Abstract
Background
In Western countries, the incidence of acute diverticulitis (AD) is increasing. Patients with uncomplicated diverticulitis can undergo a standard antibiotic treatment in an outpatient setting. The aim of this systematic review was to assess the safety and efficacy of the management of acute diverticulitis in an outpatient setting.
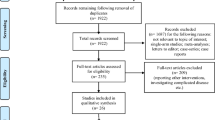
Methods
A literature search was performed on PubMed, Scopus, Embase, Central and Web of Science up to September 2018. Studies including patients who had outpatient management of uncomplicated acute diverticulitis were considered. We manually checked the reference lists of all included studies to identify any additional studies. Primary outcome was the overall failure rates in the outpatient setting. The failure of outpatient setting was defined as any emergency hospital admission in patients who had outpatient treatment for AD in the previous 60 days. A subgroup analysis of failure was performed in patients with AD of the left colon, with or without comorbidities, with previous episodes of AD, in patients with diabetes, with different severity of AD (pericolic air and abdominal abscess), with or without antibiotic treatment, with ambulatory versus home care unit follow-up, with or without protocol and where outpatient management is a common practice. The secondary outcome was the rate of emergency surgical treatment or percutaneous drainage in patients who failed outpatient treatment.
Results
This systematic review included 21 studies including 1781 patients who had outpatient management of AD including 11 prospective, 9 retrospective and only 1 randomized trial. The meta-analysis showed that outpatient management is safe, and the overall failure rate in an outpatient setting was 4.3% (95% CI 2.6%-6.3%). Localization of diverticulitis is not a selection criterion for an outpatient strategy (p 0.512). The other subgroup analyses did not report any factors that influence the rate of failure: previous episodes of acute diverticulitis (p = 0.163), comorbidities (p = 0.187), pericolic air (p = 0.653), intra-abdominal abscess (p = 0.326), treatment according to a registered protocol (p = 0.078), type of follow-up (p = 0.700), type of antibiotic treatment (p = 0.647) or diabetes (p = 0.610). In patients who failed outpatient treatment, the majority had prolonged antibiotic therapy and only few had percutaneous drainage for an abscess (0.13%) or surgical intervention for perforation (0.06%). These results should be interpreted with some caution because of the low quality of available data.
Conclusions
The outpatient management of AD can reduce the rate of emergency hospitalizations. This setting is already part of the common clinical practice of many emergency departments, in which a standardized protocol is followed. The data reported suggest that this management is safe if associated with an accurate selection of patients (40%); but no subgroup analysis demonstrated significant differences between groups (such as comorbidities, previous episode, diabetes). The main limitations of the findings of the present review concern their applicability in common clinical practice as it was impossible to identify strict criteria of failure.




Similar content being viewed by others
References
Dixon MR, Trudel JL (2004) Diverticular disease of the colon. In: Cameron JL (ed) Current surgical therapy, 9th edn. Elsevier, Philadelphia, pp 166–170
Brook MA, Victorino GP (2018) Diverticular disease of the colon. In: Harken AH, Moore E (eds) Abernathy’s surgical, 7th edn. Elsevier, Philadelphia, pp 224–226
Wu JS, Einstein DM (2004) Diagnosis and medical management of acute colonic diverticulitis. In: Fazio V, Church JM, Delaney CP Current therapy in colon and rectal surgery, 2nd edn. Elsevier, Philadelphia, pp 277–284
