Abstract
Since 2007, the Oncofertility Consortium Annual Conference has brought together a diverse network of individuals from a wide range of backgrounds and professional levels to disseminate emerging basic and clinical research findings in fertility preservation. This network also developed enduring educational materials to accelerate the pace and quality of field-wide scientific communication. Between 2007 and 2019, the Oncofertility Consortium Annual Conference was held as an in-person event in Chicago, IL. The conference attracted approximately 250 attendees each year representing 20 countries around the world. In 2020, however, the COVID-19 pandemic disrupted this paradigm and precluded an in-person meeting. Nevertheless, there remained an undeniable demand for the oncofertility community to convene. To maintain the momentum of the field, the Oncofertility Consortium hosted a day-long virtual meeting on March 5, 2021, with the theme of “Oncofertility Around the Globe” to highlight the diversity of clinical care and translational research that is ongoing around the world in this discipline. This virtual meeting was hosted using the vFairs ® conference platform and allowed over 700 people to participate, many of whom were first-time conference attendees. The agenda featured concurrent sessions from presenters in six continents which provided attendees a complete overview of the field and furthered our mission to create a global community of oncofertility practice. This paper provides a synopsis of talks delivered at this event and highlights the new advances and frontiers in the fields of oncofertility and fertility preservation around the globe from clinical practice and patient-centered efforts to translational research.
Similar content being viewed by others
Introduction
Oncofertility is a discipline that merges oncology with fertility and has moved rapidly from the purview of individual champions to an integrated field that is standard of care in many institutions [1]. The necessity for oncofertility has accelerated in parallel to the many life-preserving advances in oncologic care, including earlier diagnostics and the emergence of targeted cancer therapies, methods to reduce radiation dose and field, and localized surgical procedures. With these advances, cancer patients are surviving their disease in increasing numbers and converting what was once a mortal diagnosis to a chronic illness and, in most cases, a curable disease. The data are particularly compelling for pediatric cancer survivors; a patient treated for cancer between the years 1975 and 1979 had a 55% likelihood of surviving 5 years [2, 3]. In children diagnosed between 2005 and 2011, this number rose to 83% [2, 3]. Current estimates are that 1 in 750 adults will be a survivor of childhood cancer [4]. Although these statistics are encouraging, they now also raise concerns about the health of cancer survivors as they age. These concerns are largely related to the off-target effects of the cancer treatments themselves. Cancer survivors are at significant increased risk of second neoplasias, cardiovascular disease, and death at an early age [5]. Another major complication of cancer treatment is compromised reproductive function, which ranges from destruction of gametes to the loss of pituitary and gonadal hormone production. It is in this setting that oncofertility is working to provide information about the iatrogenic effects of drugs on reproductive organs and to develop strategies that will preserve and restore reproductive function and health for cancer survivors. Addressing the complex treatment plans and general health and quality of life concerns of young cancer patients whose fertility may be threatened by their disease or its treatment is a priority, and the Oncofertility Consortium has formally led efforts in this area since 2006 [1, 6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21].
Since its founding, the Oncofertility Consortium not only pioneers the science in the field, but also convenes the leaders and learners in the field annually at the Oncofertility Conference, which showcases groundbreaking research and creating momentum for future activities and initiatives (Table 1) [16, 21, 22]. Each year, the meeting brings together scientists, researchers, clinicians, and others in the fields of reproduction, to discuss contemporary oncofertility and fertility preservation issues, including recent advances in reproductive health for all patients receiving gonadotoxic treatment. As the field has grown, and expanded its focus from fertility preservation in cancer patients to a broader patient population that now includes non-oncologic conditions as well, the diversity of the meeting attendees has also expanded which allows members of our global community to engage in this field of study [8, 15, 21]. The annual conference has become the premier meeting of oncofertility, reflecting the width and breadth of the field. The Oncofertility Conference had been held annually as an in-person event for 13 consecutive years since 2007. The meeting had its origins as a gathering of Principal Investigators (PIs) of the Oncofertility Consortium which was funded through the National Institutes of Health Roadmap Grant for Biomedical Research (UL1DE019587). This venue enabled PIs to deliver updates on their research, but the scope of the meeting expanded as the field grew and speakers and participants began to include all oncofertility stakeholders from around the globe. Starting in 2012, meeting organizers identified a contemporary theme or themes in the multidisciplinary field which was used to frame the conference program and speakers (Table 1). The annual meeting was described by one attendee as a “must attend” event and by 2019, the conference was attended by approximately 250 individuals.
The global COVID-19 pandemic and the unpredictable events of 2020 disrupted the long-running tradition of the in-person Oncofertility Conference. To keep the community safe, the 2020 Oncofertility Conference was canceled. Although it was disappointing to end a decade long tradition of meeting in Chicago, IL for the annual event, we saw this as an opportunity to convene the globe in an unconventional way and capitalize on the momentum of the field and the appetite to gather and connect with others, albeit in a virtual setting. Hosting a large-scale virtual conference enabled the Oncofertility Consortium to continue to showcase innovative research and convene the field in a novel way. The goal of this manuscript is to provide a synopsis of the 2021 Oncofertility Around the Globe virtual conference, including the meeting structure, how it compared to metrics of previous in person meetings, and highlights from the seminal scientific and clinical topics discussed during the meeting.
On March 5, 2021, the Oncofertility Consortium hosted a day-long virtual meeting with the theme of “Oncofertility Around the Globe” to highlight ongoing international clinical care and translational research in the field. The meeting provided an accessible platform for international oncofertility leaders and those new to the field to share their perspectives, discoveries, and vision for the field of fertility preservation from basic science, translational, and clinical angles (Supplementary Fig. 1). The day-long event featured two tracks, and within each track there were six concurrent sessions which consisted of three 20-min presentations with 15 min at the end of each session dedicated to Q&A and discussion. Instead of speakers being organized according to theme and expertise, the speakers at this meeting were organized into tracks based on geographical location to show case the state of the field in North America, South America, Europe, Africa, and Australia. Oncofertility research is being conducted around the globe, so the ability to invite speakers from all over the world to present their cutting-edge research was a distinct advantage of the virtual conference format. By eliminating the need for travel, we were able to secure some of the most renowned speakers in the field who were previously unable to participate in the event due to time, scheduling, and budget constraints. Furthermore, due to budget constraints, we were previously unable to invite more than two international speakers. However, because of the virtual format, the agenda featured 38 total speakers from 6 continents and 17 different countries (Table 2). Many of the speakers were early-career investigators so even virtually, we were able to engage a new generation of oncofertility leaders which helps maintain momentum and the continuity of the field. The virtual setting of the Oncofertility Around the Globe meeting was truly the first time that the field was convened globally. The global reach of the meeting expanded from an average of 201 registrants between 2012 and 2019 to 762 registrants in 2021 (Fig. 1A). Furthermore, the number of countries represented grew from an average of 14 between 2012 and 2019 to 57 countries in 2021 (Fig. 1B, Fig. 2).
Graphs illustrating the growth of the conference in terms of A number of participants and B numbers of countries represented. The number of countries represented is based on self-reported registration information. The change to a virtual format increased overall participation and accessibility. (Note there was no conference in 2020 due to the COVID-19 pandemic.)
The increased number of participants contributed to improved diversity with respect to race, ethnicity and career stage as compared with previously hosted in-person conferences (Fig. 3A, B). Attendees reported gender identity of 72% female, 27% male, and 1% identifying as transgender, genderqueer, non-binary/third gender, or preferred not to say. Self-reported race of attendees was as follows: 53% white, 12% Asian, 12% Black or African American, less than 1% American Indian or Alaskan Native or Native Hawaiian or Other Pacific Islander, 8% some other race, ethnicity, or origin, and 13% of attendees either preferred not to answer, or preferred to self-describe (Fig. 3A). Fifty-five percent of attendees self-identified as not of Hispanic, Latino/a/x, or Spanish origin, 12% identified as Hispanic, Latino/a/x, or Spanish origin, and the remaining 33% not answering or identifying as some other race, ethnicity or origin (Fig. 3B). Thirty-one percent of participants also self-identified as trainees or early-stage investigators, which was up from 24% in 2019.
Graphs illustrating the self-reported demographic data from conference attendees from 2012–2021 including A race and B ethnicity/origin. All data was self-reported and collected at the time of conference registration. Race and ethnicity were not required fields on the data registration form. Percentages are calculated based on individuals who completed these fields on their registrations. Calculations were based on the following number of responses per year: 2012: 97; 2013: 112; 2014: 151; 2015: 186; 2016: 219; 2017: 204; 2018: 200; 2019: 231; 2021: 663
This virtual meeting was a completely new paradigm for the field. Unlike past years, the virtual meeting was free and accessible and as such, it expanded the global reach of the fertility preservation and oncofertility professionals to places previously unexplored. There were three distinct advantages to hosting a virtual conference during the global pandemic. First, the number of attendees nearly tripled and as a result of opening this meeting to a broader audience, the diversity statistics improved as well (Fig. 1A, B; Fig. 3A, B). Second, we reached a new audience, with many participants hailing from countries and areas with limited resources. And lastly, we enhanced trainee representation both as conference participants and as speakers. While the COVID-19 pandemic presented a number of challenges, it also forced us towards a new conference model that enhanced accessibility and visibility for the field.
In the next section of the paper, we summarize the talks presented at this event. This section is organized by four overarching contemporary topics and sub-topics: clinical practice (females, males, pediatrics, and DSD, gender diverse, and non-oncologic cases), patient-centered fertility preservation, translational research (males and females), and global perspectives. These talks represent some of the most cutting-edge research being conducted in the field of fertility preservation.
