Abstract
Background
The incidence of cancer in the proximal third of the stomach is increasing. Laparoscopic proximal gastrectomy (LPG) seems an attractive option for the treatment of early-stage proximal gastric cancer but has not gained wide acceptance because of technical difficulties, including the prevention of severe reflux. In this study, we describe our technique for LPG with jejunal interposition (LPG-IP) and evaluate its safety and feasibility.
Methods
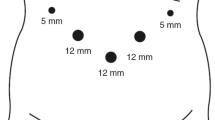
In this retrospective analysis, we reviewed the data of patients with proximal gastric cancer who underwent LPG-IP (n = 22) or the same procedure with open surgery (OPG-IP; n = 68) between January 2008 and September 2011. Short-term surgical variables and outcomes were compared between the groups. The reconstruction method was the same in both groups, with creation of a 15 cm, single-loop, jejunal interposition for anastomosis.
Results
There were no differences in patient or tumor characteristics between the groups. Operation time was longer in the LGP-IP group (233 vs. 201 min, p = 0.0002) and estimated blood loss was significantly less (20 vs. 242 g, p < 0.0001). The average number of harvested lymph nodes did not differ between the two groups (17 vs. 20). There also were no differences in the incidence of leakage at the esophagojejunostomy anastomosis (9.1 vs. 7.4 %) or other postoperative complications (27 vs. 32 %). The number of times additional postoperative analgesia was required was significantly less in the LPG-IP group compared with the OPG-IP group (2 vs. 4, p < 0.0001).
Conclusions
LPG-IP has equivalent safety and curability compared with OPG-IP. Our results imply that LPG-IP may lead to faster recovery, better cosmesis, and improved quality of life in the short-term compared with OPG-IP. Because of the limitations of retrospective analysis, a further study should be conducted to obtain definitive conclusions.



Similar content being viewed by others
References
Kitano S, Shiraishi N, Uyama I, Sugihara K, Tanigawa N, Japanese Laparoscopic Surgery Study Group (2007) A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg 245:68–72
Tanimura S, Higashino M, Fukunaga Y, Takemura M, Tanaka Y, Fujiwara Y, Osugi H (2005) Laparoscopic gastrectomy for gastric cancer: experience with more than 600 cases. Surg Endosc 19:1177–1181
Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, Bae JM (2008) Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg 248:721–727
Japanese Gastric Cancer Association (2011) Japanese Gastric Cancer treatment guidelines 2010 (Ver. 3). Gastric Cancer 14:113–123
Takeshita K, Saito N, Saeki I, Honda T, Tani M, Kando F, Endo M (1997) Proximal gastrectomy and jejunal pouch interposition for the treatment of early cancer in the upper third of the stomach: surgical techniques and evaluation of postoperative function. Surgery 121:278–286
Yoo CH, Sohn BH, Han WK, Pae WK (2005) Proximal gastrectomy reconstructed by jejunal pouch interposition for upper third gastric cancer: prospective randomized study. World J Surg 25:1592–1599
Katai H, Sano T, Fukagawa T, Shinohara H, Sasako M (2003) Prospective study of proximal gastrectomy for early gastric cancer in the upper third of the stomach. Br J Surg 90:850–853
Sano T, Hollowood A (2006) Early gastric cancer: diagnosis and less invasive treatments. Scand J Surg 95:249–255
Dindo D, Demartines N, Clavien P (2004) Classification of surgical complications. A new proposal with evaluation in a cohort of 6336 patients and results of survey. Ann Surg 240:205–213
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma 2nd edition. Gastric Cancer 14:101–112
Kinoshita T, Oshiro T, Ito K, Shibasaki H, Okazumi S, Katoh R (2010) Intracorporeal circular-stapled esophagojejunostomy using handsewn pursestring suture after laparoscopic total gastrectomy. Surg Endosc 24:2908–2912
Uyama I, Sugioka A, Matsui H, Fujita J, Komori Y, Hatakawa Y, Hasumi A (2001) Laparoscopic side-to-side esophagogastrostomy using a linear stapler after proximal gastrectomy. Gastric Cancer 4:98–102
Sakuramoto S, Yamashita K, Kikuchi S, Futawatari N, Katada N, Moriya H, Hirai K, Watanabe M (2009) Clinical experience of laparoscopy-assisted proximal gastrectomy with Toupet-like partial fundoplication in early gastric cancer for preventing reflux esophagitis. J Am Coll Surg 209:344–351
Aihara R, Mochiki E, Ohno T, Yanai M, Toyomasu Y, Ogata K, Ando H, Asao T, Kuwano H (2010) Laparoscopy-assisted proximal gastrectomy with gastric tube reconstruction for early gastric cancer. Surg Endosc 24:2343–2348
Ichikawa D, Komatsu S, Okamoto K, Shiozaki A, Fujiwara H, Otsuji E (2012) Esophagogastrostomy using a circular stapler in laparoscopy-assisted proximal gastrectomy with an incision in the left abdomen. Langenbecks Arch Surg 397:57–62
Takeuchi H, Oyama T, Kamiya S, Nakamura R, Takahashi T, Wada N, Saikawa Y, Kitagawa Y (2011) Laparoscopy-assisted proximal gastrectomy with sentinel node mapping for early gastric cancer. World J Surg 35:2463–2471
Uyama I, Sugioka A, Fujita J, Komori Y, Matsui H, Hasumi A (2000) Completely laparoscopic proximal gastrectomy with jejunal interposition and lymphadenectomy. J Am Coll Surg 191:114–119
Ikeda Y, Sasaki Y, Niimi M, Kan S, Takami H, Kodaira S (2002) Hand-assisted laparoscopic proximal gastrectomy with jejunal interposition and lymphadenectomy. J Am Coll Surg 195:578–581
Katai H, Morita S, Saka M, Taniguchi H, Fukagawa T (2010) Long-term outcomes after proximal gastrectomy with jejunal interposition for suspected early cancer in the upper third of the stomach. Br J Surg 97:558–562
Fukagawa T, Gotoda T, Oda I, Deguchi Y, Saka M, Morita S, Katai H (2010) Stenosis of esophago-jejuno anastomosis after gastric surgery. World J Surg 34:1859–1863
Disclosures
Drs. Takahiro Kinoshita, Naoto Gotohda, Yuichiro Kato, Shinichiro Takahashi, Masaru Konishi, and Taira Kinoshita have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kinoshita, T., Gotohda, N., Kato, Y. et al. Laparoscopic proximal gastrectomy with jejunal interposition for gastric cancer in the proximal third of the stomach: a retrospective comparison with open surgery. Surg Endosc 27, 146–153 (2013). https://doi.org/10.1007/s00464-012-2401-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2401-6