Abstract
Background
Laparoscopic deroofing is widely used for the treatment of symptomatic polycystic liver disease (PCLD). However, bile leakage is a common complication of surgical management for PCLD. Until now, indocyanine green fluorescence imaging (IGFI) has played an active role in hepatobiliary surgery. Herein, we report the effective application of a laparoscopic fusion IGFI system, known as PINPOINT, for laparoscopic deroofing.
Methods
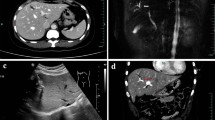
In this study, we performed laparoscopic deroofing for PCLD using the laparoscopic fusion IGFI system. We conducted the procedure mainly under the normal view mode, occasionally switching to the fusion IGFI mode. First, we confirmed that the liver cysts did not contain bile using the fusion IGFI mode and then used a percutaneous puncture needle to remove the fluid from some of the giant cysts. Second, using the fusion IGFI mode, we were able to detect thin biliary branches and to adjust the division line of the cyst wall accordingly or, occasionally, to ligate the branches. Finally, we searched for and identified unexpected small bile leakage and then closed it using sutures.
Results
The laparoscopic fusion IGFI system can simultaneously show fluorescent images, such as cholangiography and the liver parenchyma, on the normal color view. In the fusion IGFI mode, the intrahepatic bile duct and liver parenchyma can be easily discriminated in real time throughout the procedure. Accordingly, the laparoscopic fusion IGFI system is useful for the surgical treatment of PCLD, in which the boundary between the liver cysts and the liver parenchyma can otherwise be difficult to identify. This technique also enables the branches of Glisson’s capsule to be identified without any other intervention.
Conclusion
The novel application of the laparoscopic fusion IGFI system allows reliable navigation for PCLD surgery.
Similar content being viewed by others
Abbreviations
- PCLD:
-
Polycystic liver disease
- IGFI:
-
Indocyanine green fluorescence imaging
- ICG:
-
Indocyanine green
- ICG-R15:
-
Indocyanine green retention rate at 15 min
References
Ogawa K, Fukunaga K, Takeuchi T, Kawagishi N, Ubara Y, Kudo M, Ohkohchi N (2013) Current treatment status of polycystic liver disease in Japan. Hepatol Res 44:1110–1118
Ardito F, Bianco G, Vellone M, Sarno G, Ranucci G, Giovannini I, Giuliante F (2013) Long-term outcome after laparoscopic fenestration of simple liver cysts. Surg Endosc 27:4670–4674
Yamada T, Furukawa K, Yokoi K, Mamada Y, Kanazawa Y, Tajiri T (2009) Liver cysts with biliary communication successfully treated with laparoscopic deroofing. A case report. J Nippon Med Sch 76:103–108
Imamura H, Kawashita Y, Koga N, Sanada Y, Azuma T, Matsuo S, Eguchi S (2013) A large hepatic cyst with obstructive jaundice successfully treated with single-incision laparoscopic deroofing. Case Rep Gastroenterol 7:503–510
Szabo LS, Takacs I, Arkosy P, Sapy P, Szentkereszty Z (2006) Laparoscopic treatment of nonparasitic hepatic cysts. Surg Endosc 20:595–597
Qiu JG, Wu H, Jiang H, Huang JW, Pankaj P, Xu YL, Wang JZ, Zeng Y (2011) Laparoscopic fenestration vs open fenestration in patients with congenital hepatic cysts: a meta-analysis. World J Gastroenterol 17:3359–3365
Zaharie F, Bartos D, Mocan L, Zaharie R, Iancu C, Tomus C (2013) Open or laparoscopic treatment for hydatid disease of the liver? A 10-year single-institution experience. Surg Endosc 27:2110–2116
Coelho-Prabhu N, Nagorney DM, Baron TH (2012) ERCP for the treatment of bile leak after partial hepatectomy and fenestration for symptomatic polycystic liver disease. World J Gastroenterol 18:3705–3709
Hansman MF, Ryan JA, Holmes JH, Hogan S, Lee FT, Kramer D, Biehl T (2001) Management and long-term follow-up of hepatic cysts. Am J Surg 181:404–410
Cui W, Zhou HY, Zhang YH, Zhang T, Li Q (2013) Surgical management of non-parasitic hepatic cyst with biliary communication: a case report. Cancer Biol Med 10:110–113