Conference session synopsis
Clinical practice — females
For patients who are unable to delay cancer treatment, several alternative ovarian stimulation protocols have been developed and evaluated. Mitchell P. Rosen, MD, described the use of random start protocols, which have been shown to achieve comparable oocyte yields and pregnancy outcomes compared to conventional protocols. Double stimulation, during the follicular phase and luteal phase of the same menstrual cycle, allows for two oocyte retrievals in the shortest possible time. Many studies have shown that random start, luteal phase start [23], and conventional start protocols are not significantly different in terms of the time to initiation of chemotherapy [24, 25] or outcomes. In patients with estrogen-sensitive cancers, the addition of letrozole/tamoxifen to random-start protocols results in a significant decrease in peak estradiol level without compromising the length of stimulation, oocyte yield, or oocyte quality compared with standard protocols. Importantly, studies suggest there is no significant difference in survival rate among patients who underwent fertility preservation and those who did not [24, 26]. For those undergoing stimulation after chemotherapy, a 6-month waiting period is recommended to avoid birth defects and achieve maximal ovarian recovery after treatment.
Use of oocyte freezing among adolescent patients has been uneven, due to perceived lower efficacy of fertility preservation techniques in pre-pubertal or early pubertal populations, questions about disposition of unused gametes, variability in physician and hospital attitudes towards providing egg freezing services, and anesthesia restrictions in younger patients. Mary Ellen Pavone, MD, described studies that show no significant differences between younger and older patients in terms of oocyte retrievals, ovarian stimulation dosing, anti-Mullerian hormone (AMH) levels, and peak estradiol [27]. Based on data showing higher incidences of aneuploidy in eggs from younger girls [27], genetic screening for aneuploidy may improve outcomes for women who cryopreserved oocytes as adolescents. Interdisciplinary teams should include a psychologist or social worker and a patient navigator to support parents and patients, provide education, obtain both consent and assent, and discuss unused oocyte disposition.
Ovarian tissue cryopreservation (OTC) for future use in ovarian tissue transplantation (OTT) is available to pre-pubertal patients or when immediate chemotherapy is required [28]. Cryopreserved tissue can be transplanted to the native ovary or within a peritoneal pocket [29]; the pocket location may need to shift in patients who underwent pelvic irradiation and have poor vascularization of the peritoneum. Marie-Madeleine Dolmans, MD, PhD, described that OTC is most often performed before initiation of treatment, but because primordial follicles are quiescent and more resistant to damage, it may also be an option after chemotherapy. In almost all cases of OTT, endocrine function is restored, with FSH levels dropping and menstruation resuming approximately 4 months after transplantation [30]. Long-term studies report sustained function of the grafts, out to 11 years [29, 31]. The number of live births following OTT is exponentially increasing [32]. In data from three centers, one in two women had a pregnancy following OTT and 41% had at least one live birth [33]. For patients with some chemotherapy before OTC, the percentage of women with at least one birth was comparable, further indicating that exposure to chemotherapy is not a contraindication for OTC [29, 33].
Since the first OTC in Denmark in 1999, only 14% of patients have returned for OTT and 59% still have their tissue in storage. Stine Gry Kristensen, PhD, described a high return rate for OTT among women older than 30 years at OTC, and that 71% of patients return within 5 years of OTC [34]. Young patients with breast cancer had lower return rates, while young patients with lymphoma had similar return rates as older patients [34]. Return rates for OTT are dependent on the diagnosis, age of the patient at OTC, and follow-up time, which calls for new measures for reporting and comparing the OTT rates within cohorts and among centers worldwide. For patients above the age of 35 years at the time of OTC the reproductive outcomes after OTT are poor [35, 36] and the efficacy of the procedure is limited due to a significant loss (70%) of follicles occurring during transplantation as a result of ischemia and reperfusion injury [37, 38]. New methods to improve follicular survival post-OTT are being investigated, including adipose tissue-derived stem cells to increase follicle survival by enhancing vascularization [39], and intraperitoneal administration of the antioxidant N-acetylcysteine (NAC) to protect follicles from ischemia–reperfusion injury [40].
Clinical practice — males
As most male cancer survivors express a wish to become biological parents, Joshua A. Halpern, MD, MS, suggested that every patient be treated as if they will lose their fertility potential and be offered sperm cryopreservation as early as possible before cancer treatment is started [41]. Decades of data have shown that clinical outcomes are not different between fresh and cryopreserved sperm, with a frozen-thaw survival rate of about 75% [42]. A formal oncofertility program can help overcome persistent barriers to fertility preservation, at the level of the patient, physician, and system. Such programs include training sessions for nurses and physicians, oncology grand rounds focused on oncofertility, use of electronic medical record prompts for referral, a dedicated patient navigator, and a patient-facing website in multiple languages.
Clinical practice — pediatrics
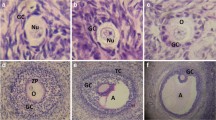
The growth in OTC for fertility preservation in pediatric patients has spurred advances in surgical technique. Erin Rowell, MD, discussed the development of a new porcine model of pediatric laparoscopic oophorectomy that is being used to test an ultrasound-based tissue removal technique. Using this model, researchers found that when the ultrasound device is placed far from the cortical capsule compared to close to the capsule, various markers of ovarian tissue cortex health were improved (ovarian tissue consumed glucose and produced less lactate and also produced more estradiol) [43]. Dr. Rowell also described their program’s surgical technique for pediatric laparoscopic oophorectomy, including optimal port placement at different pediatric developmental stages and technical principles such as scope placement, confirmation of ovary symmetry, and a “no touch technique” in which the mesovarium is grasped directly adjacent to the cortical tissue, stretched, and incised with an ultrasound energy device using a medial to lateral approach > 1 cm distant from the cortex [44]. After cutting the ovarian artery, the organ is drawn carefully through the umbilicus using an endoscopic retrieval bag with preservation of the adnexal structures — specifically the fallopian tubes — for future reproductive use.
Leena Nahata, MD, reviewed the contributions of the Pediatric Initiative Network, an international group of providers dedicated to preserving and protecting the fertility of children and adolescents at risk for infertility due to either underlying medical conditions or their treatments [45, 46]. A best practices committee was established to develop strategies to optimize fertility-related care, while a research committee set out to design and implement collaborative multi-site research to advance care. A navigator subcommittee was developed with the goal of improving access to care, and more recently, an education committee was formed to improve patient and clinician communication and develop resources on fertility and reproductive health. The PIN recently created a practical roadmap that highlights the importance of team structure and the use of a fertility navigator, organized a legislative working meeting to address insurance issues faced by front-line providers and to discuss practical approaches for advocacy, and developed a Risk Stratification System for clinicians to reference during fertility consults [22, 47]. They are now focused on missed opportunities for counseling on reproductive health and survivorship, knowledge gaps in fertility testing, when to refer for fertility preservation, psychosexual health, how AMH should be interpreted in the pediatric population, and creating an international tissue repository imaging system.
Clinical practice — DSD, gender diverse, and non-oncologic cases
Several patient groups have fertility-related concerns that can potentially be addressed with fertility preservation; each group has a unique set of considerations that affect the risk/benefit calculation.
Veronica Gomez-Lobo, MD, described that in individuals with accelerated follicular loss such as those with Turner syndrome and classic galactosemia, oocyte cryopreservation is probably the best option for those who have reached puberty; however, most of these individuals experience premature ovarian failure prior to menarche and many have advocated for ovarian tissue cryopreservation earlier in life [48, 49]. For example, individuals with galactosemia younger than five may have a normal primordial follicle pool, in which case arrest of follicle loss may be accomplished by OTC [50]. However, laparoscopic removal of an entire ovary may further reduce of the ovarian reserve preventing the possibility of puberty and post-pubertal oocyte cryopreservation in those who were destined to achieve this milestone. It is also unclear whether follicle loss after thawing, and transplantation is greater for women with these conditions. The risk/benefit of performing OTC in individuals with galactosemia is further confounded by the fact that there are reports of high rates of conception despite a diagnosis of premature ovarian insufficiency [50]. In patients with autoimmune disorders, there are significant knowledge gaps regarding fertility potential and long-term gonadal function, and fertility counseling is not part of standard of care in these patients.
In children with differences in sex development (DSD), impaired fertility may be caused by abnormal gonadal development, abnormal hormone production and/or action, assumed infertility due to discordant gender identity and gametes, or anatomic barriers such as the lack of a uterus. Courtney Finlayson, MD, described that, unlike in pediatric oncology, gonadal tissue cryopreservation is not typically offered to DSD patients due to concerns about the health of the gonadal tissue, the presence and quality of germ cells, and patient age. In many DSD diagnoses, gonadal cancer risk was thought to be high and early gonadectomy was recommended. Yet several recent publications have reported the presence of germ cells in DSD, more often in younger patients (0–3 years of age) [51]. Another study reported the presence of germ cells in a patient diagnosed with complete androgen insensitivity syndrome (CAIS) [51]. Dr. Finlayson advocates for an evolving approach to fertility preservation that moves away from traditional assumptions of infertility in DSD patients.
Emilie K Johnson, MD, MPH, FACS, echoed Dr. Finlayson’s call for a shift in the paradigm of DSD gonadal management, from a recommendation for early gonadectomy to individualized gonadectomy with multidisciplinary evaluation and patient involvement. Gonadal tissue cryopreservation (GTC) at the time of gonadectomy should be discussed as an experimental fertility preservation option for DSD patients. Dr. Johnson described the DSD GTC research protocol at Lurie Children’s Hospital, which consists of preoperative evaluation and counseling, postoperative pathology discussion, and family decision-making [52]. Protocols must include processes for accurate identification of candidates for GTC and sophisticated germ cell quality assessment and assuring that families understand that advances in Assisted Reproductive Technologies (ART) may be necessary for the gonadal tissue to be used to produce a biological child.
