Abstract
Background
Cognitive and emotional disorders frequently persist after recovery from the acute symptoms of COVID-19; possible explanations include pneumonia-induced hypoxia, infection of the central nervous system, and microstrokes. The objective of the present study was to characterize the impact of hypoxia on the cognitive and psychological profile following COVID-19.
Methods
Sixty-two patients with COVID-19 were enrolled in a cross-sectional study and divided into two groups based on disease severity: outpatients with no pulmonary complications vs. inpatients with hypoxemic pneumonia having received oxygen therapy. All the participants underwent a comprehensive neuropsychological evaluation that included depression, anxiety, fatigue, sleepiness, attentional, memory and executive processes, and social cognition. For the inpatients, we also collected laboratory data (blood gas, blood glucose, fibrin, fibrinogen, D-dimer, and C-reactive protein).
Results
Cognitive disorders was found in patients with COVID-19: at least 18% had an impairment of memory and 11% had attentional dysfunctions. A high level of fatigue (90% of the patients), anxiety (52%), and depression (50%) was also observed. The impairments in attentional (p < 0.001 for omission and commission in CPT 3) and memory (p < 0.003 for Index Cue Efficiency from free and cue selected reminding test) functions were greater in COVID-19 inpatients that in COVID-19 outpatients. In contrast, levels of fatigue, depression, and anxiety were similarly high in both groups.
Conclusions
These findings might help to improve the management of COVID-19 patients as a function of the disease severity in particular for patients with hypoxia.
Similar content being viewed by others
Background
Coronavirus disease 2019 [COVID-19, induced by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)] is characterized by a number of now well-identified signs and symptoms in its acute phase: fever, cough, shortness of breath, and (in some cases) acute respiratory distress. Along with pneumonia, neurological manifestations are typically observed in more than 70% of hospitalized patients; these mainly including headache, myalgia, and an altered state of consciousness [1, 2]. Other studies have also shown that COVID-19 accentuates the signs and symptoms of neurodegenerative diseases like Alzheimer's disease and Parkinson's disease [3]. Moreover, additional symptoms described long after disease onset (such as anosmia, ageusia, cognitive disorders, fatigue, sleep disorders, pain, and paraesthesia) may reflect neurological damage caused by the virus [4, 5] and have prompted the concept of long COVID-19. A PET-based study highlighted abnormally low baseline metabolism in the olfactory gyrus and the frontal, limbic, and paralimbic regions in patients with severe COVID-19 3 weeks after theSARS-CoV-2 infection [6].
The presence of cognitive disorders long after infection has also been described. It is well known that cognitive impairment is frequent in patients admitted to the ICU for various indications [7,8,9]. A number of infectious diseases (such as AIDS or lethargic encephalitis) can also induce cognitive impairment. However, cognitive impairment has notably been observed in patients with mild-to-moderate COVID-19 and appears to persist long after the onset of COVID-19 [10].
A recent review evidenced cognitive impairments in attentional, executive, and memory functions shortly after COVID-19 [11]. More precisely, Zhou et al. [12] found impairments in attentional functions in patients who had recovered from COVID-19 (i.e., with negative PCR tests). However, the researchers did not report on the severity of these impairments. Jaywant et al. [13] showed that 81% of patients with a severe form of COVID-19 (77% had been intubated for a mean duration of 13 days) had a cognitive impairment, although the latter might have resulted from the care received in the intensive care unit (ICU) [14, 15]. Woo et al. [10] found long-term impairments of attentional and memory functions in young patients with mild-to-moderate COVID-19. Almaria et al. [16] did not observe marked cognitive impairments in 35 patients (with mild-to-severe COVID-19) soon after hospital discharge. However, patients who had received oxygen therapy had more severe impairments in attentional, memory, and executive functions. These results suggest that lung-disease-induced hypoxia is linked to the severity of the cognitive impairment observed in some COVID-19 patients.
The known relationship between SARS-CoV-2 infection and changes in the brain suggests that the virus has a long-term impact on brain structures and functions [17]. This damage might be caused indirectly through various pathophysiological mechanisms (such as neuroinflammation and microstrokes) or directly through hypoxia [18, 19]. It has also been suggesting that SARS-CoV-2 can infect cells in the brain. However, it is well known that hypoxia can damage the brain, which possibly induces cognitive disorders [20, 21]. Here, we studied the cognitive and emotional profiles of COVID-19 patients 3–9 months after SARS-CoV-2 infection. We compared COVID-19 inpatients with a history of hypoxemia (attested to by admission to an ICU) with pneumonia-free COVID-19 outpatients. Our starting hypothesis was that patients having required oxygen therapy would have greater cognitive impairments in general and greater memory and attentional impairments in particular.
