-month TBWL: pose, 13.0 % (EWL, 45.0 %), n = 30 vs. control group, 5.3 % (18.1 %), n = 9; significant mean difference, 7.7 % (95 % CI 2.2, 13.2; p < 0.01). Pose subjects showed significant reductions in satiety parameters (p < 0.001); controls experienced reduced caloric intake and satiety volume (p < 0.05). No serious device- or procedure-related adverse events occurred.
Conclusions
In a randomized controlled trial at 12 months, pose-treated subjects had significantly greater weight loss than those treated with diet/exercise guidance alone. At 6 and 12 months, pose subjects showed significant reduction in satiety parameters.
Study registration: clinicaltrials.gov identifier # NCT01843231




Similar content being viewed by others
References
World Health Organization. Obesity and overweight—fact sheet no. 312. Updated March 2013. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 13 March 2015.
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9(1):88.
Overweight and obesity. Center for Disease Control and Prevention website. www.cdc.gov/obesity/resources/factsheets.html. Accessed March 16, 2015.
Aguilar-Valles A, Inoue W, Rummel C, Luheshi GN. Obesity, adipokines, and neuroinflammation. Neuropharmacology. 2015;96(Pt A):124–34 .Review
Hammond RA, Levine R. The economic impact of obesity in the United States. Diabetes Metab Syndr Obes. 2010;3:285–95.
Cremieux PY, Buchwald H, Shikora SA, Ghosh A, Yang HE, Buessing M. A study on the economic impact of bariatric surgery. Am J Manag Care. 2008;14(9):589–96.
Dee A, Kearns K, O'Neill C, Sharp L, Staines A, O'Dwyer V, et al. The direct and indirect costs of both overweight and obesity: a systematic review. BMC Res Notes 2014;7:242. Review.
O’Brien PE, McPhail T, Chaston TB, et al. Systematic review of medium-term weight loss after bariatric operations. Obes Surg. 2006;16:1032–40.
Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76.
Ribaric G, Buchwald JN, McGlennon TW. Diabetes and weight in comparative studies of bariatric surgery vs conventional medical therapy: a systematic review and meta-analysis. Obes Surg. 2014;24(3):437–55.
Buchwald H, Estok R, Fahrbach K, Banel D, Sledge I. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery. 2007;142(4):621–32.
Nguyen NT, Morton JM, Wolfe BM, Schirmer B, Ali M, Traverso LW. The SAGES bariatric surgery outcome inititiave. Surg Endosc. 2005;19:1429–38.
Afonso BB, Rosenthal R, Li KM, Zapatier J, Szomstein S. Perceived barriers to bariatric surgery among morbidly obese patients. Surg Obes Relat Dis. 2010;6(1):16–21.
Gregory DM, Temple Newhook J, Twells LK. Patients’ perceptions of waiting for bariatric surgery: a qualitative study. Int J Equity Health. 2013;12:86.
Padwal R, Chang H-J, Klarenbach S, Sharma A, Majumdar S. Characteristics of the population eligible for and receiving publicly funded bariatric surgery in Canada. Int J Equity Health. 2012;11:54.
Marmot M. Fair Society, Healthy Lives. The Marmot Review. Strategic review of health inequalities in England post-2010. Executive Summary. 2010. www.ucl.ac.uk/marmotreview.
Mahony D. Bariatric surgery attrition secondary to psychological barriers. Clin Obes. 2013;3(1–2):32–8.
Treato.com. Treato finds 85 % of overweight consumers would not consider having bariatric surgery. PR Newswire. June 30, 2015: http://www.prnewswire.com/news-releases/treato-finds-85-of-overweight-consumers-would-not-consider-having-bariatric-surgery-510919661.html
Martin M, Beekley A, Kjorstad R, Sebesta J. Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Relat Dis. 2010;6(1):8–15.
ASMBS. http://asmbs.org/resources/emerging-technologies-and-procedures-inventory
Verma R, Eid G, Ali M, Saber A, Pryor AD. ASMBS emerging technologies and procedures committee. Emerging technologies and procedures: results of an online survey and real-time poll. Surg Obes Relat Dis. 2015;11(1):161–8.
Espinós JC, Turró R, Mata A, Cruz M, da Costa M, Villa V, et al. Early experience with the incisionless operating platform™ (IOP) for the treatment of obesity: the primary obesity surgery endolumenal (pose) procedure. Obes Surg. 2013;23(9):1375–83.
López-Nava G, Bautistia-Castaño I, Jiminez A, de Grado T, Fernandez-Corbelle JP. The primary obesity surgery endolumenal (pose) procedure: one-year patient weight loss and safety outcomes. Surg Obes Relat Dis. 2015;11(4):861–5.
