Abstract
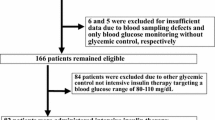
Perioperative hyperglycemia, hypoglycemia, and high glycemic variability are independent risk factors for mortality in critically ill patients. After cardiac surgery, intensive glycemic control without hypoglycemia may help to reduce the number of adverse events; however, postoperative glycemic control is difficult in many cases. In this study, we investigated whether the bedside artificial pancreas STG-55 is useful for postoperative glycemic control in cardiac surgery. Methods: In the present single-center retrospective study, we analyzed arterial blood glucose levels for 15 h after surgery in 69 patients treated using the bedside artificial pancreas and in 160 patients treated with continuous intravenous insulin infusion using a scale that adjusts for current blood glucose level, glycemic fluctuation, and insulin dose. Results: Hypoglycemia (arterial blood glucose level < 70 mg/dL) was not observed in any case. Patients in the group treated using the bedside artificial pancreas showed lower mean, maximum, and minimum blood glucose levels and glycemic variability and shorter treatment duration in the intensive care unit than patients treated with continuous intravenous insulin infusion. Notably, these results were not affected by diabetes status or differences in operative procedures. Analysis of patients undergoing isolated coronary artery bypass grafting surgery revealed that the incidence of surgical site complications composite with infection and dehiscence was lower. Conclusions: In cardiac surgery, postoperative treatment using bedside artificial pancreas is a novel therapy that improves hyperglycemia and glycemic variability, without hypoglycemia, and is, therefore, an attractive strategy for future surgeries.



Similar content being viewed by others
References
Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003;78:1471–8.
Farrokhi F, Smiley D, Umpierrez GE. Glycemic control in non-diabetic critically ill patients. Best Pract Res Clin Endocrinol Metab. 2011;25:813–24.
Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D. Importance of perioperative glycemic control in general surgery: a report from the surgical care and outcomes assessment program. Ann Surg. 2013;257:8–14.
Kotagal M, Symons RG, Hirsch IB, Umpierrez GE, Dellinger EP, Farrokhi ET, Flum DR. Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg. 2015;261:97–103.
Van Den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–67.
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39.
Preiser JC, Devos P, Ruiz-Santana S, Mélot C, Annane D, Groeneveld J, Iapichino G, Leverve X, Nitenberg G, Singer P, Wernerman J. A prospective randomised multi–centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the glucontrol study. Intensive Care Med. 2009;35:1738–48.
NICE-SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283–97.
NICE-SUGAR Study Investigators. Hypoglycemia and risk of death in critically ill patients. N Engl J Med. 2012;367:1108–18.
American Diabetes Association. Diabetes care in the hospital: standards of medical care in diabetes-2020. Diabetes Care. 2020;43:193–202.
Ban KA, Minei JP, Laronga C, Harbrecht BG, Jensen EH, Fry DE, Itani KM, Dellinger EP, Ko CY, Duane TM. American college of surgeons and surgical infection society: surgical site infection guidelines, 2016 update. J Am Coll Surg. 2017;224:59–74.
Kawahito S, Kitahata H, Kitagawa T, Oshita S. Intensive insulin therapy during cardiovascular surgery. J Med Invest. 2010;57:191–204.
Tsukamoto Y, Kinoshita Y, Kitagawa H, Munekage M, Munekage E, Takezaki Y, Yatabe T, Yamashita K, Yamazaki R, Okabayashi T, Tarumi M. Evaluation of a novel artificial pancreas: closed loop glycemic control system with continuous blood glucose monitoring. Artif Organs. 2013;37:67–73.
Kawamori R, Shichiri M, Goriya Y, Yamasaki Y, Shigeta Y, Abe H. Importance of insulin secretion based on the rate of change in blood glucose concentration in glucose tolerance, assessed by the artificial beta cell. Acta Endocrinol. 1978;87:339–51.
Okabayashi T, Nishimori I, Maeda H, Yamashita K, Yatabe T, Hanazaki K. Effect of intensive insulin therapy using a closed-loop glycemic control system in hepatic resection patients: a prospective randomized clinical trial. Diabetes Care. 2009;32:1425–7.
Okabayashi T, Nishimori I, Yamashita K, Sugimoto T, Maeda H, Yatabe T, Kohsaki T, Kobayashi M, Hanazaki K. Continuous postoperative blood glucose monitoring and control by artificial pancreas in patients having pancreatic resection: a prospective randomized clinical trial. Arch Surg. 2009;144:933–7.
Stahle E, Tammelin A, Bergstrom R, Hambreus A, Nystrom SO, Hansson HE. Sternal wound complications-incidence, microbiology and risk factors. Eur J Cardiothorac Surg. 1997;11:1146–53.
van den Boom W, Schroeder RA, Manning MW, Setji TL, Fiestan GO, Dunson DB. Effect of A1C and glucose on postoperative mortality in noncardiac and cardiac surgeries. Diabetes Care. 2018;41:782–8.