Method
Study design
Patients with suspected COVID-19 were prospectively enrolled between September 2020 and December 2021 after referral by an infectious disease physician at Lille University Hospital’s outpatient clinic for infectious diseases (Lille, France). Sixty-two patients (age range: 27–64; 37 females) were recruited 3–9 months after symptom onset. The main inclusion criteria were (i) age 18–65, (ii) a diagnosis of COVID-19 confirmed by a positive PCR test and/or a positive serology test, and (iii) subjective cognitive complaints that exerted a significant impact on activities of daily living. The main exclusion criteria were (i) severe pneumonia following COVID-19 (i.e., with intubation and sedation), (ii) the presence of asthma, unstable coronary heart disease, uncontrolled diabetes or hypertension, encephalitis, or epilepsy; (iii) a history of head injury or a brain tumor; (iv) the presence of a major psychiatric condition before the infection by SARS-CoV-2 (based on the patient’s medical records); (v) dementia (according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), (vi) insufficient understanding of the French language, and (vii) illiteracy.
All patients were offered a follow-up consultation with the infectious disease physician 3–9 months after the acute signs and symptoms of COVID-19 had resolved. The consultation lasted around 90 min, and included a comprehensive neuropsychological and psychiatric assessment. Clinical data on the sign and symptoms of COVID-19 and blood test results were also collected. Data on demographics, psychiatric and cardiovascular comorbidities, symptoms at COVID-19 onset, and treatments received were compiled on the basis of the medical records and the patient interview. We divided the COVID-19 patients into two groups: patients hospitalized for pneumonia and having received oxygen therapy (henceforth the “O2 + ” group), and pneumonia-free outpatient COVID-19 patients not having received oxygen therapy (henceforth the “O2 − ” group). The study was approved by the independent ethics committee. Furthermore, the study also complied with good clinical practice guidelines, the Declaration of Helsinki, and local legislation.
Neuropsychologic tests
An extensive battery of neuropsychological tests (broadly classified into four cognitive domains: executive function, attention, memory, and emotion) was administered to the patients. The memory assessment included a free and cued selective reminding test (FCSRT, French version) [22], with an evaluation of free recall (FR, the cumulative sum of free recall from the three first trials; range: 0–48), total recall (TR; the cumulative sum of free recall + cued recall from the three trials; range: 0–48), index cue efficiency (ICE, total recall-free recall/48-free recall, range: 0–100), delayed free recall (DFR, range: 0–16), and delayed total recall (DTR, range: 0–16). The Wechsler digit span task was used to examine verbal short term and working memory [23]. Processing speed and attention were evaluated using the digit symbol coding subtest of WAIS 4 (DSCT) [23] and the Continuous Performance Test (third edition, CPT3) [24].Several scores were computed from the CPT 3: detectability (DPR), omission (OMI, in%), commission (COM, in %), perseveration (PRS, in %), hit reaction time (HRT, in ms,), variability (VAR, in ms), hit reaction time block change (BLKCH, in ms), and hit reaction time interstimulus interval change (ISICH, in ms). The categorical and literal fluency test (Cardebat et al., 1990) and the Trail-Making Test (TMT) [21] were used to assess executive functions. Social cognition were evaluated via emotional facial recognition with the mini social cognition and emotional assessment (MINI-SEA) [26].
For each patient, we used published norms (corrected for age, sex, and education level) to calculate test-specific T scores [27,28,29]. For most of the tests, a pathological T-score was defined as a value of 35 or less, which corresponds to 1.5 standard deviations). For CPT 3 (with the exception of the HRT), we followed the guidelines defined by the test’s developers [24]; a pathological T-score was defined as a value of 60 or more. For the HRT, a pathological T-score was defined as a value of 40 or less (atypical slowness) or 60 or more (atypical rapidity).