Molly B. Moravek, MD, extended the discussion to include fertility preservation in gender diverse patients. In transfeminine individuals, the effects of estradiol exposure on reproductive anatomy have been assessed via semen analyses (count, motility, and morphology) and histological changes, with mixed results. Transfeminine individuals can undergo fertility preservation, though the outcomes may not be optimal if they have already started on hormone therapy [53, 54]. Typical semen parameters are often also affected in transgender women who have never been exposed to hormone replacement therapy, though the underlying pathophysiology is unclear [55]. In transmasculine individuals, several studies have examined pregnancy, fertility preservation, and ART outcomes. While transmasculine people are able to carry a pregnancy to term, the efficiency of conception attempts, and the long-term effects of testosterone remain unclear. One study found that individuals who had started testosterone before ovarian stimulation had significantly lower numbers of oocytes retrieved [56], while another showed improved parameters [57]. Researchers at Michigan are using a mouse model to study the effects of testosterone on reproductive parameters and the reversibility of the transmasculine transition. In this model, testosterone causes reproductive perturbations at the level of the ovary, though without an effect on overall ovarian reserve [58]. In reversibility studies, they found cyclicity resumption, persistent histological differences (assumed to be time dependent), and production of offspring [58].
Patient-centered fertility preservation
Fertility preservation and ART require patient-centered care, with shared decision-making and multidisciplinary support for patients and their families.
Gwendolyn Quinn, PhD, discussed the ethical issues that arise in fertility preservation in adolescents and young adults (AYA). Decision-making requires a clarification of the decisions to be made, a consideration of alternative options and consequences, and selection of the option that is the best for each situation. Ethical concerns are related to how prepared patients are to make these decisions in a fully informed way and who decides what happens and when. Healthcare providers vary in their approach to fertility preservation consultations, with some clinicians comfortable with full discussions of options and others trying to balance patient satisfaction with resource limitations and insurance coverage issues. Tools that clarify decision-making can reduce uncertainty. The overarching goal is to help patients make autonomous decisions about fertility preservation and reduce the chance of future decisional regret. Healthcare clinicians have an ethical obligation to inform individuals about potential threats to fertility, provide referrals to specialists, and document these conversations in the patients’ medical record.
Discussions about fertility preservation require an understanding of fertility risk. Leslie C. Appiah, MD, discussed reproductive late effects among AYA survivors. The risk of ovarian failure is 12% and of testicular failure is 66% after treatment of childhood cancer, while pregnancy rates decrease nearly 40% for young adult survivors. Radiation-induced uterine injury occurs in 30% of survivors, leading to a 2- to fourfold increased risk of premature and low-birth weight babies [59,60,61]. Dr. Appiah shared a guide for determining infertility risk according to condition and treatment with gonadotoxic agents [47]. Female patients should wait at least six, and ideally 12 months after treatment to attempt conception [62,63,64,65,66]. Ovarian reserve testing (ORT) based on AMH level reflects primary and secondary follicle function [67,68,69,70]. ORT should be performed starting 1 year after treatment is completed for patients desiring fertility assessment and continued until family planning is complete or no longer desired [47, 70, 71]. In males, sperm DNA breakage can be present for up to 24 months after cancer therapy, and providers recommend that men wait at least 12 months to conceive [72]. Dr. Appiah noted that the gonadotoxicity of newer treatments is not known and may be a threat to future fertility of childhood cancer patients [73, 74].
In addition to infertility, cancer and its treatment can have adverse effects on psychosexual well-being and sexual function. Antoinette Anazodo, MD, PhD, spoke about the development of a patient-reported outcome measurement of reproductive survivorship (RS-PROM) to help identify sexual and reproductive concerns experienced by cancer patients in the survivorship period. At her institution, two survivorship clinics currently see 397 patients 5 years of age and older, starting at the end of the treatment. Many reproductive issues are covered in the survivorship clinics, but psychosexual and sexual dysfunctions are rarely covered. The RS-PROM questionnaire helps physicians understand the unique patient experience and provides patients an opportunity to discuss concerns about reproductive symptoms with healthcare professionals [75]. Using the RS-PROM, 68% of patients reported at least one concern about their sexual health and function after cancer, 85% felt that having an active sex life was very important, and 64% feared they would not be able to have children, yet 43% reported no communication with healthcare personnel about sexual and reproductive issues. Dr. Anazodo believes the RS-PROM may help address survivors’ oncofertility needs in routine survivorship care in the future.
Helping patients and their families understand and synthesize complicated information about cancer, cancer treatment, and fertility preservation is essential to ensuring ethical, patient-centered care. Kristin Smith and Stacy Whiteside, APRN, reviewed the role of the oncofertility patient navigator, who works at the intersection of reproductive endocrinology and infertility [52] and oncology. Navigators can come from a variety of backgrounds, but they must possess skills in communication and education, be knowledgeable in healthcare systems and insurance and finance, and synthesize knowledge from many different care teams. Although there are no formal courses for patient navigators, online training opportunities are available. Funding for navigators can be acquired through consult service revenue, downstream revenue, grants or philanthropic funds, or utilization of full-time employees in other positions. Currently, legislative efforts are focused on mandated coverage for patient navigators. Sharing of program structure and outcomes data among sites will be important for building effective navigation programs with standardized procedures and training.
Translational research — females
Ovarian toxicity and fertoprotection
According to Karla Hutt, PhD, the ideal pharmacological fertoprotectant would ultimately eliminate the need to harvest and cryopreserve oocytes, embryos, and ovarian tissue to preserve fertility. Understanding the mechanisms that underlie the gonadotoxicity of cancer treatments is essential for developing new methods to protect the ovaries during treatment. Dr. Hutt described her lab’s research on the role of the PUMA apoptotic pathway in triggering oocyte death, with the loss of PUMA protecting oocytes from apoptosis following chemotherapy treatment [76]. They also found that primordial follicle oocytes have the capacity for efficient DNA repair that may restore oocyte quality and fertility potential [77].
Shuo Xiao, PhD, provided an update on research into the effects of doxorubicin on the ovary and fertility. Doxorubicin is toxic to growing follicles in vitro and in vivo, rapidly inducing apoptosis of the granulosa and theca cells as well as the oocyte, and can also activate primordial follicles, leading to an increase in primary follicles and an indirect depletion of the ovarian reserve [78]. Dr. Xiao also found that doxorubicin toxicity is age-dependent. In 5-day-old mice, doxorubicin reduced the primordial follicle pool by 84%; in 21-day-old mice, by 65%, and in 8-week-old mice, by 55% [79, 80]. Older mice might have higher baseline levels of AMH, which may protect the primordial follicle pool from either overactivation or atresia when doxorubicin is administered. Future studies will investigate the potential role of inflammation and fibrosis in doxorubicin-induced primordial follicle apoptosis and atresia.
Understanding the mechanisms by which chemotherapeutic agents deplete the ovarian reserve is also important for educating and advising patients infertility risk before they undergo treatment. Dr. Hutt noted that mice treated with the relatively new PARP inhibitor olaparib for 28 days have normal estrous cycles, ovulation, number of growing follicles, and serum AMH levels, but the primordial follicle pool is depleted by 46% [81]. Thus, women treated with PARP inhibitors may present with normal AMH and menstrual cycles yet have a reduced ovarian reserve that affects fertility.
Kara N. Goldman, MD, explained that fertoprotective agents should aim to preserve the primordial follicle pool rather than targeting growing follicles, which may explain why evidence supporting a protective effect of Gonadotropin-releasing hormone (GnRH) agonists has been mixed [82,83,84,85]. Dr. Goldman described the rationale for usage of mammalian target of rapamycin (mTOR) inhibitors as fertoprotectants, reviewing that mTOR upregulation is critical to primordial follicle activation [86,87,88,89,90,91]. The mTOR pathway is upregulated in 80% of cancers and mTOR inhibitors are FDA-approved for the treatment of a number of benign and malignant conditions, making this pathway an attractive target for pharmacologic fertoprotection. Using a murine model of treatment with mammalian target of rapamycin complex 1 (mTORC1) inhibitors and dual mTORC1/2 inhibitors alongside alkylating chemotherapy, Dr. Goldman’s group noted a downregulation of mTOR activity, a twofold increase in the number of primordial follicles, and preservation of normal litter sizes compared to mice treated with chemotherapy alone [92]. Her group is currently evaluating the effect of mTOR inhibitors on fertility outcomes, offspring survival, and overall health.
David Pepin, PhD, focused on the mechanisms of uterine and ovarian protection from chemotherapy by AMH/Mullerian inhibiting substance (MIS), which is produced by early antral follicles and acts in a paracrine fashion to inhibit primordial follicle activation [93]. Dr. Pepin’s lab engineered a more potent recombinant form of MIS protein as well as an adeno associated virus 9 (AAV9) containing MIS [94, 95]. Mice treated with AAV9-MIS showed suppressed follicle proliferation, resulting in a smaller ovary and a significant reduction in the number of primary, secondary, antral, and atretic follicles [95]. Administration of two doses of doxorubicin concurrent with MIS led to maintenance of the primordial follicle pool compared to controls, and protection of primary and secondary follicles [95]. MIS had an anti-apoptotic effect on follicles 24 h after doxorubicin treatment, with reductions in cleaved PARP and cleaved caspase 3 [95]. MIS-treated mice produced twice as many pups as control mice [95]. AMH/MIS may also have protective effects on the uterus during chemotherapy, where it appears to delay repair of the uterus by suppressing progenitor cell proliferation during chemotherapy [96].