Nystrom PO (2010) Acute diverticulitis. In: Schein M, Rogers PN, Assalia A (eds) Schein’s common sense emergency abdominal surgery. Springer, Berlin, pp 277–287
Reddy VB, Longo WE (2013) The burden of diverticular disease on patients and healthcare systems. Gastroenterol Hepatol 9:21–27
Shaheen NJ, Hansen RA, Morgan DR, Gangarosa LM, Ringel Y, Thiny MT, Russo MW, Sandler RS (2006) The burden of gastrointestinal and liver diseases. Am J Gastroenterol 101:2128–2138
Sandler RS, Everhart JE, Donowitz M, Adams E, Cronin K, Goodman C, Gemmen E, Shah S, Avdic A, Rubin R (2002) The burden of selected digestive diseases in the United States. Gastroenterology 122:1500–1511
O’Connor ES, Smith MA, Heise CP (2012) Outpatient diverticulitis: mild or myth? J Gastrointest Surg 16:1389–1396
Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, Rafferty JF (2014) Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 57:284–294
Sartelli M, Catena F, Ansaloni L, Coccolini F et al (2016) WSES Guidelines for the management of acute left sided colonic diverticulitis in the emergency setting. World J Emerg Surg 29:11–37
Binda GA, Cuomo R, Laghi A, Nascimbeni R, Serventi A, Bellini D, Gervaz P, Annibale B, Italian Society of Colon and Rectal Surgery (2015) Practice parameters for the treatment of colonic diverticular disease: Italian Society of Colon and Rectal Surgery (SICCR) guidelines. Tech Coloproctol 19:615–626
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Mizuki A, Nagata H, Tatemichi M, Kaneda S, Tsukada N, Ishii H, Hibi T (2005) The out-patient management of patients with acute mild-to-moderate colonic diverticulitis. Aliment Pharmacol Ther 21:889–897
Alonso S, Pera M, Parés D, Pascual M, Gil MJ, Courtier R, Grande L (2010) Outpatient treatment of patients with uncomplicated acute diverticulitis. Colorectal Dis 12(10 Online):e278–e282
Isacson D, Thorisson A, Andreasson K, Nikberg M, Smedh K, Chabok A (2015) Outpatient, non-antibiotic management in acute uncomplicated diverticulitis: a prospective study. Int J Colorectal Dis 30:1229–1234
Mali JP, Mentula PJ, Leppäniemi AK, Sallinen VJ (2016) Symptomatic treatment for uncomplicated acute diverticulitis: a prospective cohort study. Dis Colon Rectum 59:529–534
Joliat GR, Emery J, Demartines N, Hübner M, Yersin B, Hahnloser D (2017) Antibiotic treatment for uncomplicated and mild complicated diverticulitis: outpatient treatment for everyone. Int J Colorectal Dis 32:1313–1319
Sirany AE, Gaertner WB, Madoff RD, Kwaan MR (2017) Diverticulitis diagnosed in the emergency room: is it safe to discharge home? J Am Coll Surg 225:21–25
Isacson D, Andreasson K, Nikberg M, Smedh K, Chabok A (2018) Outpatient management of acute uncomplicated diverticulitis results in health-care cost savings. Scand J Gastroenterol 53:449–452
Etzioni DA, Chiu VY, Cannom RR, Burchette RJ, Haigh PI, Abbas MA (2010) Outpatient treatment of acute diverticulitis: rates and predictors of failure. Dis Colon Rectum 53:861–865
Al-Sahaf O, Al-Azawi D, Fauzi MZ, El-Masry S, Gillen P (2008) Early discharge policy of patients with acute colonic diverticulitis following initial CT scan. Int J Colorectal Dis 23:817–820
Ünlü Ç, Gunadi PM, Gerhards MF, Boermeester MA, Vrouenraets BC (2013) Outpatient treatment for acute uncomplicated diverticulitis. Eur J Gastroenterol Hepatol 25:1038–1043
Biondo S, Golda T, Kreisler E, Espin E, Vallribera F, Oteiza F, Codina-Cazador A, Pujadas M, Flor B (2014) Outpatient versus hospitalization management for uncomplicated diverticulitis: a prospective, multicenter randomized clinical trial (DIVER Trial). Ann Surg 259:38–44
Hunter JP, Saratzis A, Sutton AJ, Boucher RH, Sayers RD, Bown MJ (2014) In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol 67:897–903
Ioannidis JPA, Trikalinos TA (2007) The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ Can Med Assoc J 176:1091–1096