Depression, anxiety, fatigue, and sleepiness assessments
Depression was rated on the Center for Epidemiologic Studies Depression Scale (CES-D) [30], with a pathological cut-off of 17 for men and 23 for women. Anxiety was assessed on the Hamilton Anxiety Rating Scale (HAM-A) [31]: a score of 20 or more corresponds to moderate or severe anxiety. Fatigue was assessed on the Chalder Fatigue Scale [32]: a score of 6 or more corresponds to significant fatigue. Sleepiness and the impact of sleep disorders were assessed on the Epworth Sleepiness Scale [33]: a score of 10 or more corresponds to excessive daytime sleepiness.
Blood samples
Blood samples were collected when participants in the O2 + group were admitted to the emergency unit: we recorded the results for blood gases while breathing ambient air (bicarbonate, partial pressure of oxygen, partial pressure of carbon dioxide, and oxygen saturation), blood glucose, and serum levels of C-reactive protein (CRP), fibrinogen, ferritin, and D-Dimer. We also recorded collected ambient air oxygen saturation upon admission to the emergency unit.
Statistical analysis
Depending on the nature of the variable, sociodemographic data were compared by applying a parametric Student’s t test for independent samples (O2 − versus O2 +) or a χ2 test.
Depending of the nature of the outcome, generalized linear models (GLMs) were fitted according to a Gaussian, Poisson, or gamma distribution. Interaction terms were not included, to determine the overall effect of the clinical COVID-19 outcomes (pneumonia with oxygen therapy, or no pneumonia) on cognition and behavioral variables while controlling for covariates [including age, the level of depression (using CES-D scores)] and the level of anxiety (using HAM-A scores). Variables with missing data were omitted, and the remaining data were analyzed. Statistical analyses were performed using R [34] and R Studio software [35] (http://www.rstudio.com/, version 1.1.463). The threshold for statistical significance was set to p < 0.05.
Results
Demographic and clinical characteristics
The groups differed significantly in age (t = 3.30, p = 0.001) (Table 1). Overall, 50% of patients reported dysgeusia, 55% reported anosmia, 45% reported headache, 16% were taking psychotropic medication at the time of the neuropsychological assessment (4 on antidepressants, 2 on benzodiazepine, and 2 on hypnotics), and 25% were taking medication for hypertension, dyslipidaemia, or heart failure.
The blood gas results evidenced hypoxia on admission to hospital, and high CRP level evidenced inflammation. The serum levels of ferritin, fibrinogen and D-Dimer were also abnormally high (Table 2).
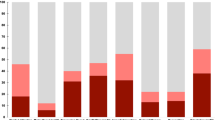
The proportion of patients with cognitive impairment, by test
Overall, we observed pathological scores (T-score > 35) for the FCSRT results (first FR (n = 14, 23%), second FR (n = 11, 18%), third FR (n = 15, 24%), and delayed FR (n = 14, 23%)), the Wechsler Digit Span Task (n = 7, 11%), the TMT part B (n = 1, 2%), phonemic fluency (n = 6, 6%), semantic fluency (n = 6, 9%), the DSCT (n = 3, 5%) and the CPT3scores (DPR (n = 17, 16%), OMI (n = 8, 13%), COM (n = 21, 34%), PRS (n = 8, 13%), HRT (n = 8; 13%), VAR (n = 7, 11%), BLKCH (n = 7, 11%), and ISICH (n = 11, 18%)). Overall, 50% of the patients were depressed, 52%had a high level of anxiety, 90% experienced an abnormally high level of fatigue, and 24% had excessive daytime sleepiness (Table 3).
Neuropsychological and psychiatric assessments
Patients in the O2 + group had lower scores for the ICE (z = − 2.23, p = 0.03, with no effect of age, the HAM-A score or the CES-D scores) than patients in the O2 − group. In the attentional assessments, the two groups differed significantly with regard to the DPR (z = 2.3, p = 0.02). The commission rate was higher in theO2 + group (z = 5.75, p < 0.001, with significant effects of age (z = − 6.41, p < 0.001) and the HAM-A score (z = 2.63, p = 0.009); there was also a significant effect of the interaction between age, the HAM-A score, and group (z = 2.35, p = 0.02). The omission rate was higher in the O2 + group (z = 3.52, p < 0.001), with a significant effect of age (z = − 6.41, p < 0.001) and the HAM-A score (z = 1.96, p < 0.001) but no effect of an interaction between the HAM-A score and group (z = − 1.24, p = 0.22). The mean reaction time was longer in the O- group(z = − 5.91, p < 0.001), with a significant effect of age (z = 8.67, p < 0.001), the CES-D scores (z = − 2.23, p = 0.03) and HAM-A score (z = 3.18, p = 0.001), and an effect of the interaction between age, HAM-A scores, CES-D scores, and group (z = − 2.20, p = 0.03). There were no significant intergroup differences in depression, anxiety, fatigue, or sleepiness scores (Table 4).
