Abstract
Background
Laparoscopic liver surgery is particularly challenging owing to restricted access, risk of bleeding, and lack of haptic feedback. Navigation systems have the potential to improve information on the exact position of intrahepatic tumors, and thus facilitate oncological resection. This study aims to evaluate the feasibility of a commercially available augmented reality (AR) guidance system employing intraoperative robotic C-arm cone-beam computed tomography (CBCT) for laparoscopic liver surgery.
Methods
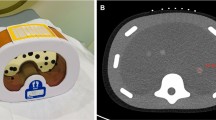
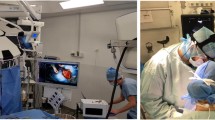
A human liver-like phantom with 16 target fiducials was used to evaluate the Syngo iPilot® AR system. Subsequently, the system was used for the laparoscopic resection of a hepatocellular carcinoma in segment 7 of a 50-year-old male patient.
Results
In the phantom experiment, the AR system showed a mean target registration error of 0.96 ± 0.52 mm, with a maximum error of 2.49 mm. The patient successfully underwent the operation and showed no postoperative complications.
Conclusion
The use of intraoperative CBCT and AR for laparoscopic liver resection is feasible and could be considered an option for future liver surgery in complex cases.





Similar content being viewed by others
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61(2):69–90
Peterhans M, Oliveira T, Banz V, Candinas D, Weber S (2012) Computer-assisted liver surgery: clinical applications and technological trends. Crit Rev Biomed Eng 40(3):199–220
Najmaei N, Mostafavi K, Shahbazi S, Azizian M (2012) Image-guided techniques in renal and hepatic interventions. Int J Med Robot. doi:10.1002/rcs.1443
Oliveira DA, Feitosa RQ, Correia MM (2011) sation of liver, its vessels and lesions from CT images for surgical planning. Biomed Eng Online 10:30
Nam WH, Kang DG, Lee D, Lee JY, Ra JB (2012) Automatic registration between 3D intra-operative ultrasound and pre-operative CT images of the liver based on robust edge matching. Phys Med Biol 57(1):69–91
Zijlmans M, Langø T, Hofstad EF, Van Swol CFP, Rethy A (2012) Navigated laparoscopy—liver shift and deformation due to pneumoperitoneum in an animal model. Minim Invasive Ther Allied Technol 21(3):241–248
Bussels B, Goethals L, Feron M, Bielen D, Dymarkowski S, Suetens P, Haustermans K (2003) Respiration-induced movement of the upper abdominal organs: a pitfall for the three-dimensional conformal radiation treatment of pancreatic cancer. Radiother Oncol 68(1):69–74
Stoykov SA. Micro Dicom viewer. http://www.microdicom.com. Accessed June 2013
R Core Team (2012) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. http://www.R-project.org. Accessed June 2013
Gumbs AA, Gayet B, Gagner M (2008) Laparoscopic liver resection: when to use the laparoscopic stapler device. HPB (Oxf) 10(4):296–303
Nozaki T, Iida Y, Morii A, Fujiuchi Y, Fuse H (2012) Laparoscopic radical nephrectomy under near real-time three-dimensional surgical navigation with C-arm cone beam computed tomography. Surg Innov 19(3):263–267
Nozaki T, Fujiuchi Y, Komiya A, Fuse H (2013) Efficacy of DynaCT for surgical navigation during complex laparoscopic surgery: an initial experience. Surg Endosc 27(3):903–909
Rossitti S, Pfister M (2009) 3D road-mapping in the endovascular treatment of cerebral aneurysms and arteriovenous malformations. Interv Neuroradiol 15(3):283–290
Ieiri S, Uemura M, Konishi K, Souzaki R, Nagao Y, Tsutsumi N, Akahoshi T, Ohuchida K, Ohdaira T, Tomikawa M, Zanoue K, Hashizume M, Taguchi T (2012) Augmented reality navigation system for laparoscopic splenectomy in children based on preoperative CT image using optical tracking device. Pediatr Surg Int 28(4):341–346
