Abstract
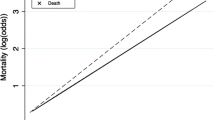
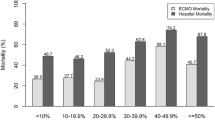
Hemolysis is common during extracorporeal life support (ECLS). Elevated levels of circulating plasma free hemoglobin (FHb) has been linked to the development of hemoglobinuria nephropathy. Its clinical significance in patients receiving ECLS remains unknown. Medical records of 104 children <3 years old who required ECLS after repair of congenital heart disease were reviewed. Forty-two patients required continuous renal replacement therapy (CRRT) during ECLS (CRRT group), and 62 patients did not (no-CRRT group). For all patients, FHb level and the degree of fluid overload at the end of ECLS predicted the mortality rate during ECLS. Compared with the no-CRRT group, the CRRT group had a higher mortality rate during ECLS, a higher peak FHb level during ECLS, a higher FHb level at the end of ECLS, and more days of ECLS. In the CRRT group, the FHb level at the end of ECLS predicted death during ECLS. In the no-CRRT group, the peak FHb level was associated with a worse renal function. In conclusion, elevated FHb levels were associated with renal dysfunction and death during ECLS in children undergoing cardiac surgery. Further studies are needed to elucidate the cause–effect relationship in our findings.
Similar content being viewed by others
References
Steinhorn RH, Isham-Schopf B, Smith C, Green TP (1989) Hemolysis during long-term extracorporeal membrane oxygenation. J Pediatr 115:625–630
Williams AR (1973) Shear-induced fragmentation of human erythrocytes. Biorheology 10:303–311
Shimono T, Makinouchi K, Nose Y (1995) Total erythrocyte destruction time: the new index for the hemolytic performance of rotary blood pumps. Artif Organs 19:571–575
Green TP, Kriesmer P, Steinhorn RH, Payne NR, Irmiter RJ, Meyer CL (1991) Comparison of pressure-volume-flow relationships in centrifugal and roller pump extracorporeal membrane oxygenation systems for neonates. ASAIO Trans 37:572–576
Wielogorski JW, Cross DE, Nwadike EV (1975) The effects of subatmospheric pressure on the haemolysis of blood. J Biomech 8:321–325
Bearss MG (1993) The relationship between membrane oxygenator blood path pressure drop and hemolysis: an in-vitro evaluation. J Extracorpor Technol 25:87–92
Skogby M, Mellgren K, Adrian K, Friberg LG, Chevalier JY, Mellgren G (1998) Induced cell trauma during in vitro perfusion: a comparison between two different perfusion systems. Artif Organs 22:1045–1051
Zager RA, Gamelin LM (1989) Pathogenetic mechanisms in experimental hemoglobinuric acute renal failure. Am J Physiol Renal Physiol 256:F446–F455
Kolovos NS, Bratton SL, Moler FW, Bove EL, Ohye RG, Bartlett RH, Kulik TJ (2003) Outcome of pediatric patients treated with extracorporeal life support after cardiac surgery. Ann Thorac Surg 76:1435–1441
Duncan BW, Hraska V, Jonas RA, Wessel DL, Del Nido PJ, Laussen PC, Mayer JE, Lapierre RA, Wilson JM (1999) Mechanical circulatory support in children with cardiac disease. J Thorac Cardiovasc Surg 117:529–542
Montgomery VL, Strotman JM, Ross MP (2000) Impact of multiple organ system dysfunction and nosocomial infections on survival of children treated with extracorporeal membrane oxygenation after heart surgery. Crit Care Med 28:526–531
Aharon AS, Drinkwater DC Jr, Churchwell KB, Quisling SV, Reddy VS, Taylor M, Hix S, Christian KG, Pietsch JB, Deshpande JK, Kambam J, Graham TP, Chang PA (2001) Extracorporeal membrane oxygenation in children after repair of congenital cardiac lesions. Ann Thorac Surg 72:2095–2101
Hasegawa T, Yamaguchi M, Yoshimura N, Okita Y (2005) The dependence of myocardial damage on age and ischemic time in pediatric cardiac surgery. J Thorac Cardiovasc Surg 129:192–198
Swaniker F, Kolla S, Moler F, Custer J, Grams R, Barlett R, Hirschl R (2000) Extracorporeal life support outcome for 128 pediatric patients with respiratory failure. J Pediatr Surg 35:197–202
Schwartz GJ, Brion LP, Spitzer A (1987) The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am 34:571–590