Discussion
The objective of the present study was to determine the psychological and neuropsychological profiles of hospitalized patients having received oxygen therapy (mean duration: 4 days) for COVID-19 pneumonia (the O2 + group) vs. outpatients without pneumonia (the O2 − group). The blood test results confirmed the presence of hypoxia and marked damage to the lungs. We studied patients with cognitive complaints after COVID-19, who account for only a small proportion of COVID-19 patients overall. However, our focus on this subset highlighted (i) the presence of significant cognitive and psychiatric disorders, and (ii) a clear effect of lung damage on the severity of the cognitive disorders.
In line with the literature data, we found that 90% of the study participants had significant fatigue [36]. Nevertheless, we did not observe significant differences in fatigue between the O2 + and O2 − groups; the state of hypoxia did not appear to impact the level of fatigue experienced by the patients. Twenty-four percent of the patients reported daytime sleepiness, which confirmed the impact of fatigue on activities of daily living. In our study, fatigue was the most frequently reported and most disabling symptom for patients with COVID-19, with no difference between the O2 + and O2 − groups.
With regard to anxiety and depression, almost 50% of the patients had a high CES-Dscore. There was no difference between the O2 + and O2 − groups. This result is consistent with the literature data [37]. Furthermore, 54% of the patients reported significant anxiety; again, this result is in line with the literature. These anxiety-depressive disorders might be related to the trauma associated with the disease and (in some cases) hospitalization [38].
Neuropsychological disorders (and particularly attentional and memory functions) affected a large proportion of the study participants. According to the CPT3, nearly 13% of the participants had a pathological omission rate and 34% had a pathological error rate. These results are concordant with Zhou et al.’s (2020) report in a heterogeneous patient population. Our study participants also suffered from memory disorders. Indeed, almost 18% had a pathological score in at least one of the first three free recall tasks, and 23% had a pathological score in the delayed free recall task. These results are consistent with Garcia-Sanchez et al.’s report [39] of attentional and memory impairments in a group of 84 consecutive patients. In contrast, few of our patients had executive function disorders.
We observed greater memory impairment in the O2 + group, with notably a significant difference for the cue efficiency index and the total recall, which shows that semantic indexing does not help in the retrieval of memory information which is considered to reflect hippocampal damage [22, 40]. Patients in the O2 + group showed psychomotor slowing with attentional disorders, relative to patients in the O2 − group. The significant hypoxia related to COVID-19 pneumonia might explain (at least in part) the observed cognitive impairment. Hypoxia-related memory and attentional impairments have already been described in other disease states (influenza, pulmonary bacterial infections, and severe asthma) [21]. Our study results are in line with the literature data. We also highlighted cognitive and psychiatric impairments specifically related to COVID-19 among patients in the O2 − group.
The present study had a number of limitations. First, the sample size was small. Second, the patients in the O2 + group were older than those in the O2 − group. Third, for patients in the O2 − group, we did not have data on PCR tests and blood tests performed at the time of infection; these data might have allowed us to compare indicators of inflammation and to better clarify the relationship between inflammation and cognitive impairments.