Ovarian tissue cryopreservation and transplantation
With removal of the “experimental” label in 2018, use of OTC has expanded and translational research is laser focused on improving tissue freezing and optimizing follicle survival in transplanted tissues. Mary Zelinski, PhD, discussed the functional evaluation of transplanted vitrified ovarian tissue in nonhuman primates. Vascular flow to the tissue can be evaluated in vivo with contrast-enhanced ultrasound (CEUS) or computed tomography (CT) imaging, which can predict early tissue function, return of ovarian cyclicity, and production of competent oocytes [97, 98]. Heterotopic transplantation of vitrified ovarian cortex to omental sites was found to be associated with greater blood volume and vascularization compared to subcutaneous sites in the arm [97]. Oocytes collected from heterotopically transplanted vitrified ovarian tissue have produced viable offspring, underscoring clinical feasibility and efficacy. Standardized vitrification protocols, media, and training of laboratory personnel are needed to ensure quality control.
Wen Li, MD, PhD, described a novel method of applying urinary bladder matrix (UBM) to improve OTT efficiency. Promoting neovascularization of the graft is crucial to maximize follicular survival following transplantation. UBM is a biodegradable, acellular matrix membrane with added angiogenic factors (VEGF and b-FGF) that has been shown to regulate the immune microenvironment, promote angiogenesis, and reduce inflammation [99]. In a study in rats, ovarian tissue was treated with either VEGF, UBM, or control media, then transplanted under the renal capsule. After 4 weeks, the transplanted ovarian tissue in the UBM group was larger, contained more follicles of all sizes, and showed less fibrosis and atresia and greater neovascularization than the VEGF and control groups [99]. The rats in the UBM group also had lower levels of FSH and higher levels of AMH. Current work is examining the mechanisms underlying the effects of UBM on transplanted ovarian tissue.
Methods to overcome the current limitations and potential risks of OTC include the development of scaffolds that can support follicle development in vivo. Monica M. Laronda, PhD, described the development of a bioprosthetic ovary that recreates the follicular microenvironment — both physical and biochemical — to prevent premature primordial follicle activation, improve transplantation success rates, and increase the longevity of hormone production. Research has demonstrated follicle growth, expansion, and ovulation in 3D printed scaffolds, producing eggs that can be fertilized and lead to live birth in mice [100]. Techniques such as decellularization, reconstituted tissue papers, and 3D printing have also been used to recreate bioprosthetic ovary environments with specific extracellular matrix-associated biochemical cues, referred to as the matrisome [101,102,103,104,105]. Future studies include the development of a specialized 3D printable gel containing specific proteins and rigidity to support follicle activation and folliculogenesis.
In vitro techniques
The ability to culture early-stage follicles, activate them, grow them, and induce oocyte maturation in vitro will further expand fertility preservation options, particularly for pre-pubertal patients who are unable to undergo ovarian stimulation. Robert Gilchrist, DSc, discussed the advantages of oocyte vitro maturation (IVM) techniques for fertility preservation. Cumulus oocyte complexes (COCs) can be collected from antral follicles with or without ovarian simulation or from ovarian tissue prior to OTC and matured in vitro at short notice [106,107,108,109,110]. Although still experimental, oocytes from very small antral follicles can also be collected and developed in vitro prior to IVM using a pre-IVM step [111, 112]. Dr. Gilchrist described the a biphasic IVM CAPA technique called CAPA, in which oocytes are cultured in pre-IVM for 24 h followed by a 30-h maturation period designed to prolong germinal vesicle arrest and promote gap junction communication, which is followed by a 30 h maturation period [111,112,113,114]. In their study, 49% of oocytes developed to MII using standard IVM and 64% using the CAPA technique [114]. Using oocytes collected from ovarian tissue and matured with standard IVM, most mature oocytes did not progress to the blastocyst stage, while a small number progressed in the CAPA group [115]. These techniques may make it possible to eliminate ovarian stimulation for fertility preservation and provide a fertility preservation option for those who cannot delay treatment, have hormone-sensitive cancers, or prepubertal patients, and for clinics that do not have the technical skills to provide OTC.
Kazuhiro Kawamura, MD, PhD, described his research on harnessing the intracellular signaling system involved in egg activation — the phosphatidylinositol 3-kinase (PI3K) signaling pathway — to access dormant follicles in the ovaries of patients with POI. The PI3K pathway inhibits FOXO3 and is negatively regulated by PTEN [116]. After birth, PTEN or FOXO3 deletion leads to activation of dormant primordial follicles [117, 118]. Dr. Kawamura cultured fragmented cubes of cryopreserved ovarian cortical tissue with PTEN inhibitors and PI3K activators for 2 days to activate the dormant follicles, then auto transplanted the cubes back into patients. Mature eggs were retrieved for in vitro fertilization and embryo transfer, and successful pregnancy was achieved for 36.3% of patients [119,120,121]. The possibility of activation of malignant cells existing in ovarian tissue by the PI3K activation treatment cannot be excluded, making this treatment risky for oncofertility patients. Dr. Kawamura established a safer approach such as a drug-free in vitro activation based on suppression of Hippo signaling pathway that would only require a single surgery without PI3K activation [122,123,124].
The ultimate goal of in vitro follicle growth is to produce mature oocytes that can be fertilized and implanted to achieve pregnancy and healthy offspring. José Ricardo de Figueiredo, PhD, DVM, discussed his work to improve the efficiency of in vitro survival, growth, and maturation of oocytes in ruminant animal models. Primordial follicles from ruminant ovaries can be activated in in vitro culture using hormones, growth factors, and antioxidants, and the development and oocyte maturation of primordial follicles has been achieved with fibrin alginate scaffolds and supplemented media [125]. The “artificial ovary network” was established in Brazil with the goal of achieving pregnancy with in vitro cultured caprine follicles. Following in vitro follicle growth, maturation, and fertilization, a single embryo was transferred to a recipient goat, and pregnancy was confirmed after 30 days [126]. Unfortunately, the pregnancy was lost on day 46. The network continues to optimize in vitro follicle growth conditions to achieve a full-term pregnancy and produce viable offspring.
Translational research — males
Rod T. Mitchell, MBChB, PhD, described the establishment in 2015 of a two-site UK program for fertility preservation in prepubertal boys, which now has stored tissue from more than 400 patients. Patient selection for testicular tissue cryopreservation is complicated by a lack of precision in assigning gonadotoxicity to treatments. One commonly used method to calculate gonadotoxicity is the Cyclophosphamide Equivalent Dose (CED), in which each drug in an alkylating group is given a gonadotoxicity relative to cyclophosphamide [127, 128]. Total CED is then calculated based on dose to predict likelihood of azoospermia. While widely used for alkylating chemotherapies, the CED does not apply to platinum-based agents, which are also gonadotoxic [129]. Dr. Mitchell described a hanging drop system, in which human testicular tissue is exposed to an agent and the reduction in spermatogonia and spermatogonial stem cell (SSC) populations is assessed [130]. Xenograft models can be used to assess the effects of longer exposure.
Functional sperm can be generated from transplanted human testicular tissue or cells [131]. In one method, isolated SSCs are transplanted directly into the seminiferous tubules to restore spermatogenesis [132, 133] A second method involves transplantation of whole tissue to regenerate spermatogenesis, followed by retrieval of mature sperm for intracytoplasmic sperm injection (ICSI) [134,135,136].
Kyle Orwig, PhD, described his work in macaques demonstrating the safety and feasibility of testicular stem cell and testicular tissue transplantation. Testicular tissue biopsies were collected from prepubertal monkeys, cut into 9 to 25 mm cubed pieces and cryopreserved by controlled slow rate freezing. In one study, tissues were thawed and digested with enzymes to produce a testicular cell suspension (including spermatogonial stem cells) that was transplanted, under ultrasound guidance, into the testes of chemotherapy treated, infertile males. Transplanted stem cells restored normal spermatogenesis and ejaculated sperm were competent to fertilize rhesus eggs [133, 137]. In another study, immature prepubertal testicular tissue pieces were thawed and transplanted intact under the back skin or scrotal skin of chemotherapy-treated male monkeys. When transplanted tissues were collected 8–12 months later, complete spermatogenesis was observed. Sperm were used to fertilize rhesus eggs and produced an embryo that was transferred to a surrogate female, resulting in a pregnancy and birth of a healthy baby girl named Grady (Graft-derived baby) [138].
Human testis xenotransplants have so far not been able to generate sperm, possibly because the supporting somatic cell populations are not mature [139]. To investigate this possibility, Dr. Mitchell’s group grafted human fetal tissue to mice exposed to human chorionic gonadotropin (hCG). Those treated with hCG produced mature somatic cells, but germ cell development did not occur. Using pre-pubertal tissue with exposure to pubertal hormones yielded similar results [140]. Evidence supports scrotal/testicular tissue transplant followed by recovery and extraction of sperm for ICSI; however, this procedure should only be performed in adults as part of an ethically approved research study with systematic follow-up. The safety of autologous human testicular transplantation also needs to be evaluated, in particular the risks of reintroducing malignancy.
The epigenetic stability of germ cells after storage is another important consideration [131, 141, 142]. While there is currently evidence of stability following spermatogonia cryopreservation in adult males, more information is needed in prepubertal cases. Prepubertal boys have not yet started producing mature sperm; therefore, research is focused on optimizing the preservation of SSCs and development of mature sperm after thawing.
Continuing the dialogue on oncofertility — global perspectives
As oncofertility and fertility preservation have expanded across the globe, it has encountered various social, cultural, geographic, educational, and economic challenges. Several speakers shared perspectives on oncofertility in their countries, underscoring significant gaps that limit patient access.
