Abstract
Background
We examined the impact of muscle relaxation on surgical conditions and patients’ postoperative outcome during elective laparoscopic cholecystectomy under balanced anaesthesia.
Methods
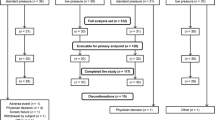
After approval and consent, 57 anaesthetized patients were randomly assigned to group no neuromuscular blockade (No NMB) and deep neuromuscular blockade (Deep NMB), i.e. no twitch response to train-of-four nerve stimulation. Laparoscopic cholecystectomy was performed using the 4-trocar technique with a CO2-pneumoperitoneum. Surgical conditions were assessed using a Visual Analogue Scale. Movement of diaphragm or abdominal muscles, inadequate visibility, or breathing and coughing against the ventilator were documented as events reflecting inadequate muscle relaxation. Independently, surgeons could request 0.3 mg/kg rocuronium to improve surgical conditions. Workflow variables were obtained as a surrogate of surgical conditions. Data are presented as mean (95 % confidence interval). The trial is registered at ClinicalTrials.gov (NCT00895778).
Results
While in 12 of 25 patients of group “No NMB” one or more adverse events impaired the surgical procedure (p < 0.001), only 1 of 25 patients of group “Deep NMB” showed an adverse event. Deep NMB resulted in an absolute risk reduction of 0.44 (0.23–0.65) and a number needed to treat of 2.3 (1.5–4.4), respectively. Surgeons requested 0.3 mg/kg rocuronium in 10 of 25 cases (40 %) of group “No NMB” only. This dose significantly improved surgical conditions by an average 62 of 100 possible points. All further variables did not differ between groups.
Conclusions
Deep NMB ameliorates surgical conditions for laparoscopic cholecystectomy by improved visibility and reduction of involuntary movements.





Similar content being viewed by others
References
Lawen (1912) Über die Verbindung der Lokalanästhesia mit der Narkose, über hohe Extraduralanästhesie und epidurale Injektionen anästhesierender Lösungen bei tabischen Magenkrisen. Beitr zur Klin Chir 80:168–189
Griffith HR, Johnson GE (1942) The use of curare in general anesthesia. Anesthesiology 3:418–420
Mencke T, Echternach M, Kleinschmidt S, Lux P, Barth V, Plinkert PK, Fuchs-Buder T (2003) Laryngeal morbidity and quality of tracheal intubation: a randomized controlled trial. Anesthesiology 98:1049–1056
Sandin RH, Enlund G, Samuelsson P, Lennmarken C (2000) Awareness during anaesthesia: a prospective case study. Lancet 355:707–711
Viby-Mogensen J, Jorgensen BC, Ording H (1979) Residual curarization in the recovery room. Anesthesiology 50:539–541
Hayes AH, Mirakhur RK, Breslin DS, Reid JE, McCourt KC (2001) Postoperative residual block after intermediate-acting neuromuscular blocking drugs. Anaesthesia 56:312–318
Debaene B, Plaud B, Dilly MP, Donati F (2003) Residual paralysis in the PACU after a single intubating dose of nondepolarizing muscle relaxant with an intermediate duration of action. Anesthesiology 98:1042–1048
Eikermann M, Blobner M, Groeben H, Rex C, Grote T, Neuhauser M, Beiderlinden M, Peters J (2006) Postoperative upper airway obstruction after recovery of the train of four ratio of the adductor pollicis muscle from neuromuscular blockade. Anesth Analg 102:937–942
Berg H, Roed J, Viby-Mogensen J, Mortensen CR, Engbaek J, Skovgaard LT, Krintel JJ (1997) Residual neuromuscular block is a risk factor for postoperative pulmonary complications. A prospective, randomised, and blinded study of postoperative pulmonary complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand 41:1095–1103
