Abstract
Introduction
The aim of this study was to demonstrate the safety and the efficacy of the self-gripping Parietex ProGrip™ mesh (Sofradim Production, Trévoux, France) used with the laparoscopic approach for inguinal hernia repair. The incidence of chronic pain, post-operative complications, patient satisfaction and hernia recurrence at follow-up after 12 months was evaluated.
Methods
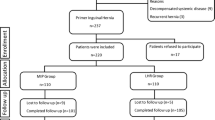
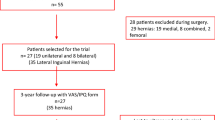
Data were collected retrospectively from patient files and were analyzed for 169 male and female patients with 220 primary inguinal hernias. All patients included had undergone surgical repair for inguinal hernia by the laparoscopic transabdominal preperitoneal approach using Parietex ProGrip™ meshes performed in the same clinical center in Germany. Pre-, per- and post-operative data were collected, and a follow-up after 12 months was performed prospectively. Complications, pain scored on a 0–10 numeric rating scale (NRS), patient satisfaction and hernia recurrence were assessed.
Results
The only complications were minor and were post-operative: hematoma/seroma (3 cases), secondary hemorrhage through the trocar’s site (2 cases), hematuria, emphysema in the inguinal regions (both sides) and swelling above the genital organs (1 case for each). At mean follow-up at 22.8 months, there were only 3 reports of hernia recurrence: 1.4 % of the hernias. Most patients (95.9 %) were satisfied or very satisfied with their hernia repair with only 1.2 % reporting severe pain (NRS score 7–10) and 3.6 % reported mild pain.
Conclusion
This study demonstrates that in experienced hands, inguinal hernia repair surgery performed by laparoscopic transabdominal preperitoneal hernioplasty using Parietex ProGrip™ self-gripping meshes is rapid, efficient and safe with low pain and low hernia recurrence rate.




Similar content being viewed by others
References
The EU Hernia Trialists Collaboration (2002) Repair of groin hernia with synthetic mesh. Ann Surg 235(3):322–332
Bittner R, Scwartz J (2011) Inguinal hernia repair: current surgical techniques. Lang Arch Surg 397(2):271–282
Simons MP et al (2009) European hernia society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362(9395):1561–1571
Amid P, Shulman A, Lichtenstein I (1994) A critical evaluation of the Lichtenstein tension-free hernioplasty. Int Surg 79(1):76–79
Schmedt C, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19:188–199
Neumayer L et al (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Memon MA et al (2003) Meta—analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 90(12):1479–1492
Bittner R et al (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25:2773–2843
Teng Y et al (2011) A meta-analysis of randomized controlled trials of fixation versus nonfixation of mesh in laparoscopic total extraperitoneal inguinal hernia repair. Surg Endosc 26:249–254
Canonico S et al (2005) Mesh fixation with human fibrin glue (Tissucol) in open tension-free inguinal hernia repair: a preliminary report. Hernia 9(4):330–333
Canziani M et al (2009) Sutureless mesh fibrin glue incisional hernia repair. Hernia 13(6):625–629
Tam K, Liang H, Chai C (2010) Outcomes of staple fixation of mesh versus nonfixation in laparoscopic total extraperitoneal inguinal repair: a meta-analysis of randomized controlled trials. World J Surg 34(12):3065–3074
Taylor C et al (2008) Laparoscopic inguinal hernia repair without mesh fixation, early results of a large randomised clinical trial. Surg Endosc 22(3):757–762
Topart P, Vandenbroucke F, Lozac’h P (2005) Tisseel versus tack staples as mesh fixation in totally extraperitoneal laparoscopic repair of groin hernias. Surg Endosc 19(5):724–727
Kapiris S et al (2009) Laparoscopic transabdominal preperitoneal hernia repair (TAPP): stapling the mesh is not mandatory. J Laparoendosc Adv Surg Tech 19(3):419–422
Katkhouda N (2004) A new technique for laparoscopic hernia repair using fibrin sealant. Surg Technol Int 12:120–126
Chastan P (2009) Tension-free open hernia repair using an innovative self-gripping semi-resorbable mesh. Hernia 13(2):137–142
Kingsnorth A et al (2012) Randomized controlled multicenter international clinical trial of self-gripping Parietex™ ProGrip™ polyester mesh versus lightweight polypropylene mesh in open inguinal hernia repair: interim results at 3 months. Hernia 16(3):287–294
Kapischke M, Schulze H, Caliebe A (2010) Self-fixating mesh for the Lichtenstein procedure—a prestudy. Langenbecks Arch Surg 395(4):317–322
Justinger C, Mikneviciute J, Schuld J, Schilling M (2011) Effective operative training in hernia repair for junior surgery residents. Eur Surg Acta Chir Austr 43(1):45–48
Eklund A et al (2009) Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair. A randomized, multicenter trial with 5-year follow-up. Ann Surg 249(1):33–38
Aasvang EK et al (2010) Predictive risk factors for persistent postherniotomy pain. Anesthesiology 112:957–969
Eklund A et al (2010) Long term cost minimalization analysis comparing laparoscopic with open (Lichtenstein) inguinal repair. Br J Surg 97:765–771
Beldi G et al (2006) Laparoscopic ventral hernia repair is safe and cost effective. Surg Endosc 20(1):92–95
Butler RE et al (2007) The economic impact of laparoscopic inguinal hernia repair results of a double-blinded, prospective, randomized trial. Surg Endosc 21(3):387–390
Jacobs VR, Morrison JE (2008) Comparison of institutional costs for laparoscopic preperitoneal inguinal hernia versus open repair and its reimbursement in an ambulatory surgery center. Surg Laparosc Endosc Percut Tech 18(1):70–74
Heikkinen TJ et al (1998) A prospective randomized outcome and cost comparison of totally extraperitoneal endoscopic hernioplasty versus Lichtenstein hernia operation among employed patients. Surg Laparosc Endosc 8(5):338–344
Schneider BE et al (2003) Laparoscopic totally extraperitoneal versus Lichtenstein herniorrhaphy: cost comparison at teaching hospitals. Surg Laparosc Endosc Percut Tech 13(4):216–267
Pielacinski K et al (2011) Self-fixating Progrip implant used in the laparoscopic totally extraperitoneal technique for inguinal hernia repair. Pol Merkur Lekarski 31(186):345–347
Acknowledgments
This research program was supported by Sofradim Production/Covidien, Trévoux, France. Medical writing and editing support were provided by Gaynor Green PhD (Delta Consultants, Eybens, France) Corinne Martinella, Patrice Becker (Sofradim Production/Covidien), M. Fritz, H. J. Klingen, A. Sifft, P. Djalali, W. Schwendich and K. Schwaemmle as participating surgeons.
Conflict of interest
D. B. declares having received a travel grant from Covidien. S. H. declares having no conflict of interest. C. G. P. declares having no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Birk, D., Hess, S. & Garcia-Pardo, C. Low recurrence rate and low chronic pain associated with inguinal hernia repair by laparoscopic placement of Parietex ProGrip™ mesh: clinical outcomes of 220 hernias with mean follow-up at 23 months. Hernia 17, 313–320 (2013). https://doi.org/10.1007/s10029-013-1053-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-013-1053-3