Ellen M. Greenblatt, MDCM, shared the current landscape of oncofertility in Canada. She estimated that 50% of reproductive-aged Canadians do not have access to publicly funded Oncofertility services, and all costs are currently covered in only one province (Quebec). Funded sperm and egg freezing for oncofertility exists only in Quebec and Ontario. There are 42 fertility/IVF centers in Canada and many have smaller regional satellites, yet half of Canadians live in areas without an IVF clinic. Non-profit charity programs such as Fertile Future, which runs the Power of Hope Program, offset costs of oncofertility across Canada. A recent survey of IVF clinics found that publicly funded oncofertility treatment does not cover the cost of medication and storage. Of IVF centers that are not publicly funded, most estimated an average cost for oncofertility care of more than $3500. Most clinics offer sperm banking and clinics reported an average of 5–30 oncofertility egg freezing cycles/year.
Maria Teresa Bourlon, MD, described a similar challenge with oncofertility accessibility in Mexico. Though the technology is available, it is limited to a small population and in private clinics. A recent survey among breast cancer patients in Mexico found that while 44% had fertility preservation concerns and 22.5% changed their treatment options because of these concerns, only 3% could afford fertility preservation (n = 134). Dr. Bourlon’s group also found that fertility preservation for testicular cancer patients was feasible as long as funding was available; 30% of patients who received grant support and early referral completed biological reproduction assessment and 20% completed sperm cryopreservation. In addition to financial barriers, conservative religious, cultural, and ethical attitudes in Mexico have limited more widespread use of oncofertility. Patients in Mexico receive little information about fertility risks and very few pursue cryopreservation. Knowledge about oncofertility is also low amongst oncology providers in Mexico. One study found that, though providers are able to identify oncologic treatments associated with infertility, they rarely know the tests that need to be ordered to assess fertility. In addition, 50% of providers could not name a fertility preservation method, and only 10% reported self-perceived confidence in providing fertility preservation counseling. Physicians under 40 years of age were more likely to inform patients about fertility preservation and provide effective fertility counseling. Dr. Bourlon clarified the need for culturally appropriate educational tools, public funding mechanisms, and resource-stratified guidelines to increase access to oncofertility in Mexico. Dr. Bourlon was in the process of developing an oncofertility registry when the COVID-19 pandemic hit.
In Panama, only 7% of people have private insurance and most do not cover oncofertility treatment or tests. To fill this gap, Mario Vega Croker, MD, implemented Panama Fertility as a pro-bono oncofertility program, in which patients only pay facility fees (approx. $1000–1500). In addition, the referral rate to fertility centers from gynecologists in Panama is about 1%, compared to 50% in the US, and the rate among oncologists is even lower, which makes coordination of oncofertility care difficult. To change this medical mindset, Dr. Vega Crocker reached out to FUNAFES: the National Foundation for Fertility and Sterility, which brought credibility and communications outreach experience. Dr. Vega Crocker ultimately started his own foundation to create partnerships with cancer patients and medical societies, with the goal of increasing referrals of oncology patients to fertility centers. The foundation recently hosted a webinar series directed at oncologists and surgical oncologists to educate on the importance of timely referrals of patients to oncofertility care.
Within Latin America, Argentina has the highest ART usage rate per million inhabitants and was the first country to ensure fertility preservation procedures are covered by public and private healthcare. Romina I. Pesce, MD, MSC, described three key barriers faced by oncology patients seeking fertility preservation in Argentina. The first occurs at the initial consultation, where patients encounter a range of attitudes about fertility preservation. Some healthcare professionals avoid the discussion, while others report not having enough time to discuss options with patients. This leads to low referral rates as well as delays in connecting a patient with a specialist. Geographic and transportation issues are also often overlooked during the initial consultation. The second set of barriers includes limited time to decide whether to pursue fertility preservation and the long processing times for financial coverage. A patient with an aggressive cancer may not have time to make the decision to undergo fertility preservation before cancer treatment starts. Finally, several barriers prevent patients from returning after cancer treatment, including a lack of information about the success of fertility treatment and fear about pregnancy among survivors. Dr. Pesce stressed the need for interdisciplinary teamwork to quickly connect patients with specialists. Fertility preservation patient decision aids and patient navigators can help patients with decision-making or find insurance coverage. Improving follow-up and sharing data on the effectiveness and safety of procedures and processes, as well as keeping open communication with national and international networks, is important to raise awareness of oncofertility among physicians and patients. Patients need accurate information about outcomes and should be encouraged to return after undergoing a fertility preservation procedure.
Dana Kimelman, MD, MS-RSM, described the results of a survey to evaluate the knowledge, attitudes, and practice of fertility preservation treatments among healthcare professionals in Uruguay. All participants agreed that cancer treatment had gonadotoxic effects; however, only half of those surveyed knew about the types of fertility preservation options available to cancer patients. Although the majority of participants agreed that oncofertility should be considered part of the cancer treatment plan, the same number reported that they either sometimes, once in a while, or never showed concern about the reproductive effects of cancer treatments in young cancer patients. The survey further found that more than half of participants would sometimes or never refer a patient to an oncofertility specialist. As in many other countries, one of the biggest barriers for fertility preservation treatment in Uruguay cost. About 52% of participants did not know of any financial support for fertility preservation treatments. There is a need for greater awareness and education about oncofertility among healthcare professionals in Uruguay, as well as the establishment of a clear set of standard practices for patient selection, OTC, ovarian tissue handling, vitrification and storage, and autologous transplantation to improve patient care and oncofertility outcomes.
Chris Venter, MD, traced the footprint of the Oncofertility Consortium in South Africa. With 58 million people, 12 official languages, and 9 provinces, South Africa faced challenges in establishing a national Oncofertility Network, requiring a hard look at the resources at hand to provide standardized care, increase awareness of these services, provide a multidisciplinary approach to treatment plans, and increase funding. In 2018, an initial collaboration between Fertility Preservation and Medical Oncology in South Africa was established and the first Oncofertility session at the South African Society for Medical Oncology Conference was held the same year. Since then, 6 of 19 clinics accredited by the Southern African Society of Reproductive Medicine and Gynaecological Endoscopy (SASREG) have joined the Oncofertility Network in South Africa. While 85% of these clinics are private, there is a growing partnership between public and private clinics, with a commitment to provide standard fertility preservation services, from IRB-approved tissue preservation to standard IVF. Since the inception of the Oncofertility Network, there has been a dramatic increase in oncology patients seeking fertility preservation options, with the highest number in 2020. SASREG provides accreditation to clinics that maintain a high standard of care, and doctors are encouraged to take online courses to stay current on cryopreservation methods and standard clinical procedures. Funding remains the largest issue, with 85% of the population in South Africa utilizing public healthcare and unable to afford the out-of-pocket fees associated with oncofertility care. Future efforts are focused on funding to increase accessibility and awareness of fertility preservation services and promoting formal data acquisition to ensure standardization of care.
In 2017, Nonso Daniels helped establish an Oncofertility Network in Nigeria to provide infrastructure, awareness, and collaboration amongst practitioners. Nigeria has 205 million people, 15 oncology centers (only half of which are functional), and 92 fertility centers. Of the fertility centers in Nigeria, only 4 are located near oncology units. Currently, there is a wide gap in knowledge among oncology providers regarding fertility preservation options for patients with cancer. Oocyte retrieval and oocyte and embryo cryopreservation have been available, but ovarian tissue freezing and transplantation and fertoprotective approaches are not. Practitioners do not present options for fertility preservation due to financial and time constraints and fears about survivability. A lack of awareness in the general public underscores a critical need for advocacy, awareness, and sensitization programs. Research and education about fertility preservation has relied on the work of local organizations dedicated to supporting individual patients, but with more than 250 ethnic nationalities and diverse belief systems, advocacy efforts are challenging. Mr. Daniels continues to engage and potentially collaborate with charities, non-profits, and businesses to increase awareness, funding for treatment, and development of online educational tools.
Mohamed Khrouf, MD, discussed his experience building the Oncofertility Consortium in Africa. About half of countries in Africa have IVF clinics and 15 also provide oncology treatment. Cryopreservation is well developed in Africa, accounting for more than 75% of reported procedures since 2013. To overcome barriers to care, Dr. Khrouf is actively encouraging oncology and fertility practitioners to collaborate and form a robust oncofertility network in Africa. These barriers include a lack of awareness amongst practitioners, minimal referrals from oncologists, and overall lack of communication and collaboration in patient care. Since 2017, Dr. Khrouf has pursued a “door-to-door” strategy in Tunisia to visit oncology teams and build relationships, leading to a sharp increase in fertility preservation. Financial barriers remain an issue across Africa. Currently, fertility preservation drug therapies are covered in Morocco. In Tunisia, infertility medications are covered by National Insurance and there is a public hospital that provides fertility preservation options at an affordable cost. South Africa has plans to provide affordable fertility preservation options and Egypt remains a champion of providing services at lower costs, offering support for one cycle of IVF. Social and legal barriers limit third-party egg donation options in Tunisia, Senegal, Algeria, Egypt, and Morocco, but is allowed and potentially unregulated in Nigeria, South Africa, and the Ivory Coast. Practitioners are constantly overcoming social and legal hurdles to provide these services. In 2020, the African Federation of Fertility Societies was established, consisting of 20 Fertility Societies including the African Oncofertility Consortium.