Ishizawa T, Bandai Y, Ijichi M, Kaneko J, Hasegawa K, Kokudo N (2010) Fluorescent cholangiography illuminating the biliary tree during laparoscopic cholecystectomy. Br J Surg 97:1369–1377
Morita K, Ishizawa T, Tani K, Harada N, Shimizu A, Yamamoto S, Takemura N, Kaneko J, Aoki T, Sakamoto Y, Sugawara Y, Hasegawa K, Kokudo N (2014) Application of indocyanine green-fluorescence imaging to full-thickness cholecystectomy. Asian J Endosc Surg 7:193–195
Ishizawa T, Kaneko J, Inoue Y, Takemura N, Seyama Y, Aoki T, Beck Y, Sugawara Y, Hasegawa K, Harada N, Ijichi M, Kusaka K, Shibasaki M, Bandai Y, Kokudo N (2011) Application of fluorescent cholangiography to single-incision laparoscopic cholecystectomy. Surg Endosc 25:2631–2636
Kawaguchi Y, Ishizawa T, Masuda K, Sato S, Kaneko J, Aoki T, Beck Y, Sugawara Y, Hasegawa K, Kokudo N (2011) Hepatobiliary surgery guided by a novel fluorescent imaging technique for visualizing hepatic arteries, bile ducts, and liver cancers on color images. J Am Coll Surg 212:e33–e39
Ishizawa T, Tamura S, Masuda K, Aoki T, Hasegawa K, Imamura H, Beck Y, Kokudo N (2009) Intraoperative fluorescent cholangiography using indocyanine green: a biliary road map for safe surgery. J Am Coll Surg 208:e1–e4
Inoue Y, Arita J, Sakamoto T, Ono Y, Takahashi M, Takahashi Y, Kokudo N, Saiura A (2015) Anatomical liver resection guided by 3-dimensional parenchymal staining using fusion indocyanine green fluorescence imaging. Ann Surg (Epub ahead of print)
Cherrick GR, Stein SW, Leevy CM, Davidson CS (1960) Indocyanine green: observations on its physical properties, plasma decay, and hepatic extraction. J Clin Investig 39:592–600
Yano K, Nimura H, Mitsumori N, Takahashi N, Kashiwagi H, Yanaga K (2012) The efficiency of micrometastasis by sentinel node navigation surgery using indocyanine green and infrared ray laparoscopy system for gastric cancer. Gastric Cancer 15:287–291
Ishizawa T, Masuda K, Urano Y, Kawaguchi Y, Satou S, Kaneko J, Hasegawa K, Shibahara J, Fukayama M, Tsuji S, Midorikawa Y, Aburatani H, Kokudo N (2014) Mechanistic background and clinical applications of indocyanine green fluorescence imaging of hepatocellular carcinoma. Ann Surg Oncol 21:440–448
Ishizawa T, Fukushima N, Shibahara J, Masuda K, Tamura S, Aoki T, Hasegawa K, Beck Y, Fukayama M, Kokudo N (2009) Real-time identification of liver cancers by using indocyanine green fluorescent imaging. Cancer 115:2491–2504
Kudo H, Ishizawa T, Tani K, Harada N, Ichida A, Shimizu A, Kaneko J, Aoki T, Sakamoto Y, Sugawara Y, Hasegawa K, Kokudo N (2014) Visualization of subcapsular hepatic malignancy by indocyanine-green fluorescence imaging during laparoscopic hepatectomy. Surg Endosc 28:2504–2508
Ris F, Hompes R, Cunningham C, Lindsey I, Guy R, Jones O, George B, Cahill RA, Mortensen NJ (2014) Near-infrared (NIR) perfusion angiography in minimally invasive colorectal surgery. Surg Endosc 28:2221–2226
Acknowledgments
Yosuke Inoue participated in the operation and supervised the writing of the paper. Yoshihiro Mise, Takeaki Ishizawa, and Yu Takahashi also supervised the writing of the paper. Akio Saiura represents our surgical department and supervised the writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Masayuki Tanaka, Yosuke Inoue, Yoshihiro Mise, Takeaki Ishizawa, Junichi Arita, Yu Takahashi and Akio Saiura read and approved the final manuscript and declare that they have no conflicts of interest or financial ties to disclose.
Informed consent
Written informed consent was obtained from the patient for the publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 2 (WMV 45426 kb)
Rights and permissions
About this article
Cite this article
Tanaka, M., Inoue, Y., Mise, Y. et al. Laparoscopic deroofing for polycystic liver disease using laparoscopic fusion indocyanine green fluorescence imaging. Surg Endosc 30, 2620–2623 (2016). https://doi.org/10.1007/s00464-015-4526-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4526-x