Knapik P, Nadziakiewicz P, Urbanska E, Saucha W, Herdynska M, Zembala M. Cardiopulmonary bypass increases postoperative glycemia and insulin consumption after coronary surgery. Ann Thorac Surg. 2009;87:1859–65.
Kawahito K, Sato H, Kadosaki M, Egawa A, Misawa Y. Spike in glucose levels after reperfusion during aortic surgery: assessment by continuous blood glucose monitoring using artificial endocrine pancreas. Gen Thorac Cardiovasc Surg. 2018;66:150–4.
McAlister FA, Man J, Bistritz L, Amad H, Tandon P. Diabetes and coronary artery bypass surgery: an examination of perioperative glycemic control and outcomes. Diabetes Care. 2003;26:1518–24.
Umpierrez G, Cardona S, Pasquel F, Jacobs S, Peng L, Unigwe M, Newton CA, Smiley-Byrd D, Vellanki P, Halkos M, Puskas JD. Randomized controlled trial of intensive versus conservative glucose control in patients undergoing coronary artery bypass graft surgery: GLUCO-CABG Trial. Diabetes Care. 2015;38:1665–72.
Mackenzie IMJ, Whitehouse T, Nightingale PG. The metrics of glycaemic control in critical care. Intensive Care Med. 2011;37:435–43.
Scott MJ, Miller TE. Pathophysiology of major surgery and the role of enhanced recovery pathways and the anesthesiologist to improve outcomes. Anesthesiol Clin. 2015;33:79–91.
Engelman DT, Ali WB, Williams JB, Perrault LP, Reddy VS, Arora RC, Roselli EE, Khoynezhad A, Gerdisch M, Levy JH, Lobdell K. Guidelines for perioperative care in cardiac surgery: enhanced recovery after surgery society recommendations. JAMA Surg. 2019;154:755–66.
Li M, Zhang J, Gan TJ, Qin G, Wang L, Zhu M, Zhang Z, Pan Y, Ye Z, Zhang F, Chen X. Enhanced recovery after surgery pathway for patients undergoing cardiac surgery: a randomized clinical trial. Eur J Cardiothorac Surg. 2018;54:491–7.
Trivedi V, Bleeker H, Kantor N, Visintini S, McIsaac DI, McDonald B. Survival, quality of life, and functional status following prolonged ICU stay in cardiac surgical patients: a systematic review. Crit Care Med. 2019;47:52–63.
Hanazaki K, Kitagawa H, Yatabe T, Munekage M, Dabanaka K, Takezaki Y, Tsukamoto Y, Asano T, Kinoshita Y, Namikawa T. Perioperative intensive insulin therapy using an artificial endocrine pancreas with closed-loop glycemic control system: the effects of no hypoglycemia. Am J Surg. 2014;207:935–41.
Mibu K, Yatabe T, Hanazaki K. Blood glucose control using an artificial pancreas reduces the workload of ICU Nurses. J Artif Organs. 2012;15:71–6.
Nygren JO, Thorell A, Soop M, Efendic S, Brismar K, Karpe F, Nair KS, Ljungqvist O. Perioperative insulin and glucose infusion maintains normal insulin sensitivity after surgery. Am J Physiol. 1998;275:140–8.
Hatzakorzian R, Shum-Tim D, Wykes L, Hülshoff A, Bui H, Nitschmann E, Lattermann R, Schricker T. Glucose and insulin administration while maintaining normoglycemia inhibits whole body protein breakdown and synthesis after cardiac surgery. J Appl Physiol. 2014;117:1380–7.
Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997;14:29–34.
Visser L, Zuurbier CJ, Hoek FJ, Opmeer BC, De Jonge E, De Mol BA, Van Wezel HB. Glucose, insulin and potassium applied as perioperative hyperinsulinaemic normoglycaemic clamp: effects on inflammatory response during coronary artery surgery. Br J Anaesth. 2005;95:448–57.
Akabori H, Tani M, Kitamura N, Maehira H, Imashuku Y, Tsujita Y, Shimizu T, Kitagawa H, Eguchi Y. Perioperative tight glycemic control using artificial pancreas decreases infectious complications via suppression of inflammatory cytokines in patients who underwent pancreaticoduodenectomy: a prospective, non-randomized clinical trial. Am J Surg. 2020;220:365–71.
Acknowledgements
This study has received no specific grants from funding agencies.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shin, U., Naoko, H., Michinori, T. et al. Utility of bedside artificial pancreas for postoperative glycemic control in cardiac surgery. J Artif Organs 24, 225–233 (2021). https://doi.org/10.1007/s10047-020-01223-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-020-01223-7