India is home to a large and growing number of fertility centers; 97% are stand-alone or private ART facilities and only 2% are institution-based. The oncofertility score — a tool used to measure the availability and utilization of an oncofertility option for patients in a treating center, country, or group of countries — showed that these centers are similar to those in other parts of the world, but do not provide egg and embryo freezing for all cancer patients. In 2020, Satish Kumar Adiga, PhD, and colleagues surveyed Indian oncologists and gynecologists about their knowledge and attitudes towards fertility preservation and barriers to establishing oncofertility in India [143]. Oncologists were only slightly less aware and less knowledgeable about options for fertility preservation compared to gynecologists. Economic barriers were seen as largest the contributing factor to a lack of oncofertility care, with poor health insurance coverage for fertility services, lack of institutional funding, and high out-of-pocket costs for fertility treatment received at private centers. Dr. Adiga advocates for creation of fertility preservation consortiums nationally to facilitate networking, knowledge sharing, and resource distribution among medical professionals; the incorporation of oncofertility into the training of cancer and fertility healthcare providers; and development of fertility preservation societies in India.
Discussion and future directions
Although it was the first time we convened the field virtually, in an unconventional way, we convened the field, nonetheless. What we learned at this meeting was that this group of diverse professionals in fertility preservation and oncofertility, consistently and enthusiastically comes together on an annual basis with the common goal of advancing the field. One notable part of this meeting was how it engaged the next generation of leaders including early-career or junior level speakers as well as participants who self-identified as trainees. New research was presented at the meeting and many of the talks focused on new and improved ways to treat our patients around the globe. Transitional patient care and fundamental science came together to unify and direct the next generation of work in the field.
As a field, there are a variety of challenges we must overcome in the next decade to ensure progress continues even despite limited resources and other paucities. One area of universal struggle that has been documented in the literature is the lack of resources especially in third world and developing nations [14, 21, 144]. Another issue is the leaky pipeline of reproductive scientists and clinicians in academia. While this is not a challenge unique to our field, it is one that poses a prolonged threat. While we anticipate resource limitations, both in the financial and personnel sense, will continue to be obstacles foe the field, if we continue to convene as a field on a regular basis, at meetings like the Oncofertility Conference and others, we can continue to share best practices and templates for success, which can strengthen local, regional, and international ties and maximize interaction among centers to create synergistic opportunities for the field [21].
While the circumstances surrounding the COVID-19 pandemic forced us to convene virtually, one outstanding upside of this event was that it enhanced the accessibility. We learned a virtual environment allows us to open the doors wide to over 700 attendees, including many first-time attendees. We also learned that fundamental science is continuing despite the context of the COVID-19 pandemic. Conversations continue to happen between basic science and clinical science and there are large data sets that feed back to the bench to drive the next generation of new questions that will be asked. Around the globe, there is extraordinary value in coming together as it provides value and allows us to make the arguments to governments, philanthropists, and funders about the importance of fertility preservation for patients both in the oncologic and non-oncologic settings. This improved model for global accessibility will allow us to provide a route for advocacy, so we are recognized as an authentic area of medicine that is burgeoning around the globe.
Change history
03 August 2022
A Correction to this paper has been published: https://doi.org/10.1007/s10815-022-02586-x
References
Woodruff TK. Oncofertility: a grand collaboration between reproductive medicine and oncology. Reproduction. 2015;150(3):S1-10.
Armstrong GT, et al. Reduction in late mortality among 5-year survivors of childhood cancer. N Engl J Med. 2016;374(9):833–42.
Armstrong GT, Yasui Y, Robison LL. Reduction in late mortality after childhood cancer. N Engl J Med. 2016;375(3):290–2.
Weir HK, et al. The past, present, and future of cancer incidence in the United States: 1975 through 2020. Cancer. 2015;121(11):1827–37.
Cox CL, et al. Noncancer-related mortality risks in adult survivors of pediatric malignancies: the childhood cancer survivor study. J Cancer Surviv. 2014;8(3):460–71.
Anazodo A, et al. Oncofertility-An emerging discipline rather than a special consideration. Pediatr Blood Cancer. 2018;65(11):e27297.
Ataman LM, et al. Quantifying the growth of oncofertility. Biol Reprod. 2018;99(2):263–5.
Ataman LM, et al. Creating a global community of practice for oncofertility. J Glob Oncol. 2016;2(2):83–96.
De Vos M, Smitz J, Woodruff TK. Fertility preservation in women with cancer. Lancet. 2014;384(9950):1302–10.
Rashedi, A.S., et al., Survey of third-party parenting options associated with fertility preservation available to patients with cancer around the globe. JCO Glob Oncol, 2020. 6.
Rashedi, A.S., et al., Survey of fertility preservation options available to patients with cancer around the globe. JCO Glob Oncol, 2020. 6.
Salama, M., et al., Building oncofertility core competency in developing countries: experience from Egypt, Tunisia, Brazil, Peru, and Panama. JCO Glob Oncol, 2020. 6.
Salama M, et al. Installing oncofertility programs for common cancers in limited resource settings (Repro-Can-OPEN Study): an extrapolation during the global crisis of Coronavirus (COVID-19) pandemic. J Assist Reprod Genet. 2020;37(7):1567–77.
Salama, M., et al., Barriers and opportunities of oncofertility practice in nine developing countries and the emerging oncofertility professional engagement network. JCO Glob Oncol, 2020. 6.
Smith BM, et al. The National Physicians Cooperative: transforming fertility management in the cancer setting and beyond. Future Oncol. 2018;14(29):3059–72.
Waimey KE, et al. Future directions in oncofertility and fertility preservation: a report from the 2011 Oncofertility Consortium Conference. J Adolesc Young Adult Oncol. 2013;2(1):25–30.
Woodruff TK. The emergence of a new interdiscipline: oncofertility. Cancer Treat Res. 2007;138:3–11.
Woodruff TK. Preserving fertility during cancer treatment. Nat Med. 2009;15(10):1124–5.
Woodruff TK. The Oncofertility Consortium–addressing fertility in young people with cancer. Nat Rev Clin Oncol. 2010;7(8):466–75.
Woodruff TK. Reproductive endocrinology: fertility in female survivors of childhood cancer. Nat Rev Endocrinol. 2013;9(10):571–2.
Woodruff TK, et al. A view from the past into our collective future: the oncofertility consortium vision statement. J Assist Reprod Genet. 2021;38(1):3–15.
Moravek MB, et al. Development of a pediatric fertility preservation program: a report from the Pediatric Initiative Network of the Oncofertility Consortium. J Adolesc Health. 2019;64(5):563–73.
Kuang Y, et al. Luteal-phase ovarian stimulation is feasible for producing competent oocytes in women undergoing in vitro fertilization/intracytoplasmic sperm injection treatment, with optimal pregnancy outcomes in frozen-thawed embryo transfer cycles. Fertil Steril. 2014;101(1):105–11.
Chien AJ, et al. Fertility preservation with ovarian stimulation and time to treatment in women with stage II-III breast cancer receiving neoadjuvant therapy. Breast Cancer Res Treat. 2017;165(1):151–9.
Letourneau JM, et al. Random start ovarian stimulation for fertility preservation appears unlikely to delay initiation of neoadjuvant chemotherapy for breast cancer. Hum Reprod. 2017;32(10):2123–9.
Letourneau JM, et al. Fertility preservation before breast cancer treatment appears unlikely to affect disease-free survival at a median follow-up of 43 months after fertility-preservation consultation. Cancer. 2020;126(3):487–95.
Manuel SL, et al. Ovarian stimulation is a safe and effective fertility preservation option in the adolescent and young adult population. J Assist Reprod Genet. 2020;37(3):699–708.
Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112(6):1022–33.
Dolmans MM, et al. Transplantation of cryopreserved ovarian tissue in a series of 285 women: a review of five leading European centers. Fertil Steril. 2021;115(5):1102–15.
Donnez J, et al. Children born after autotransplantation of cryopreserved ovarian tissue a review of 13 live births. Ann Med. 2011;43(6):437–50.
Donnez J, Dolmans MM. Ovarian cortex transplantation: 60 reported live births brings the success and worldwide expansion of the technique towards routine clinical practice. J Assist Reprod Genet. 2015;32(8):1167–70.
Dolmans MM, Falcone T, Patrizio P. Importance of patient selection to analyze in vitro fertilization outcome with transplanted cryopreserved ovarian tissue. Fertil Steril. 2020;114(2):279–80.
Shapira M, et al. Evaluation of ovarian tissue transplantation: results from three clinical centers. Fertil Steril. 2020;114(2):388–97.
Kristensen SG, et al. Use of cryopreserved ovarian tissue in the Danish fertility preservation cohort. Fertil Steril. 2021;116(4):1098–106.
Dueholm Hjorth IM, et al. Reproductive outcomes after in vitro fertilization treatment in a cohort of Danish women transplanted with cryopreserved ovarian tissue. Fertil Steril. 2020;114(2):379–87.
Khattak, H., et al., Fresh and cryopreserved ovarian tissue transplantation for preserving reproductive and endocrine function: a systematic review and individual patient data meta-analysis. Hum Reprod Update, 2022.
Baird DT, et al. Long-term ovarian function in sheep after ovariectomy and transplantation of autografts stored at -196 C. Endocrinology. 1999;140(1):462–71.
Nisolle M, et al. Histologic and ultrastructural evaluation of fresh and frozen-thawed human ovarian xenografts in nude mice. Fertil Steril. 2000;74(1):122–9.
Manavella DD, et al. Two-step transplantation with adipose tissue-derived stem cells increases follicle survival by enhancing vascularization in xenografted frozen-thawed human ovarian tissue. Hum Reprod. 2018;33(6):1107–16.
Olesen HØ, et al. N-Acetylcysteine protects ovarian follicles from ischemia-reperfusion injury in xenotransplanted human ovarian tissue. Hum Reprod. 2020;36(2):429–43.