In conclusion, our study evidenced cognitive impairment in nearly a quarter of patients 4 months after the onset of COVID-19. Psychiatric disorders were also frequent, with significant fatigue, daytime sleepiness, anxiety, and depression observed in more than half of the patients. More specifically, a particular cognitive profile (with a decrease in memory capacity, due perhaps to hippocampal damage and psychomotor slowing) was observed in COVID-19 patients in the O2 + group. Future studies with neuroimaging might reveal the nature of the brain damage and the relationship with the observed cognitive and psychiatric disorders. Our results also provide perspectives for the specific management of patients as a function of the severity of COVID-19.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- CES-D:
-
Center for Epidemiologic Studies Depression Scale
- FCSRT:
-
Free and cued selective reminding test
- FR:
-
Free recall
- TR:
-
Total recall
- ICE:
-
Index cue efficiency
- DFR:
-
Delayed free recall
- DTR:
-
Delayed total recall
- CPT3:
-
Continuous performance test third edition
- DPR:
-
Detectability
- OMI:
-
Omission
- COM:
-
Commission
- PRS:
-
Perseveration
- HRT:
-
Hit reaction time
- VAR:
-
Variability
- BLKCH:
-
Hit reaction time block change
- ISICH:
-
Hit reaction time interstimulus interval change
- TMT:
-
Trail making test
- O2 − :
-
COVID-19 patients not having received oxygen therapy
- O2 + :
-
COVID-19 patients having received oxygen therapy
References
Maury A, Lyoubi A, Peiffer-Smadja N et al (2021) Neurological manifestations associated with SARS-CoV-2 and other coronaviruses: a narrative review for clinicians. Rev Neurol (Paris) 177:51–64
Premraj L, Kannapadi NV, Briggs J et al (2022) Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis. J Neurol Sci
Erausquin GA, Snyder H, Carrillo M et al (2021) The chronic neuropsychiatric sequelae of COVID-19: the need for a prospective study of viral impact on brain functioning. Alzheimers Dement 17:1056–1065
Liguori C, Pierantozzi M, Spanetta M et al (2020) Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection. Brain Behav Immun 88:11–16
Niazkar HR, Zibaee B, Nasimi A et al (2020) The neurological manifestations of COVID-19: a review article. Neurol Sci 41:1667–1671
Hosp JA, Dressing A, Blazhenets G et al (2021) Cognitive impairment and altered cerebral glucose metabolism in the subacute stage of COVID-19. Brain 144:1263–1276
Beaud V, Crottaz-Herbette S, Dunet V et al (2021) Pattern of cognitive deficits in severe COVID-19. J Neurol Neurosurg Psychiatry 92:567–568
Pandharipande PP, Girard TD, Jackson JC et al (2013) Long-term cognitive impairment after critical illness. N Engl J Med 369:1306–1316
Rengel KF, Hayhurst CJ, Pandharipande PP et al (2019) Long-term cognitive and functional impairments after critical illness. Anesth Analg 128:772–780
Woo MS, Malsy J, Pöttgen J et al (2020) Frequent neurocognitive deficits after recovery from mild COVID-19. Brain Commun 2: 205
Vanderlind WM, Rabinovitz BB, Miao IY et al (2021) A systematic review of neuropsychological and psychiatric sequalae of COVID-19: implications for treatment. Curr Opin Psychiatry 34:420–433
Zhou H, Lu S, Chen J et al (2020) The landscape of cognitive function in recovered COVID-19 patients. J Psychiatr Res 129:98–102
Jaywant A, Vanderlind WM, Alexopoulos GS et al (2021) Frequency and profile of objective cognitive deficits in hospitalized patients recovering from COVID-19. Neuropsychopharmacology [Internet]. 2021 [cited 2021 Aug 15]. Available from http://www.nature.com/articles/s41386-021-00978-8.
Widmann CN, Heneka MT (2014) Long-term cerebral consequences of sepsis. Lancet Neurol 13:630–636
Hopkins RO, Jackson JC (2006) Long-term neurocognitive function after critical illness. Chest 130:869–878
Almeria M, Cejudo JC, Sotoca J et al (2020) Cognitive profile following COVID-19 infection: clinical predictors leading to neuropsychological impairment. Brain Behav Immun Health 9:100163
Boldrini M, Canoll PD, Klein RS (2021) How COVID-19 affects the brain. JAMA Psychiat 78:682
Song E, Zhang C, Israelow B et al (2021) Neuroinvasion of SARS-CoV-2 in human and mouse brain. J Exp Med 218:e20202135
Solomon T (2021) Neurological infection with SARS-CoV-2—the story so far. Nat Rev Neurol 17:65–66
Lanteaume L, Cassé-Perrot C, Lefebvre M-N et al (2016) Neurobehavioral and cognitive changes induced by hypoxia in healthy volunteers. CNS Neurol Disord Drug Targets Former Curr Drug Targets 15:816–822
Sasannejad C, Ely EW, Lahiri S (2019) Long-term cognitive impairment after acute respiratory distress syndrome: a review of clinical impact and pathophysiological mechanisms. Crit Care [Internet] [cited 2021 Jul 9]. Available from https://doi.org/10.1186/s13054-019-2626-z
Grober E, Merling A, Heimlich T et al (1997) Free and cued selective reminding and selective reminding in the elderly. J Clin Exp Neuropsychol 19:643–654
Wechsler D (2008) Wechsler adult intelligence scale–fourth edition (WAIS–IV), vol 22. NCS Pearson, San Antonio, TX, pp 816–827
Conners CK, Sitarenios G (2011) Conners’ continuous performance test (CPT). In: Kreutzer JS, DeLuca J, Caplan B (eds) Encycl Clin Neuropsychol [Internet]. Springer, New York; [cited 2021 Aug 29], pp 681–683. Available from https://doi.org/10.1007/978-0-387-79948-3_1535.