Espinós JC, Turró R, Moragas G, Bronstone A, Buchwald JN, Mearin F, et al. Gastrointestinal physiological changes and their relationship to weight loss following the pose procedure. Obes Surg. 2015.
Protocol registration. Use of the Incisionless Operating Platform as a Primary Treatment for Obesity vs. Diet-Exercise Alone (MILEPOST). Clinical Trials Identifier NCT01843231. April 22, 2013. https://clinicaltrials.gov/ct2/show/NCT01843231?term=USGI&rank=6
USGI Medical. Protocol: a randomized controlled multicenter study of an incisionless operating platform for primary obesity vs. diet-exercise alone: The MILEPOST study. 2014.
Puigvehi M, Gras-Miralles B, Torra S, Alsina S, et al. Comparison of ad-libitum energy intake and the neuro-endocrine postprandial response as measured during a buffet-type meal and a standardized nutrient drink test. Gastroenterology. 2012;142:S-56.
Meyer-Gerspach AC, Wölnerhanssen B, Beglinger B, Nessenius F, Napitupulu M, Schulte FH, et al. Gastric and intestinal satiation in obese and normal weight healthy people. Physiol Behav. 2014;129:265–71.
Torra S, Ilzarbe L, Malagelada JR, Negre M, Mestre-Fusco A, Aguade-Bruix S, et al. Meal size can be decreased in obese subjects through pharmacological acceleration of gastric emptying (the OBERYTH trial). Int J Obes. 2011;35(6):829–37.
USGI Medical. Randomized controlled multicenter study of an incisionless operating platform for primary obesity vs. diet-exercise alone: the MILEPOST study. TPR41936 Rev F, 2014.
Sjöström L. Review of the key results from the Swedish obese subjects (SOS) trial—a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34.
Heo YS, Park JM, Kim YJ, et al. Bariatric surgery versus conventional therapy in obese Korea patients: a multicenter retrospective cohort study. J Korean Surg Soc. 2012;83(6):335–42.
Shauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Leccesi L, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–85.
Maggard-Gibbons M, Maglione M, Livhits M, Ewing B, Maher HR, Hu K, et al. Bariatric surgery for weight loss and glycemic control in nonmorbidly obese adults with diabetes: a systematic review. JAMA. 2013;309(21):2250–61.
Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:CD003641 .Review
Padwal R, Klarenbach S, Wiebe N, Birch D, Karmali S, Manns B, et al. Bariatric surgery: a systematic review and network meta-analysis of randomized medical versus surgical treatment of type 2 diabetes: the search for level 1 evidence. Obes Rev. 2011;12:602–21.
Buchwald H, Avidor Y, Braunwald E, Pories W, Fahrbach K, Schoelles K. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–56.
Wilson PW, Kannel WB, Silbershatz H, D'Agostino RB. Clustering of metabolic factors and coronary heart disease. Arch Intern Med. 1999;159(10):1104–9.
Korner J, Inabnet W, Conwell IM, et al. Differential effects of gastric bypass and banding on circulating gut hormone and leptin levels. Obesity (Silver Spring). 2006;14:1553–61.
Cummings DE, Overduin J, Foster-Schubert KE. Gastric bypass for obesity: mechanisms of weight loss and diabetes resolution. J Clin Endocrinol Metab. 2004;89(6):2608–15.
Acknowledgments
We would like to thank Stephanie Amlung, PhD, RN, USGI Medical, San Clemente, CA, USA for database integration and management and T. W. McGlennon, M3 LLC, Maiden Rock, Wisconsin, USA, for statistical analysis. We also thank Marcus Radauer, MSc and Jonas Philipp, MD (Austria) and Rochelle Nelissen (the Netherlands) for their assistance in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
As stated in the Methods, all procedures involving human participants were performed in this study in accordance with the ethical standards of the institutional and national research committees and with the 1964 Helsinki declaration and its later amendments.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Disclosures
Manuscript development was financially supported by USGI Medical, Inc., San Clemente, CA, USA. Dr. Miller (Salzburg, Austria), Dr. Espinós (Barcelona, Spain), Dr. Turró (Barcelona, Spain), and Dr. Greve (Heerlen, the Netherlands) received investigator consulting fees from USGI Medical. J. N. Buchwald, Chief Scientific Research Writer and Director, Medwrite LLC, WI, USA received fees from USGI Medical for statistical analysis and manuscript development.
Rights and permissions
About this article
Cite this article
Miller, K., Turró, R., Greve, J.W. et al. MILEPOST Multicenter Randomized Controlled Trial: 12-Month Weight Loss and Satiety Outcomes After pose SM vs. Medical Therapy. OBES SURG 27, 310–322 (2017). https://doi.org/10.1007/s11695-016-2295-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2295-9