Abstract
Background
Preliminary studies have indicated clinical advantages of mesh fixation using fibrin glue in transabdominal preperitoneal groin hernia repair (TAPP) compared with tack fixation. The aim of this randomized double-blinded, controlled, clinical trial is to compare fibrin glue with tacks fixation of mesh during TAPP.
Methods
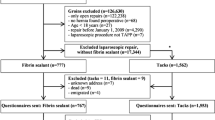
One hundred and twelve men with unilateral inguinal hernia were enrolled. Primary outcome was pain during coughing on postoperative day 1. Secondary outcomes were postoperative scores of pain at rest, discomfort, and fatigue (day 1 and cumulated day 0–3), incidence of moderate/severe nausea and/or vomiting, foreign-body sensation, and recurrence after 6 months. Outcome measures were assessed by visual analogue scale (VAS, 0–100 mm), verbal rating scale (no, light, moderate or severe) and numerical rating scales (NRS, 1–10).
Results
One hundred patients were available for analysis. The fibrin group (n = 50) had significantly less pain during coughing on day 1 compared with the tacks group (n = 50) [median 23 (range 0–80) vs 35 (2–100) mm] (p = 0.020). Moreover, day 1 scores and all cumulated scores of pain during rest, discomfort, and fatigue were significantly lower in the fibrin group compared with the tacks group (all p-values ≤ 0.02). There was no significant difference in the incidence of nausea and/or vomiting (p > 0.05) or recurrence (fibrin glue n = 2, tacks n = 0, p = 0.241). Incidence of foreign-body sensation was significantly lower in the fibrin group at 1 month (p = 0.006).
Conclusions
Fibrin glue compared with tacks fixation improved the early postoperative outcome after TAPP. The trial was registered at clinicaltrials.gov NCT01000116.


Similar content being viewed by others
References
Boldo E, Armelles A, de Perez LG, Martin F, Aracil JP, Miralles JM, Martinez D, Escrig J (2008) Pain after laparascopic bilateral hernioplasty : Early results of a prospective randomized double-blind study comparing fibrin versus staples. Surg Endosc 22:1206–1209
Olmi S, Scaini A, Erba L, Guaglio M, Croce E (2007) Quantification of pain in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernioplasty identifies marked differences between prosthesis fixation systems. Surgery 142:40–46
Fortelny RH, Petter-Puchner AH, May C, Jaksch W, Benesch T, Khakpour Z, Redl H, Glaser KS (2012) The impact of atraumatic fibrin sealant vs. staple mesh fixation in TAPP hernia repair on chronic pain and quality of life: results of a randomized controlled study. Surg Endosc 26:249–254
Bittner R, Gmahle E, Gmahle B, Schwarz J, Aasvang E, Kehlet H (2010) Lightweight mesh and noninvasive fixation: an effective concept for prevention of chronic pain with laparoscopic hernia repair (TAPP). Surg Endosc 24:2958–2964
Ceccarelli G, Casciola L, Pisanelli MC, Bartoli A, Di ZL, Spaziani A, Biancafarina A, Stefanoni M, Patriti A (2008) Comparing fibrin sealant with staples for mesh fixation in laparoscopic transabdominal hernia repair: a case control-study. Surg Endosc 22:668–673
Lau H (2005) Fibrin sealant versus mechanical stapling for mesh fixation during endoscopic extraperitoneal inguinal hernioplasty: a randomized prospective trial. Ann Surg 242:670–675
Bay-Nielsen M, Thomsen H, Andersen FH, Bendix JH, Sorensen OK, Skovgaard N, Kehlet H (2004) Convalescence after inguinal herniorrhaphy. Br J Surg 91:362–367
Pavlin DJ, Chen C, Penaloza DA, Polissar NL, Buckley FP (2002) Pain as a factor complicating recovery and discharge after ambulatory surgery. Anesth Analg 95:627–634
Callesen T, Klarskov B, Bech K, Kehlet H (1999) Short convalescence after inguinal herniorrhaphy with standardised recommendations: duration and reasons for delayed return to work. Eur J Surg 165:236–241
Kehlet H, Jensen TS, Woolf CJ (2006) Persistent postsurgical pain: risk factors and prevention. Lancet 367:1618–1625
McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, Vale L, Grant A (2005) Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess 9:1–203, iii–iv
Christensen T, Bendix T, Kehlet H (1982) Fatigue and cardiorespiratory function following abdominal surgery. Br J Surg 69:417–419