Tombaugh TN (2004) Trail making test A and B: normative data stratified by age and education. Arch Clin Neuropsychol 19:203–214
Funkiewiez A, Bertoux M, de Souza LC et al (2012) The SEA (Social Cognition and Emotional Assessment): a clinical neuropsychological tool for early diagnosis of frontal variant of frontotemporal lobar degeneration. Neuropsychology 26:81
Boccardi M, Monsch AU, Ferrari C et al (2021) Harmonizing neuropsychological assessment for mild neurocognitive disorders in Europe. Alzheimers Dement alz.12365
Griffith LE, van den Heuvel E, Raina P et al (2016) Comparison of standardization methods for the harmonization of phenotype data: an application to cognitive measures. Am J Epidemiol 184:770–778
Becker JH, Lin JJ, Doernberg M et al (2021) Assessment of cognitive function in patients after COVID-19 infection. JAMA Netw Open 4:e2130645–e2130645
Radloff LS (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32:50–55
Jackson C (2015) The Chalder fatigue scale (CFQ 11). Occup Med 65:86–86
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14: 540–545
Team RC (2013) R: a language and environment for statistical computing
Team Rs (2020) RStudio: integrated development for R. RStudio. PBC, Boston, MA
Townsend L, Dyer AH, Jones K, et al. (2020) Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLOS One 15: e0240784
Kumar S, Veldhuis A, Malhotra T (2021) Neuropsychiatric and cognitive sequelae of COVID-19. Front Psychol 12:577529
Tarsitani L, Vassalini P, Koukopoulos A et al (2021) Post-traumatic stress disorder among COVID-19 survivors at 3-month follow-up after hospital discharge. J Gen Intern Med 36:1702–1707
García‐Sánchez C, Calabria M, Grunden N et al (2022) Neuropsychological deficits in patients with cognitive complaints after COVID‐19. Brain Behav [Internet]. [cited 2022 Feb 11]. Available from https://doi.org/10.1002/brb3.2508
Traykov L, Baudic S, Raoux N et al (2005) Patterns of memory impairment and perseverative behavior discriminate early Alzheimer’s disease from subcortical vascular dementia. J Neurol Sci 229–230:75–79
Acknowledgements
The authors would like to thank the team of infectious unit of CHU for help in collecting the data and Dr. David Fraser (Biotech Communication, France) for editing the article.
Funding
The authors have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article. The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
TD, DD, and RB are the guarantors of this article. TD: contributed to study design, data acquisition, statistical analysis, and interpretation; wrote the first draft of the manuscript; and revised it following critical reviews by the co-authors. FR: contributed to data acquisition and interpretation and critically reviewed the manuscript. FV: contributed to the referral of patients with COVID-19 and critically reviewed the manuscript. LC: contributed to data interpretation and critically reviewed the manuscript. PG: contributed to data acquisition and interpretation and critically reviewed the manuscript. KF: contributed to the referral of patients with COVID-19 and critically reviewed the manuscript. DD: contributed to study design, study coordination, and fundraising, and critically reviewed the manuscript. RB: contributed to study design, study coordination, and fundraising, and critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
All participants consented to the retrospective analysis of their anonymized personal data.
Consent for publication
All participants consented to the publication of their anonymized personal data.
Rights and permissions
About this article
Cite this article
Dondaine, T., Ruthmann, F., Vuotto, F. et al. Long-term cognitive impairments following COVID-19: a possible impact of hypoxia. J Neurol 269, 3982–3989 (2022). https://doi.org/10.1007/s00415-022-11077-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11077-z