Abstract
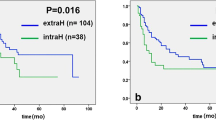
Biliary tract cancers are aggressive tumors of which the incidence seems to increase. Resection with cancer-free margins is crucial for curative therapy. However, how often biliary intraepithelial neoplasia (BilIN) occurs in resection margins and what its clinical and therapeutic implications might be is largely unknown. We reexamined margins of resection specimens of adenocarcinoma of the biliary tree including the gallbladder for the presence of BilIN. When present, it was graded. The findings were correlated with clinicopathological parameters and overall survival. Complete examination of the resection margin could be performed on 55 of 78 specimens (71 %). BilIN was detected in the margin in 29 specimens (53 %) and was mainly low-grade (BilIN-1; N = 14 of 29; 48 %). In resection specimens of extrahepatic cholangiocarcinoma, BilIN was most frequent (N = 6 of 8; 75 %). BilIN was found in the resection margin more frequently in extrahepatic cholangiocarcinomas (P = 0.007) and in large primary tumors (P = 0.001) with lymphovascular (P = 0.006) and perineural invasion (P = 0.049). Patients with cancer in the resection margin (R1) had a significantly shorter overall survival than those with resection margins free of tumor (R0) irrespective of the presence of BilIN (R0 vs R1; P < 0.001) or BilIN grade (BilIN-positive vs BilIN-negative, P = 0.6, and BilIN-1 + 2 vs BilIN-3, P = 0.58). BilIN is frequently found in the surgical margin of resection specimens of adenocarcinoma of the biliary tract. Hepatopancreatobiliary surgeons will be confronted with this recently defined entity when an intraoperative frozen section of a resection margin is requested. However, this diagnosis does not require additional resection and in the intraoperative evaluation of resection, the emphasis should remain on the detection of residual invasive tumor.


Similar content being viewed by others
References
Patel T (2006) Cholangiocarcinoma. Nat Clin Pract Gastroenterol Hepatol 3(1):33–42
Khan SA, Emadossadaty S, Ladep NG et al (2012) Rising trends in cholangiocarcinoma: is the ICD classification system misleading us? J Hepatol 56(4):848–54
Shaib Y, El-Serag HB (2004) The epidemiology of cholangiocarcinoma. Semin Liver Dis 24(2):115–25
Khan SA, Toledano MB, Taylor-Robinson SD (2008) Epidemiology, risk factors, and pathogenesis of cholangiocarcinoma. HPB 10(2):77–82
Taylor-Robinson SD, Toledano MB, Arora S et al (2001) Increase in mortality rates from intrahepatic cholangiocarcinoma in England and Wales 1968–1998. Gut 48(6):816–20
Khan SA, Taylor-Robinson SD, Toledano MB et al (2002) Changing international trends in mortality rates for liver, biliary and pancreatic tumours. J Hepatol 37(6):806–13
Schnitzbauer AA, Lang SA, Goessmann H et al (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 255(3):405–14
Jang JY, Kim SW, Park DJ et al (2005) Actual long-term outcome of extrahepatic bile duct cancer after surgical resection. Ann Surg 241(1):77–84
Sakamoto Y, Kosuge T, Shimada K et al (2005) Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery 137(4):396–402
Shingu Y, Ebata T, Nishio H et al (2010) Clinical value of additional resection of a margin-positive proximal bile duct in hilar cholangiocarcinoma. Surgery 147(1):49–56
Ribero D, Amisano M, Lo Tesoriere R et al (2011) Additional resection of an intraoperative margin-positive proximal bile duct improves survival in patients with hilar cholangiocarcinoma. Ann Surg 254(5):776–81, discussion 81–3
Zen Y, Adsay NV, Bardadin K et al (2007) Biliary intraepithelial neoplasia: an international interobserver agreement study and proposal for diagnostic criteria. Mod Pathol 20(6):701–9
Kloppel G, Adsay V, Konukiewitz B et al (2013) Precancerous lesions of the biliary tree. Best Pract Res Clin Gastroenterol 27(2):285–97
Edge SB, Byrd D, Compton CC et al (2010) AJCC cancer staging manual. Springer, New York
Bosman FT, Carneiro F, Hruban RH et al (2010) WHO classification of tumours of the digestive system
Bismuth H, Corlette MB (1975) Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet 140(2):170–8
Neuhaus P, Jonas S, Bechstein WO et al (1999) Extended resections for hilar cholangiocarcinoma. Ann Surg 230(6):808–18, discussion 19
Jarnagin WR, Fong Y, DeMatteo RP et al (2001) Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 234(4):507–17, discussion 17–9
Neuhaus P, Thelen A, Jonas S et al (2012) Oncological superiority of hilar en bloc resection for the treatment of hilar cholangiocarcinoma. Ann Surg Oncol 19(5):1602–8
Lang H, Kaiser GM, Zopf T, et al. (2006) Surgical therapy of hilar cholangiocarcinoma. Chirurg 77(4):325–34
DeOliveira ML, Cunningham SC, Cameron JL et al (2007) Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg 245(5):755–62
Sasaki R, Takeda Y, Funato O et al (2007) Significance of ductal margin status in patients undergoing surgical resection for extrahepatic cholangiocarcinoma. World J Surg 31(9):1788–96
Wakai T, Shirai Y, Moroda T et al (2005) Impact of ductal resection margin status on long-term survival in patients undergoing resection for extrahepatic cholangiocarcinoma. Cancer 103(6):1210–6
Bickenbach KA, Shia J, Klimstra DS et al (2011) High-grade dysplasia of the cystic duct margin in the absence of malignancy after cholecystectomy. HPB (Oxford) 13(12):865–8
Nakanuma Y (2010) A novel approach to biliary tract pathology based on similarities to pancreatic counterparts: is the biliary tract an incomplete pancreas? Pathol Int 60(6):419–29
Cardinale V, Wang Y, Carpino G et al (2012) The biliary tree—a reservoir of multipotent stem cells. Nat Rev Gastroenterol Hepatol 9(4):231–40
Matthaei H, Hong SM, Mayo SC et al (2011) Presence of pancreatic intraepithelial neoplasia in the pancreatic transection margin does not influence outcome in patients with R0 resected pancreatic cancer. Ann Surg Oncol 18(12):3493–9
Yamaguchi K, Shirahane K, Nakamura M et al (2005) Frozen section and permanent diagnoses of the bile duct margin in gallbladder and bile duct cancer. HPB (Oxford) 7(2):135–8
Acknowledgments
This study was supported by the BONFOR program of the Bonn University Medical Faculty.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Hanno Matthaei, Philipp Lingohr, and Anke Strässer have equal contributions.
Rights and permissions
About this article
Cite this article
Matthaei, H., Lingohr, P., Strässer, A. et al. Biliary intraepithelial neoplasia (BilIN) is frequently found in surgical margins of biliary tract cancer resection specimens but has no clinical implications. Virchows Arch 466, 133–141 (2015). https://doi.org/10.1007/s00428-014-1689-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-014-1689-0