Abstract
Purpose
For the prevention of nutritional rickets, 400 IU vitamin D daily and circulating 25-hydroxyvitamin D (25OHD) concentrations > 50 nmol/L are recommended, whereas the toxicity threshold is set at 250 nmol/L. We synthesized the evidence for the effect of vitamin D supplementation on incremental 25OHD in infants up to 1 year of age.
Methods
We performed a systematic review and meta-analysis of intervention trials in several databases. A total of 87 records were identified for full-text review and 27 articles with 61 studies were included in the final analysis.
Results
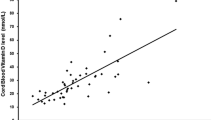
The selected 61 studies included 1828 participants. Nineteen cohorts had already mean baseline 25OHD levels ≥ 50 nmol/L. The weighted mean difference in 25OHD following vitamin D supplementation was + 49.4 nmol/L (95% CI 43.6–55.3 nmol/L; P < 0.001). The increment was dose-dependent (P = 0.002), was higher in full-term than in pre-term infants (P < 0.001), was higher in infants with baseline 25OHD < 50 nmol/L as compared to ≥ 50 nmol/L (P = 0.001), and was marginally influenced by the 25OHD test procedure (P = 0.080). Vitamin D3 doses of 400 IU/day were sufficient to achieve 25OHD concentrations ≥ 50 nmol/L in most full-term infants. A 25OHD level of 250 nmol/L was not exceeded in ≥ 97.5% of infants at doses between 200 and 1200 IU/day, but potentially in ≥ 2.5% of infants at a dose of 1600 IU/day.
Conclusions
Vitamin D supplementation of 400 IU/day is sufficient for achieving 25OHD concentrations able to prevent nutritional rickets. A more personalized vitamin D dosing strategy would require 25OHD testing, but also assay standardization.




Similar content being viewed by others
References
Rajakumar K (2003) Vitamin D, cod-liver oil, sunlight, and rickets: a historical perspective. Pediatrics 112:e132–e135
Holick MF (2012) The D-lightful vitamin D for child health. J Parenter Enteral Nutr 36:9S–19S
Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, Michigami T, Tiosano D, Mughal MZ, Mäkitie O, Ramos-Abad L, Ward L, DiMeglio LA, Atapattu N, Cassinelli H, Braegger C, Pettifor JM, Seth A, Idris HW, Bhatia V, Fu J, Goldberg G, Sävendahl L, Khadgawat R, Pludowski P, Maddock J, Hyppönen E, Oduwole A, Frew E, Aguiar M, Tulchinsky T, Butler G, Högler W (2016) Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab 101:394–415
Uday S, Kongjonaj A, Aguiar M, Tulchinsky T, Högler W (2017) Variations in infant and childhood vitamin D supplementation programmes across Europe and factors influencing adherence. Endocr Connect 6:667–675
Ahrens KA, Rossen LM, Simon AE (2016) Adherence to vitamin D recommendations among US infants aged 0 to 11 Months, NHANES, 2009 to 2012. Clin Pediatr 55:555–556
Weisberg P, Scanlon KS, Li R, Cogswell ME (2004) Nutritional rickets among children in the United States: review of cases reported between 1986 and 2003. Am J Clin Nutr 80:1697S–1705S
Creo AL, Thacher TD, Pettifor JM, Strand MA, Fischer PR (2017) Nutritional rickets around the world: an update. Paediatr Int Child Health 37:84–98
Uday S, Högler W (2018) Prevention of rickets and osteomalacia in the UK: political action overdue. Arch Dis Child 103:901–906
Dagnelie PC, Vergote FJ, van Staveren WA, van den Berg H, Dingjan PG, Hautvast JG (1990) High prevalence of rickets in infants on macrobiotic diets. Am J Clin Nutr 51:202–208
IOM (Institute of Medicine) (2011) Dietary reference intakes for calcium and vitamin D. The National Academies Press, Washington, DC