Nicolau S, Soler L, Mutter D, Marescaux J (2011) Augmented reality in laparoscopic surgical oncology. Surg Oncol 20(3):189–201
Shekhar R, Dandekar O, Bhat V, Philip M, Lei P, Godinez C, Sutton E, George I, Kavic S, Mezrich R, Park A (2010) Live augmented reality: a new visualization method for laparoscopic surgery using continuous volumetric computed tomography. Surg Endosc 24(8):1976–1985
Vemuri AS, Wu JCH, Liu KC, Wu HS (2012) Deformable three-dimensional model architecture for interactive augmented reality in minimally invasive surgery. Surg Endosc 26(12):3655–3662
Teber D, Guven S, Simpfendörfer T, Baumhauer M, Güven EO, Yencilek F, Gözen AS, Rassweiler J (2009) Augmented reality: a new tool to improve surgical accuracy during laparoscopic partial nephrectomy? Preliminary in vitro and in vivo results. Eur Urol 56(2):332–338
Våpenstad C, Rethy A, Langø T, Selbekk T, Ystgaard B, Hernes TA, Marvik R (2010) Laparoscopic ultrasound: a survey of its current and future use, requirements, and integration with navigation technology. Surg Endosc 24(12):2944–2953
Rassweiler MC, Ritter M, Michel MS, Häcker A (2013) Influence of endourological devices on 3D reconstruction image quality using the Uro Dyna-CT. World J Urol 31(5):1291–1295
Bai M, Liu B, Mu H, Liu X, Jiang Y (2012) The comparison of radiation dose between C-arm flat-detector CT (DynaCT) and multi-slice CT (MSCT): a phantom study. Eur J Radiol 81(11):3577–3580. http://www.ncbi.nlm.nih.gov/pubmed/21963617
Kenngott HG, Wegner I, Neuhaus J, Nickel F, Fischer L, Gehrig T, Meinzer HP, Müller-Stich BP (2013) Magnetic tracking in the operation room using the da Vinci® telemanipulator is feasible. J Robot Surg 7(1):59–64
Kenngott HG, Neuhaus J, Müller-Stich BP, Wolf I, Vetter M, Meinzer HP, Köninger J, Büchler MW, Gutt CN (2008) Development of a navigation system for minimally invasive esophagectomy. Surg Endosc 22(8):1858–1865
Koelblinger C, Schima W, Berger-Kulemann V, Wolf F, Plank C, Weber M, Lammer J (2013) C-arm CT during hepatic arteriography tumour-to-liver contrast: intraindividual comparison of three different contrast media application protocols. Eur Radiol 23(4):938–942
Worm ES, Høyer M, Fledelius W, Nielsen JE, Larsen LP, Poulsen PR (2012) On-line use of three-dimensional marker trajectory estimation from cone-beam computed tomography projections for precise setup in radiotherapy for targets with respiratory motion. Int J Radiat Oncol Biol Phys 83(1):e145–e151
Acknowledgments
The authors thank Siemens AG, Healthcare Sector, for providing expert personnel during the evaluation to calibrate and operate the system during the intervention. In particular, we would like to thank Martin von Roden for his excellent contribution. Professor Böckler received a research grant and speaker honoraria from Siemens AG. Dr. Müller-Stich received reimbursements of travel expenses from Siemens AG, Erlangen, Germany. This research was supported by the Transregional Collaborative Research Centre (TCRC) ‘Cognition-Guided Surgery’ and the Research Training Group 1126 both funded by the DFG (German Research Foundation).
Disclosures
Drs. Kenngott, Wagner, Gondan, Nickel, Nolden, Fetzer, Weitz, Fischer, Meinzer and Büchler have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kenngott, H.G., Wagner, M., Gondan, M. et al. Real-time image guidance in laparoscopic liver surgery: first clinical experience with a guidance system based on intraoperative CT imaging. Surg Endosc 28, 933–940 (2014). https://doi.org/10.1007/s00464-013-3249-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3249-0