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration, London
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y, Norris SL, Williams JW Jr, Atkins D, Meerpohl J, Schünemann HJ (2011) GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). J Clin Epidemiol 64:407–415
Zafer M, Horvath H, Mmeje O, van der Poel S, Semprini AE, Rutherford G, Brown J (2016) Effectiveness of semen washing to prevent human immunodeficiency virus (HIV) transmission and assist pregnancy in HIV-discordant couples: a systematic review and meta-analysis. Fertil Steril 105:645–655
Chan DKH, Tan KK (2018) Asian patients with Hinchey Ia acute diverticulitis: a condition for the ambulatory setting? Int J Colorectal Dis 33:61–64
Reynolds IS, O’Connell E, Heaney RM, Khan W, Khan IZ, Waldron R, Barry K (2018) Adherence to clinical guidelines and the potential economic benefits of admission avoidance for acute uncomplicated diverticulitis. Ir J Med Sci 187:59–64
Yoo T, Yang KH, Kim J, Park I, Cho H, Gwak G, Bae BN, Kim KH (2018) Predictive factors affecting the clinical course of patients with diverticulitis: who needs hospital management? Ann Coloproctol 34:23–28
Jaung R, Kularatna M, Robertson JP, Vather R, Rowbotham D, MacCormick AD, Bissett IP (2017) Uncomplicated acute diverticulitis: identifying risk factors for severe outcomes. World J Surg 41:2258–2265
Peláez N, Pera M, Courtier R, Sánchez J, Gil MJ, Parés D, Grandea L (2006) Applicability, safety and efficacy of an ambulatory treatment protocol in patients with uncomplicated acute diverticulitis. Cir Esp 80:369–372
Martín Gil J, Serralta De Colsa D, García Marín A, Vaquero Rodríguez A, Rey Valcárcel C, Pérez Díaz MD, Sanz Sánchez M, Turégano Fuentes F (2009) Safety and efficiency of ambulatory treatment of acute diverticulitis. Gastroenterol Hepatol 32:83–87
Rodríguez-Cerrillo M, Poza-Montoro A, Fernandez-Diaz E, Romero AI (2010) Patients with uncomplicated diverticulitis and comorbidity can be treated at home. Eur J Intern Med 21:553–554
Park HC, Kim BS, Lee BH (2011) Management of right colonic uncomplicated diverticulitis: outpatient versus inpatient management. World J Surg 35:1118–1122
Latuwak N (2012) Acute diverticulitis: a small retrospective study leaving many questions unanswered. Am J Clin Med 9:138–143
Rueda JC, Jimenez A, Caro A, Feliu F, Escuder J, Gris F, Spuch J, Vicente V (2012) Home treatment of uncomplicated acute diverticulitis. Int Surg 97:203–209
Moya P, Arroyo A, Pérez-Legaz J, Serrano P, Candela F, Soriano-Irigaray L, Calpena R (2012) Applicability, safety and efficiency of outpatient treatment in uncomplicated diverticulitis. Tech Coloproctol 16:301–307
Rodríguez-Cerrillo M, Poza-Montoro A, Fernandez-Diaz E, Matesanz-David M, Iñurrieta Romero A (2013) Treatment of elderly patients with uncomplicated diverticulitis, even with comorbidity, at home. Eur J Intern Med 24(5):430–432
Lorente L, Cots F, Alonso S, Pascual M, Salvans S, Courtier R, Gil MJ, Grande L, Pera M (2013) Outpatient treatment of uncomplicated acute diverticulitis: Impact on healthcare costs. Cir Esp 91:504–509
Mora Lopez L, Serra Pla S, Serra-Aracil X, Ballesteros E, Navarro S (2013) Application of a modified Neff classification to patients with uncomplicated diverticulitis. Colorectal Dis 15:1442–1447
Estrada Ferrer O, Ruiz Edo N, Hidalgo Grau LA, Abadal Prades M, Del Bas Rubia M, Garcia Torralbo EM, Heredia Budo A, Suñol Sala X (2016) Selective non-antibiotic treatment in sigmoid diverticulitis: is it time to change the traditional approach? Tech Coloproctol 20:309–315
Moya P, Bellon M, Arroyo A, Galindo I, Candela F, Lacueva J, Calpena R (2016) Outpatient treatment in uncomplicated acute diverticulitis: 5-year experience. Turk J Gastroenterol 27(4):330–335
Ribas Y, D’Hoore A (2016) Pushing the boundaries of the management of uncomplicated diverticulitis. Tech Coloproctol 20:269–270