European Food Safety Authority (2016) Scientific opinion on dietary reference values for vitamin D. EFSA J 14:2813
European Food Safety Authority (2018) Scientific opinion on the tolerable upper intake level of vitamin D. EFSA J 16:5365
Deutsche Gesellschaft für Ernährung, Österreichische Gesellschaft für Ernährung, Schweizerische Gesellschaft für Ernährungsforschung, and Schweizerische Vereinigung für Ernährung, Referenzwerte für die nährstoffzufuhr, Neuer Umschau Buchverlag, 1. Aufl Neustadt an der Weinstraße (2013) (5. Korrigierter Nachdruck) (in German)
Vidailhet M, Mallet E, Bocquet A, Bresson JL, Briend A, Chouraqui JP, Darmaun D, Dupont C, Frelut ML, Ghisolfi J, Girardet JP, Goulet O, Hankard R, Rieu D, Simeoni U, Turck D, Comité de nutrition de la Société française de pédiatrie (2012) Vitamin D: still a topical matter in children and adolescents. A position paper by the Committee on Nutrition of the French Society of Paediatrics. Arch Pediatr 19:316–328
Pettifor JM (2005) Vitamin D deficiency and nutritional rickets in children. In: Vitamin D, Feldman D, Pike JW, Glorieux FH (eds), pp 1065–1083, Elsevier Academic Press, San Diego
Spiro A, Buttriss JL (2014) Vitamin D: An overview of vitamin D status and intake in Europe. Nutr Bull 39:322–350
Thorisdottir B, Gunnarsdottir I, Steingrimsdottir L, Palsson GI, Thorsdottir I (2014) Vitamin D intake and status in 12-month-old infants at 63–66°N. Nutrients 6:1182–1193
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283:2008–2012
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539 – 1558
Macaskill P, Walter SD, Irwig L (2001) A comparison of methods to detect publication bias in meta-analysis. Stat Med 20:641–654
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Valkama S, Holmlund-Suila E, Enlund-Cerullo M, Rosendahl J, Hauta-Alus H, Helve O, Hytinantti T, Viljakainen H, Andersson S, Mäkitie O (2017) No severe hypercalcemia with daily vitamin D3 supplementation of up to 30 µg during the first year of life. Horm Res Paediatr 88:147–154
Ponnapakkam T, Bradford E, Gensure R (2010) A treatment trial of vitamin D supplementation in breast-fed infants: universal supplementation is not necessary for rickets prevention in Southern Louisiana. Clin Pediatr 49:1053–1060
Gallo S, Comeau K, Agellon S, Vanstone C, Sharma A, Jones G, L’abbé M, Khamessan A, Weiler H, Rodd C (2014) Methodological issues in assessing plasma 25-hydroxyvitamin D concentration in newborn infants. Bone 61:186–190
Gallo S, Comeau K, Vanstone C, Agellon S, Sharma A, Jones G, L’Abbé M, Khamessan A, Rodd C, Weiler H (2013) Effect of different dosages of oral vitamin D supplementation on vitamin D status in healthy, breastfed infants: a randomized trial. JAMA 309:1785–1792
Schlingmann KP, Kaufmann M, Weber S, Irwin A, Goos C, John U, Misselwitz J, Klaus G, Kuwertz-Bröking E, Fehrenbach H, Wingen AM, Güran T, Hoenderop JG, Bindels RJ, Prosser DE, Jones G, Konrad M (2011) Mutations in CYP24A1 and idiopathic infantile hypercalcemia. N Engl J Med 365:410–421
Pronicka E, Ciara E, Halat P, Janiec A, Wójcik M, Rowińska E, Rokicki D, Płudowski P, Wojciechowska E, Wierzbicka A, Książyk JB, Jacoszek A, Konrad M, Schlingmann KP, Litwin M (2017) Biallelic mutations in CYP24A1 or SLC34A1 as a cause of infantile idiopathic hypercalcemia (IIH) with vitamin D hypersensitivity: molecular study of 11 historical IIH cases. J Appl Genet 58:349–353
Hyppönen E, Sovio U, Wjst M, Patel S, Pekkanen J, Hartikainen AL, Järvelinb MR (2004) Infant vitamin D supplementation and allergic conditions in adulthood: Northern Finland birth cohort 1966. Ann NY Acad Sci 1037:84–95