Mehta U, Laks H, Sadeghi A, Marelli D, Odim J, Alejos J, Kim M, Atkinson JB, Bui KC (2000) Extracorporeal membrane oxygenation for cardiac support in pediatric patients. Am Surg 66:879–886
Raithel SC, Pennington DG, Boegner E, Fiore A, Weber TR (1992) Extracorporeal membrane oxygenation in children after cardiac surgery. Circulation 86:II305–II310
Shah SA, Shankar V, Churchwell KB, Taylor MB, Scott BP, Bartilson R, Byrne DW, Christian KG, Drinkwater DC (2005) Clinical outcomes of 84 children with congenital heart disease managed with extracorporeal membrane oxygenation after cardiac surgery. ASAIO J 51:504–507
Baslaim G, Bashore J, Al-Malki F, Jamjoom A (2006) Can the outcome of pediatric extracorporeal membrane oxygenation after cardiac surgery be predicted? Ann Thorac Cardiovasc Surg 12:21–27
Meyer RJ, Brophy PD, Bunchman TE, Annich GM, Maxvold NJ, Mottes TA, Custer JR (2001) Survival and renal function in pediatric patients following extracorporeal life support with hemofiltration. Pediatr Crit Care Med 2:238–242
Humphrey H, Hall J, Sznajder I, Silverstein M, Wood L (1990) Improved survival in ARDS patients associated with a reduction in pulmonary capillary wedge pressure. Chest 97:1176–1180
Schuller D, Mitchell JP, Calandrino FS, Schuster DP (1991) Fluid balance during pulmonary edema. Is fluid gain a marker or a cause of poor outcome? Chest 100:1068–1075
Goldstein SL, Currier H, Graf C, Cosio CC, Brewer ED, Sachdeva R (2001) Outcome in children receiving continuous venovenous hemofiltration. Pediatrics 107:1309–1312
Haussinger D, Lang F, Gerok W (1994) Regulation of cell function by the cellular hydration state. Am J Physiol Endocrinol Metab 267:E343–E355
Betrus C, Remenapp R, Charpie J, Kudelka T, Brophy P, Smoyer WE, Lin JJ (2007) Enhanced hemolysis in pediatric patients requiring extracorporeal membrane oxygenation and continuous renal replacement therapy. Ann Thorac Cardiovasc Surg 13:378–383
De Wachter DS, Verdonck PR, De Vos JY, Hombrouckx RO (1997) Blood trauma in plastic haemodialysis cannulae. Int J Artif Organs 20:366–370
Luckraz H, Woods M, Large SR (2002) And hemolysis goes on: ventricular assist device in combination with veno-venous hemofiltration. Ann Thorac Surg 73:546–548
Bunn HF, Esham WT, Bull RW (1969) The renal handling of hemoglobin. I. Glomerular filtration. J Exp Med 129:909–923
Jaenike JR (1966) The renal lesion associated with hemoglobinemia. I. Its production and functional evolution in the rat. J Exp Med 123:523–535
Gburek J, Verroust PJ, Willnow TE, Fyfe JC, Nowacki W, Jacobsen C, Moestrup SK, Christensen EI (2002) Megalin and cubilin are endocytic receptors involved in renal clearance of hemoglobin. J Am Soc Nephrol 13:423–430
Lieberthal W (1995) Stroma-free hemoglobin: a potential blood substitute. J Lab Clin Med 126:231–232
Paller MS, Hedlund BE (1988) Role of iron in postischemic renal injury in the rat. Kidney Int 34:474–480
Lieberthal W, Fuhro R, Andry C, Valeri CR (2000) Effects of hemoglobin-based oxygen-carrying solutions in anesthetized rats with acute ischemic renal failure. J Lab Clin Med 135:73–81
Vogel WM, Dennis RC, Cassidy G, Apstein CS, Valeri CR (1986) Coronary constrictor effect of stroma-free hemoglobin solutions. Am J Physiol Heart Circ Physiol 251:H413–H420
Rother RP, Bell L, Hillmen P, Gladwin MT (2005) The clinical sequelae of intravascular hemolysis and extracellular plasma hemoglobin: a novel mechanism of human disease. JAMA 293:1653–1662
Kulik TJ, Moler FW, Palmisano JM, Custer JR, Mosca RS, Bove EL, Bartlett RH (1996) Outcome-associated factors in pediatric patients treated with extracorporeal membrane oxygenator after cardiac surgery. Circulation 94(9 Suppl):II63–II68
Ando M, Takahashi Y, Kikuchi T, Short operation time (2005) An important element to reduce operative invasiveness in pediatric cardiac surgery. Ann Thorac Surg 80:631–635
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gbadegesin, R., Zhao, S., Charpie, J. et al. Significance of hemolysis on extracorporeal life support after cardiac surgery in children. Pediatr Nephrol 24, 589–595 (2009). https://doi.org/10.1007/s00467-008-1047-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-008-1047-z