Halpern JA, Hill R, Brannigan RE. Guideline based approach to male fertility preservation. Urol Oncol. 2020;38(1):31–5.
Huang C, et al. Long-term cryostorage of semen in a human sperm bank does not affect clinical outcomes. Fertil Steril. 2019;112(4):663-669 e1.
Rowell EE, et al. Ovarian tissue health after laparoscopic unilateral oophorectomy: a porcine model for establishing optimized fertility preservation techniques in children. J Pediatr Surg. 2020;55(8):1631–8.
Corkum KS, Rowell E. Optimal technique for laparoscopic oophorectomy for ovarian tissue cryopreservation in pediatric girls. In: Woodruff TK, Shah DK, Vitek WS, editors. Textbook of oncofertility research and practice: a multidisciplinary approach. Cham: Springer International Publishing; 2019. p. 115–9.
Nahata L, et al. 2019 Pediatric Initiative Network: progress, proceedings, and plans. J Adolesc Young Adult Oncol. 2020;9(4):457–63.
Nahata L, et al. Ovarian tissue cryopreservation as standard of care: what does this mean for pediatric populations? J Assist Reprod Genet. 2020;37(6):1323–6.
Meacham LR, et al. Standardizing risk assessment for treatment-related gonadal insufficiency and infertility in childhood adolescent and young adult cancer: the Pediatric Initiative Network Risk Stratification System. J Adolesc Young Adult Oncol. 2020;9(6):662–6.
Schleedoorn MJ, et al. International consensus: ovarian tissue cryopreservation in young Turner syndrome patients: outcomes of an ethical Delphi study including 55 experts from 16 different countries. Hum Reprod. 2020;35(5):1061–72.
Oktay K, et al. Fertility preservation in women with Turner syndrome: a comprehensive review and practical guidelines. J Pediatr Adolesc Gynecol. 2016;29(5):409–16.
Abbott BP, et al. GW170817: observation of gravitational waves from a binary neutron star inspiral. Phys Rev Lett. 2017;119(16):161101.
Finlayson C, et al. Presence of germ cells in disorders of sex development: implications for fertility potential and preservation. J Urol. 2017;197(3 Pt 2):937–43.
Harris CJ, et al. Establishing an institutional gonadal tissue cryopreservation protocol for patients with differences of sex development. J Urol. 2020;204(5):1054–61.
Matoso A, et al. Spectrum of findings in orchiectomy specimens of persons undergoing gender confirmation surgery. Hum Pathol. 2018;76:91–9.
Schneider F, et al. Testicular functions and clinical characterization of patients with gender dysphoria (GD) undergoing sex reassignment surgery (SRS). J Sex Med. 2015;12(11):2190–200.
Kent MA, Winoker JS, Grotas AB. Effects of feminizing hormones on sperm production and malignant changes: microscopic examination of post orchiectomy specimens in transwomen. Urology. 2018;121:93–6.
Adeleye AJ, et al. Ovarian stimulation for fertility preservation or family building in a cohort of transgender men. J Assist Reprod Genet. 2019;36(10):2155–61.
Leung A, et al. Assisted reproductive technology outcomes in female-to-male transgender patients compared with cisgender patients: a new frontier in reproductive medicine. Fertil Steril. 2019;112(5):858–65.
Kinnear HM, et al. A mouse model to investigate the impact of testosterone therapy on reproduction in transgender men. Hum Reprod. 2019;34(10):2009–17.
Anderson RA, et al. The impact of cancer on subsequent chance of pregnancy: a population-based analysis. Hum Reprod. 2018;33(7):1281–90.
Chiarelli AM, Marrett LD, Darlington GA. Pregnancy outcomes in females after treatment for childhood cancer. Epidemiology. 2000;11(2):161–6.
Welsh LC, Taylor A. Impact of pelvic radiotherapy on the female genital tract and fertility preservation measures. World J Obstet Gynecol. 2014;3(2):45–53.
Chung K, et al. Emergency IVF versus ovarian tissue cryopreservation: decision making in fertility preservation for female cancer patients. Fertil Steril. 2013;99(6):1534–42.
Gougeon A. Regulation of ovarian follicular development in primates: facts and hypotheses. Endocr Rev. 1996;17(2):121–55.
Mahajan N. Fertility preservation in female cancer patients: an overview. J Hum Reprod Sci. 2015;8(1):3–13.
Meirow D, Schiff E. Appraisal of chemotherapy effects on reproductive outcome according to animal studies and clinical data. J Natl Cancer Inst Monogr. 2005;34:21–5.
European Society of Human Reproduction and Embryology. ESHRE Guideline Female Fertility Preservation. 2020 [cited 2021 May 16]; Available from: https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Female-fertility-preservation.
La Marca A, et al. Anti-Mullerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART). Hum Reprod Update. 2010;16(2):113–30.
Hagen CP, et al. Serum levels of anti-Mullerian hormone as a marker of ovarian function in 926 healthy females from birth to adulthood and in 172 Turner syndrome patients. J Clin Endocrinol Metab. 2010;95(11):5003–10.
Broer SL, et al. Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: an individual patient data approach. Hum Reprod Update. 2013;19(1):26–36.
Toner JP, Seifer DB. Why we may abandon basal follicle-stimulating hormone testing: a sea change in determining ovarian reserve using antimullerian hormone. Fertil Steril. 2013;99(7):1825–30.
Guzy L, Demeestere I. Assessment of ovarian reserve and fertility preservation strategies in children treated for cancer. Minerva Ginecol. 2017;69(1):57–67.
Choy JT, Brannigan RE. The determination of reproductive safety in men during and after cancer treatment. Fertil Steril. 2013;100(5):1187–91.
Loren AW, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31(19):2500–10.
Meirow D. Ovarian injury and modern options to preserve fertility in female cancer patients treated with high dose radio-chemotherapy for hemato-oncological neoplasias and other cancers. Leuk Lymphoma. 1999;33(1–2):65–76.
Gerstl B, et al. Feasibility, acceptability and appropriateness of a reproductive patient reported outcome measure for cancer survivors. PLoS ONE. 2021;16(8):e0256497.
Nguyen Q-N, et al. Loss of PUMA protects the ovarian reserve during DNA-damaging chemotherapy and preserves fertility. Cell Death Dis. 2018;9(6):618.
Stringer JM, et al. Oocytes can efficiently repair DNA double-strand breaks to restore genetic integrity and protect offspring health. Proc Natl Acad Sci U S A. 2020;117(21):11513–22.
Xiao S, et al. Size-specific follicle selection improves mouse oocyte reproductive outcomes. Reproduction. 2015;150(3):183–92.
Xiao S, et al. Doxorubicin has dose-dependent toxicity on mouse ovarian follicle development, hormone secretion, and oocyte maturation. Toxicol Sci. 2017;157(2):320–9.
Wang Y, et al. Multidrug resistance protein 1 deficiency promotes doxorubicin-induced ovarian toxicity in female mice. Toxicol Sci. 2018;163(1):279–92.
Winship AL, et al. The PARP inhibitor, olaparib, depletes the ovarian reserve in mice: implications for fertility preservation. Hum Reprod. 2020;35(8):1864–74.
Behringer K, et al. No protection of the ovarian follicle pool with the use of GnRH-analogues or oral contraceptives in young women treated with escalated BEACOPP for advanced-stage Hodgkin lymphoma. Final results of a phase II trial from the German Hodgkin Study Group. Ann Oncol. 2010;21(10):2052–60.
Falcone T, Moore HC. GnRH agonist for gonadal protection during chemotherapy. Hum Reprod. 2015;30(12):2711–2.
Lambertini M, et al. Ovarian protection with gonadotropin-releasing hormone agonists during chemotherapy in cancer patients: from biological evidence to clinical application. Cancer Treat Rev. 2019;72:65–77.
Spears N, et al. Ovarian damage from chemotherapy and current approaches to its protection. Hum Reprod Update. 2019;25(6):673–93.
Adhikari D, et al. Disruption of Tsc2 in oocytes leads to overactivation of the entire pool of primordial follicles. Mol Hum Reprod. 2009;15(12):765–70.
Reddy P, et al. Oocyte-specific deletion of Pten causes premature activation of the primordial follicle pool. Science. 2008;319(5863):611–3.
Zhang XM, et al. Rapamycin preserves the follicle pool reserve and prolongs the ovarian lifespan of female rats via modulating mTOR activation and sirtuin expression. Gene. 2013;523(1):82–7.
Guo Z, Yu Q. Role of mTOR signaling in female reproduction. Front Endocrinol (Lausanne). 2019;10:692.
Liu W, et al. The protective effects of rapamycin pretreatment on ovarian damage during ovarian tissue cryopreservation and transplantation. Biochem Biophys Res Commun. 2021;534:780–6.
Tanaka Y, et al. Protective effect of a mechanistic target of rapamycin inhibitor on an in vivo model ofcisplatin-induced ovarian gonadotoxicity. Exp Anim. 2018;67(4):493–500.
Goldman KN, et al. mTORC1/2 inhibition preserves ovarian function and fertility during genotoxic chemotherapy. Proc Natl Acad Sci U S A. 2017;114(12):3186–91.
Durlinger AL, et al. Control of primordial follicle recruitment by anti-Mullerian hormone in the mouse ovary. Endocrinology. 1999;140(12):5789–96.
Pepin D, et al. An albumin leader sequence coupled with a cleavage site modification enhances the yield of recombinant C-terminal Mullerian Inhibiting Substance. Technology. 2013;1(1):63–71.
Kano M, et al. AMH/MIS as a contraceptive that protects the ovarian reserve during chemotherapy. Proc Natl Acad Sci U S A. 2017;114(9):E1688–97.