Tursi A (2014) Efficacy, safety, and applicability of outpatient treatment for diverticulitis. Drug Health Patient Saf 6:29–36
O’Leary DP, Lynch N, Clancy C, Winter DC, Myers E (2015) International, expert-based, consensus statement regarding the management of acute diverticulitis. JAMA Surg 150:899–904
Kaiser AM, Jiang JK, Lake JP et al (2005) The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol 100:910–917
Kaewlai R, Nazinitsky KJ (2007) Acute colonic diverticulitis in a community-based hospital: CT evaluation in 138 patients. Emerg Radiol 13:171–179
Paolillo C, Spallino I (2015) Is it safe to send home an uncomplicated diverticulitis? The DIVER trial. Intern Emerg Med 10:193–194
Unlü C, de Korte N, Daniels L et al (2010) Dutch Diverticular Disease 3D Collaborative Study Group. A multicenter randomized clinical trial investigating the cost-effectiveness of treatment strategies with or without antibiotics for uncomplicated acute diverticulitis (DIABOLO trial). BMC Surg 20:10–23
Daniels L, Ünlü Ç, de Korte N, van Dieren S, Stockmann HB, Vrouenraets BC, Consten EC, van der Hoeven JA, Eijsbouts QA, Faneyte IF, Bemelman WA, Dijkgraaf MG, Boermeester MA, Dutch Diverticular Disease (3D) Collaborative Study Group (2017) Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis. Br J Surg 104:52–61
Chabok A, Påhlman L, Hjern F, Haapaniemi S, Smedh K, AVOD Study Group (2012) Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg 99:532–539
De Korte N, Kuyvenhoven JP, van der Peet DL, Felt-Bersma RJ, Cuesta MA, Stockmann HB (2012) Mild colonic diverticulitis can be treated without antibiotics. A case–control study. Colorectal Dis 14:325–330
Ridgway PF, Latif A, Shabbir J, Ofriokuma F, Hurley MJ, Evoy D, O’Mahony JB, Mealy K (2009) Randomized controlled trial of oral vs intravenous therapy for the clinically diagnosed acute uncomplicated diverticulitis. Colorectal Dis 11:941–946
Shabanzadeh DM, Wille-Jørgensen P (2012) Antibiotics for uncomplicated diverticulitis. Cochrane Database Syst Rev 14;11:CD009092
Van Dijk ST, Bos K, de Boer MGJ, Draaisma WA, van Enst WA, Felt RJF, Klarenbeek BR, Otte JA, Puylaert JBCM, van Geloven AAW, Boermeester MA (2018) A systematic review and meta-analysis of outpatient treatment for acute diverticulitis. Int J Colorectal Dis 33:505–512
Balasubramanian I, Fleming C, Mohan HM, Schmidt K, Haglind E, Winter DC (2017) Out-patient management of mild or uncomplicated diverticulitis: a systematic review. Dig Surg 34:151–160
Jackson JD, Hammond T (2014) Systematic review: outpatient management of acute uncomplicated diverticulitis. Int J Colorectal Dis 29:775–781
Kohn LT, Corrigan JM, Donaldson MS (2000) To err is human: building a safer health system. Institute of Medicine, Committee on Quality of Health Care in America, National Academy Press, Washington
Robinson KJ, Nouhan PP (2018) Expert Witness. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK436001/. Accessed 20 Jul 2018
Huscher C, Mingoli A, Mereu A, Sgarzini G (2013) Single-access laparoscopic “lavage” for purulent diverticulitis in a 96-year-old patient: how to reduce surgical trauma and standardize surgical technique. Surg Innov 20:109–112
Melsen WG, Bootsma MC, Rovers MM, Bonten MJ (2014) The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin Microbiol Infect 20:123–129
Acknowledgements
The authors thank Nereo Vettoretto and Vito D’Andrea for their assistance.
Funding
This study did not benefit of any source of funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study a formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cirocchi, R., Randolph, J.J., Binda, G.A. et al. Is the outpatient management of acute diverticulitis safe and effective? A systematic review and meta-analysis. Tech Coloproctol 23, 87–100 (2019). https://doi.org/10.1007/s10151-018-1919-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-018-1919-6