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother 1:100–107
Bittner R, Schmedt CG, Schwarz J, Kraft K, Leibl BJ (2002) Laparoscopic transperitoneal procedure for routine repair of groin hernia. Br J Surg 89:1062–1066
Tolver MA, Strandfelt P, Rosenberg J, Bisgaard T (2011) Pain characteristics after laparoscopic inguinal hernia repair. Surg Endosc 25:3859–3864
Tanphiphat C, Tanprayoon T, Sangsubhan C, Chatamra K (1998) Laparoscopic vs open inguinal hernia repair. A randomized, controlled trial. Surg Endosc 12:846–851
Gallagher EJ, Liebman M, Bijur PE (2001) Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med 38:633–638
Todd KH, Funk KG, Funk JP, Bonacci R (1996) Clinical significance of reported changes in pain severity. Ann Emerg Med 27:485–489
Wei L, Zhang J (2001) Analysis of data with imbalance in the baseline outcome variable for randomized clinical trials. Drug information journal 35:1201–1214
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg 245:222–231
Topart P, Vandenbroucke F, Lozac’h P (2005) Tisseel versus tack staples as mesh fixation in totally extraperitoneal laparoscopic repair of groin hernias: a retrospective analysis. Surg Endosc 19:724–727
Schwab R, Willms A, Kroger A, Becker HP (2006) Less chronic pain following mesh fixation using a fibrin sealant in TEP inguinal hernia repair. Hernia 10:272–277
Novik B, Hagedorn S, Mork UB, Dahlin K, Skullman S, Dalenback J (2006) Fibrin glue for securing the mesh in laparoscopic totally extraperitoneal inguinal hernia repair: a study with a 40-month prospective follow-up period. Surg Endosc 20:462–467
Santoro E, Agresta F, Buscaglia F, Mulieri G, Mazzarolo G, Bedin N, Mulieri M (2007) Preliminary experience using fibrin glue for mesh fixation in 250 patients undergoing minilaparoscopic transabdominal preperitoneal hernia repair. J Laparoendosc Adv Surg Tech A 17:12–15
Fortelny RH, Petter-Puchner AH, Glaser KS, Redl H (2012) Use of fibrin sealant (Tisseel/Tissucol) in hernia repair: a systematic review. Surg Endosc 26:1803–1812
Eriksen JR, Poornoroozy P, Jorgensen LN, Jacobsen B, Friis-Andersen HU, Rosenberg J (2009) Pain, quality of life and recovery after laparoscopic ventral hernia repair. Hernia 13:13–21
Kehlet H, Dahl JB (2003) Anaesthesia, surgery, and challenges in postoperative recovery. Lancet 362:1921–1928
Kaul A, Hutfless S, Le H, Hamed SA, Tymitz K, Nguyen H, Marohn MR (2012) Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc 26:1269–1278
Bisgaard T, Schulze S, Christian HN, Rosenberg J, Bjerregaard KV (2008) Randomized clinical trial comparing oral prednisone (50 mg) with placebo before laparoscopic cholecystectomy. Surg Endosc 22:566–572
Karanicolas PJ, Smith SE, Kanbur B, Davies E, Guyatt GH (2008) The impact of prophylactic dexamethasone on nausea and vomiting after laparoscopic cholecystectomy: a systematic review and meta-analysis. Ann Surg 248:751–762
Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Kockerling F, Kuhry E et al (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25:2773–2843
Acknowledgments
The authors thank Region Zealand’s Health Research Fund (RESUS) for financial support and private hospital Aleris-Hamlet for use of their facilities. Additionally, we would like to thank Research Nurse Pernille Strandfelt for assistance in data collection during the trial.
Disclosures
Mette A. Tolver has received payment for lectures by Baxter Healthcare. Jacob Rosenberg has received payment for expert testimony from Baxter Healthcare and has had travel/accommodation expenses for international meetings covered by Johnson & Johnson. Poul Juul has no conflicts of interest. The Bisgaard has received support from Johnson & Johnson, Covidien and Baxter Healthcare and travel/accommodation expenses for international meetings covered by Baxter Healthcare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tolver, M.A., Rosenberg, J., Juul, P. et al. Randomized clinical trial of fibrin glue versus tacked fixation in laparoscopic groin hernia repair. Surg Endosc 27, 2727–2733 (2013). https://doi.org/10.1007/s00464-012-2766-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2766-6