Saatcioglu, H.D., et al., Single-cell sequencing of neonatal uterus reveals an Misr2+ endometrial progenitor indispensable for fertility. Elife, 2019. 8.
Zelinski MB, et al. Vitrified macaque ovarian cortical tissue transplanted to heterotopic sites produces fertilizable oocytes. Fertil Steril. 2018;110(4):E55–E55.
Lee DM, et al. Heterotopic transplants of vitrifiedovarian tissue in macaques: assessment of follicular function, embryonic development and a novel microbubble assay for blood flow. Fertil Steril. 2012;98(3):S69–S69.
Zhang H, et al. Urinary bladder matrix scaffolds improve endometrial regeneration in a rat model of intrauterine adhesions. Biomater Sci. 2020;8(3):988–96.
Laronda MM, et al. A bioprosthetic ovary created using 3D printed microporous scaffolds restores ovarian function in sterilized mice. Nat Commun. 2017;8:15261.
Laronda MM, et al. Initiation of puberty in mice following decellularized ovary transplant. Biomaterials. 2015;50:20–9.
Jakus, A.E., et al., "Tissue papers" from organ-specific decellularized extracellular matrices. Adv Funct Mater, 2017. 27(3).
Henning NF, et al. Proteomic analyses of decellularized porcine ovaries identified new matrisome proteins and spatial differences across and within ovarian compartments. Sci Rep. 2019;9(1):20001.
Henning, N.F.C., A.E. Jakus, and M.M. Laronda, Building organs using tissue-specific microenvironments: perspectives from a bioprosthetic ovary. Trends Biotechnol, 2021.
Ouni E, et al. Spatiotemporal changes in mechanical matrisome components of the human ovary from prepuberty to menopause. Hum Reprod. 2020;35(6):1391–410.
Edwards, R.G., Meiosis in Ovarian Oocytes of Adult Mammals. Nature, 1962. 196(4853): p. 446-+.
Edwards RG. Maturation in vitro of mouse sheep cow pig rhesus monkey and human ovarian oocytes. Nature. 1965;208(5008):349–0.
Peluffo MC, et al. Cumulus-oocyte complexes from small antral follicles during the early follicular phase of menstrual cycles in rhesus monkeys yield oocytes that reinitiate meiosis and fertilize in vitro. Biol Reprod. 2010;83(4):525–32.
Grynberg M, et al. First birth achieved after fertility preservation using vitrification of in vitro matured oocytes in a woman with breast cancer. Ann Oncol. 2020;31(4):541–2.
Grynberg M, et al. Similar in vitro maturation rates of oocytes retrieved during the follicular or luteal phase offer flexible options for urgent fertility preservation in breast cancer patients. Hum Reprod. 2016;31(3):623–9.
Sanchez F, et al. Biphasic in vitro maturation (CAPA-IVM) specifically improves the developmental capacity of oocytes from small antral follicles. J Assist Reprod Genet. 2019;36(10):2135–44.
Sanchez F, et al. An improved IVM method for cumulus-oocyte complexes from small follicles in polycystic ovary syndrome patients enhances oocyte competence and embryo yield. Hum Reprod. 2017;32(10):2056–68.
Vuong LN, et al. In-vitro maturation of oocytes versus conventional IVF in women with infertility and a high antral follicle count: a randomized non-inferiority controlled trial. Hum Reprod. 2020;35(11):2537–47.
Vuong LN, et al. Live births after oocyte in vitro maturation with a prematuration step in women with polycystic ovary syndrome. J Assist Reprod Genet. 2020;37(2):347–57.
Kirillova, A., et al., Improved maturation competence of ovarian tissue oocytes using a biphasic in vitro maturation system for patients with gynecological malignancy: a study on sibling oocytes. J Assist Reprod Genet, 2021.
Park MK, et al. PTEN self-regulates through USP11 via the PI3K-FOXO pathway to stabilize tumor suppression. Nat Commun. 2019;10(1):636.
Chen Y, et al. The factors and pathways regulating the activation of mammalian primordial follicles in vivo. Front Cell Dev Biol. 2020;8:575706.
Vo, K.C.T. and K. Kawamura, In vitro activation early follicles: from the basic science to the clinical perspectives. Int J Mol Sci, 2021. 22(7).
Kawamura K, et al. Hippo signaling disruption and Akt stimulation of ovarian follicles for infertility treatment. Proc Natl Acad Sci U S A. 2013;110(43):17474–9.
Hsueh AJ, et al. Intraovarian control of early folliculogenesis. Endocr Rev. 2015;36(1):1–24.
Kawamura K, Kawamura N, Hsueh AJ. Activation of dormant follicles: a new treatment for premature ovarian failure? Curr Opin Obstet Gynecol. 2016;28(3):217–22.
Tanaka Y, Hsueh AJ, Kawamura K. Surgical approaches of drug-free in vitro activation and laparoscopic ovarian incision to treat patients with ovarian infertility. Fertil Steril. 2020;114(6):1355–7.
Hsueh AJW, Kawamura K. Hippo signaling disruption and ovarian follicle activation in infertile patients. Fertil Steril. 2020;114(3):458–64.
Kawamura K, Ishizuka B, Hsueh AJW. Drug-free in-vitro activation of follicles for infertility treatment in poor ovarian response patients with decreased ovarian reserve. Reprod Biomed Online. 2020;40(2):245–53.
Ernst EH, et al. Dormancy and activation of human oocytes from primordial and primary follicles: molecular clues to oocyte regulation. Hum Reprod. 2017;32(8):1684–700.
Correia HHV, et al. Activation of goat primordial follicles in vitro: influence of alginate and ovarian tissue. Reprod Domest Anim. 2020;55(1):105–9.
Green DM, et al. Cumulative alkylating agent exposure and semen parameters in adult survivors of childhood cancer: a report from the St Jude Lifetime Cohort Study. Lancet Oncol. 2014;15(11):1215–23.
Green DM, et al. The cyclophosphamide equivalent dose as an approach for quantifying alkylating agent exposure: a report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer. 2014;61(1):53–67.
Tian En L, et al. Impacts of platinum-based chemotherapy on subsequent testicular function and fertility in boys with cancer. Hum Reprod Update. 2020;26(6):874–85.
Tharmalingam MD, et al. Cisplatin and carboplatin result in similar gonadotoxicity in immature human testis with implications for fertility preservation in childhood cancer. BMC Med. 2020;18(1):374.
Kilcoyne KR, Mitchell RT. Fertility preservation: testicular transplantation for fertility preservation: clinical potential and current challenges. Reproduction. 2019;158(5):F1–14.
Kanatsu-Shinohara M, et al. Restoration of fertility in infertile mice by transplantation of cryopreserved male germline stem cells. Hum Reprod. 2003;18(12):2660–7.
Hermann BP, et al. Spermatogonial stem cell transplantation into rhesus testes regenerates spermatogenesis producing functional sperm. Cell Stem Cell. 2012;11(5):715–26.
Honaramooz A, et al. Sperm from neonatal mammalian testes grafted in mice. Nature. 2002;418(6899):778–81.
Honaramooz A, et al. Accelerated maturation of primate testis by xenografting into mice. Biol Reprod. 2004;70(5):1500–3.
Liu Z, et al. Generation of macaques with sperm derived from juvenile monkey testicular xenografts. Cell Res. 2016;26(1):139–42.
Hermann BP, et al. Characterization, cryopreservation, and ablation of spermatogonial stem cells in adult rhesus macaques. Stem Cells. 2007;25(9):2330–8.
Fayomi AP, et al. Autologous grafting of cryopreserved prepubertal rhesus testis produces sperm and offspring. Science. 2019;363(6433):1314–9.
Hutka, M., et al., Exogenous gonadotrophin stimulation induces partial maturation of human Sertoli cells in a testicular xenotransplantation model for fertility preservation. J Clin Med, 2020. 9(1).
Hutka, M., et al., Fertility preservation in childhood cancer: endocrine activity in prepubertal human testis xenografts exposed to a pubertal hormone environment. Cancers (Basel), 2020. 12(10).
Nickkholgh B, et al. Genetic and epigenetic stability of human spermatogonial stem cells during long-term culture. Fertil Steril. 2014;102(6):1700-7 e1.
Wu X, et al. Fertile offspring derived from mouse spermatogonial stem cells cryopreserved for more than 14 years. Hum Reprod. 2012;27(5):1249–59.
Tholeti P, et al. Oncofertility: knowledge, attitudes, and barriers among Indian oncologists and gynecologists. J Adolesc Young Adult Oncol. 2021;10(1):71–7.
Salama M, et al. Building oncofertility core competency in developing countries: experience from Egypt, Tunisia, Brazil, Peru, and Panama. J Glob Oncol. 2018;4:1–11.
Acknowledgements
We would like to thank all the speakers who delivered talks at this event. All those listed as authors reviewed and approved the content of their presentations. We would also like to thank Stacey Tobin for her editorial assistance and help preparing this manuscript. We would also like to acknowledge the Oncofertility Consortium for its continued commitment to hosting this annual meeting.
Funding
This work was funded through the Northwestern University Center for Reproductive Science and by a conference grant from the NIH/NICHD (R13HD063248).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Summary Sentence
This paper is a synopsis of the 2021 Oncofertility Around the Globe virtual conference and highlights the advances and frontiers in oncofertility and fertility preservation.
The correct given name of the 13th Author is S.K. instead of S.L.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ataman, L.M., Laronda, M.M., Gowett, M. et al. A synopsis of global frontiers in fertility preservation. J Assist Reprod Genet 39, 1693–1712 (2022). https://doi.org/10.1007/s10815-022-02570-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02570-5