Butterly A, Bittner EA, George E, Sandberg WS, Eikermann M, Schmidt U (2010) Postoperative residual curarization from intermediate-acting neuromuscular blocking agents delays recovery room discharge. Br J Anaesth 105:304–309
Jones RK, Caldwell JE, Brull SJ, Soto RG (2008) Reversal of profound rocuronium-induced blockade with sugammadex: a randomized comparison with neostigmine. Anesthesiology 109:816–824
Schaller SJ, Fink H (2013) Sugammadex as a reversal agent for neuromuscular block: an evidence-based review. Core Evid 8:57–67
Feussner H, Ungeheuer A, Lehr L, Siewert JR (1991) Technique of laparoscopic cholecystectomy. Langenbecks Arch Chir 376:367–374
Fanelli G, Berti M, Casati A (2006) Fast-track anaesthesia for laparoscopic cholecystectomy: a prospective, randomized, multicentre, blind comparison of desflurane-remifentanil or sevoflurane-remifentanil. Eur J Anaesthesiol 23:861–868
Jensen K, Kehlet H, Lund CM (2007) Post-operative recovery profile after laparoscopic cholecystectomy: a prospective, observational study of a multimodal anaesthetic regime. Acta Anaesthesiol Scand 51:464–471
Fuchs-Buder T, Claudius C, Skovgaard LT, Eriksson LI, Mirakhur RK, Viby-Mogensen J (2007) Good clinical research practice in pharmacodynamic studies of neuromuscular blocking agents II: the Stockholm revision. Acta Anaesthesiol Scand 51:789–808
Schoh RJ, Fero LJ, Shapiro H, Aslor JP, Kaelin OJ, Rollins DR, Petty TL (2002) Performance of a new screening spirometer at a community health fair. Respir Care 47:1150–1157
King M, Sujirattanawimol N, Danielson DR, Hall BA, Schroeder DR, Warner DO (2000) Requirements for muscle relaxants during radical retropubic prostatectomy. Anesthesiology 93:1392–1397
Gurusamy KS, Samraj K, Davidson BR (2009) Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst Rev 2:CD006930
Murphy GS, Szokol JW, Marymont JH, Greenberg SB, Avram MJ, Vender JS (2008) Residual neuromuscular blockade and critical respiratory events in the postanesthesia care unit. Anesth Analg 107:130–137
Kreuzer M, Zanner R, Pilge S, Paprotny S, Kochs EF, Schneider G (2012) Time delay of monitors of the hypnotic component of anesthesia: analysis of state entropy and index of consciousness. Anesth Analg 115:315–319
De Jong RH (1966) Controlled relaxation. I. Quantitation of electromyogram with abdominal relaxation. JAMA 197:393–395
Gild WM, Posner KL, Caplan RA, Cheney FW (1992) Eye injuries associated with anesthesia. A closed claims analysis. Anesthesiology 76:204–208
Disclosures
Prof. Manfred Blobner has received honoraria from GlaxoSmithKline and MSD Sharp & Dohme. Dr. Christiane Frick has received honoraria and a travel grant from MSD Sharpe & Dohme. Dr. Stefan Schaller holds stocks of the following companies in the healthcare sector in small amounts: Bayer AG, Siemens AG, GE, MERCK & CO INC, Rhoen-Klinikum AG and Fresenius SE. However, these holdings do not influence any decisions regarding the study. Dr. Heidrun Fink has received honoraria and travel grants from the following companies: MSD Sharp & Dohme, Essex, Baxter, Care Fusion, GE Healthcare. Prof. Dr. Feussner and Drs. Stäuble, Unterbuchner, Lingg and Geisler have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
The work was performed at: Klinik für Anaesthesiologie and Chirurgische Klinik, Technische Universität München, Klinikum rechts der Isar, Munich, Germany.
Rights and permissions
About this article
Cite this article
Blobner, M., Frick, C.G., Stäuble, R.B. et al. Neuromuscular blockade improves surgical conditions (NISCO). Surg Endosc 29, 627–636 (2015). https://doi.org/10.1007/s00464-014-3711-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3711-7