Zittermann A, Ernst JB, Gummert JF, Börgermann J (2014) Vitamin D supplementation, body weight and human serum 25-hydroxyvitamin D response: a systematic review. Eur J Nutr 53:367–374
Thiele DK, Ralph J, El-Masri M, Anderson CM (2017) Vitamin D3 Supplementation during pregnancy and lactation improves vitamin D status of the mother-infant dyad. J Obstet Gynecol Neonatal Nurs 46:135–147
O’Callaghan KM, Hennessy A, Hull GLJ, Healy K, Ritz C, Kenny LC, Cashman KD, Kiely ME (2018) Estimation of the maternal vitamin D intake that maintains circulating 25-hydroxyvitamin D in late gestation at a concentration sufficient to keep umbilical cord sera ≥ 25–30 nmol/L: a dose-response, double-blind, randomized placebo-controlled trial in pregnant women at northern latitude. Am J Clin Nutr 108:77–91
Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, Domellöf M, Embleton ND, Fusch C, Genzel-Boroviczeny O, Goulet O, Kalhan SC, Kolacek S, Koletzko B, Lapillonne A, Mihatsch W, Moreno L, Neu J, Poindexter B, Puntis J, Putet G, Rigo J, Riskin A, Salle B, Sauer P, Shamir R, Szajewska H, Thureen P, Turck D, van Goudoever JB, Ziegler EE, ESPGHAN Committee on Nutrition (2010) Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr 50:85–91
Abrams SA, Committee on Nutrition (2013) Calcium and vitamin d requirements of enterally fed preterm infants. Pediatrics 131:e1676–e1683
World Health Organization (2011) Guidelines on optimal feeding of low birth-weight infants in low- and middle-income countries. http://www.who.int/maternal_child_adolescent/documents/infant_feeding_low_bw/en/. Accessed 22 Feb 2018
Anderson-Berry A, Thoene M, Wagner J, Lyden E, Jones G, Kaufmann M, Van Ormer M, Hanson C (2017) Randomized trial of two doses of vitamin D3 in preterm infants < 32 weeks: Dose impact on achieving desired serum 25(OH)D3 in a NICU population. PLoS One 12:e0185950
Pieltain C, de Halleux V, Senterre T, Rigo J (2013) Prematurity and bone health. World Rev Nutr Diet 106:181–188
De Curtis M, Vetrano G (1986) Absorption of proteins, carbohydrates and fats in the preterm neonate. Pediatr Med Chir 8:437–442 (in Italian)
Abitbol CL, DeFreitas MJ, Strauss J (2016) Assessment of kidney function in preterm infants: lifelong implications. Pediatr Nephrol 31:2213–2222
Gallo S, Phan A, Vanstone CA, Rodd C, Weiler HA (2013) The change in plasma 25-hydroxyvitamin D did not differ between breast-fed infants that received a daily supplement of ergocalciferol or cholecalciferol for 3 months. J Nutr 143:148–153
Durazo-Arvizu RA, Tian L, Brooks SPJ, Sarafin K, Cashman KD, Kiely M, Merkel J, Myers GL, Coates PM, Sempos CT (2017) The vitamin D standardization program (VDSP) manual for retrospective laboratory standardization of serum 25-hydroxyvitamin D data. J AOAC Int 100:1234–1243
Funding
None.
Author information
Authors and Affiliations
Contributions
AZ designed the study. AZ and HKB analyzed the data. ÁZ, SP, and HKB interpreted the data. AZ draft the manuscript. SP and HKB participated in the writing and critical revision of the manuscript. AZ, SP, and HKB read and approved the version of the manuscript being submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zittermann, A., Pilz, S. & Berthold, H.K. Serum 25-hydroxyvitamin D response to vitamin D supplementation in infants: a systematic review and meta-analysis of clinical intervention trials. Eur J Nutr 59, 359–369 (2020). https://doi.org/10.1007/s00394-019-01912-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-019-01912-x