Abstract
Aim
To evaluate the reason for failure of STARR (stapled transanal rectal resection) operation for obstructed defecation.
Methods
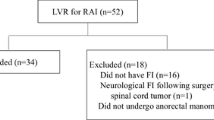
A retrospective study (June 2012–December 2017) was performed using a prospectively maintained database of patients who underwent STARR operation for ODS (obstructed defecation syndrome), complaining of persisting or de novo occurrence of pelvic floor dysfunctions. Postoperative St Mark’s and ODS scores were evaluated. A VAS was used to score pelvic pain. Patients’ satisfaction was estimated administering the CPGAS (clinical patient grading assessment scale) questionnaire. Objective evaluation was performed by dynamic proctography and anorectal manometry.
Results
Ninety patients (83.3% females) operated for ODS using STARR technique were evaluated.
Median ODS score was 19 while 20 patients (22%) reported de novo fecal urgency and 4 patients a worsening of their preoperative fecal incontinence.
Dynamic proctography performed in 54/90 patients showed a significant (> 3.0 cm) rectocele in 19 patients, recto-rectal intussusception in 10 patients incomplete emptying in 24 patients. When compared with internal normal standards, anorectal manometry showed decreased rectal compliance and maximum tolerable volume in patients with urgency. Nine patients reported a persistent postoperative pelvic pain (median VAS score 6).
Conclusion
Failure of STARR to treat ODS, documented by persisting ODS symptoms, fecal urgency, or chronic pelvic pain, is often justified by the persistence or de novo onset of alteration of the anorectal anatomy at defecation. This occurs in about half of the patients, but in 40% of the cases who complained of incomplete emptying or incontinence, anatomical abnormalities were not recognized.



Similar content being viewed by others
References
Podzemny V, Pescatori LC, Pescatori M (2015) Management of obstructed defecation. World J Gastroenterol 21:1053–1060
Tsar’komhtv PV, Sandrikov VA, Tulina IA et al (2012) Surgical treatment of rectocele with the use of mesh implants by the obstructive defecation syndrome. Khirurgiia (Mosk) 8:25–33
Karlbom U, Nilsson S, Pahlman L et al (1999) Defecographic study of rectal evacuation in constipated patients and control subjects. Radiology 210:103–108
Pescatori M, Spyrou M, Pulvirenti d’Urso A (2007) A prospective evaluation of occult disorders in obstructed defecation using the ‘iceberg diagram’. Color Dis 9:452–456
Zehler O, Vashist YK, Bogoevski D et al (2010) Quo vadis STARR? A prospective long-term follow-up of stapled transanal rectal resection for obstructed defecation syndrome. J Gastrointest Surg 14:1349–1354
Schwandner O, Furst A, German SRSG (2010) Assessing the safety, effectiveness, and quality of life after the STARR procedure for obstructed defecation: results of the German STARR registry. Langenbeck's Arch Surg 395:505–513
Pomerri F, Zuliani M, Mazza C et al (2001) Defecographic measurements of rectal intussusception and prolapse in patients and in asymptomatic subjects. Am J Roentgenol 176:641–645
Altomare DF (2010) ODS score and obstructed defecation. Dis Colon Rectum 53:363 author reply 363
Vaizey CJ, Carapeti E, Cahill JA et al (1999) Prospective comparison of faecal incontinence grading systems. Gut 44:77–80
Heckert J, Sankineni A, Hughes WB, Harbison S, Parkman H (2016) Gastric electric stimulation for refractory gastroparesis: a prospective analysis of 151 patients at a single center. Dig Dis Sci 61(1):168–175
Martelli H, Devroede G, Arhan P et al (1978) Mechanisms of idiopathic constipation: outlet obstruction. Gastroenterology 75:623–631
Talley NJ, Weaver AL, Zinsmeister AR et al (1993) Functional constipation and outlet delay: a population-based study. Gastroenterology 105:781–790
Schwandner O, Stuto A, Jayne D et al (2008) Decision-making algorithm for the STARR procedure in obstructed defecation syndrome: position statement of the group of STARR pioneers. Surg Innov 15:105–109
Zhang B, Ding JH, Yin SH et al (2010) Stapled transanal rectal resection for obstructed defecation syndrome associated with rectocele and rectal intussusception. World J Gastroenterol 16:2542–2548
Dodi G, Pietroletti R, Milito G et al (2003) Bleeding, incontinence, pain and constipation after STARR transanal double stapling rectotomy for obstructed defecation. Tech Coloproctol 7:148–153
Gagliardi G, Pescatori M, Altomare DF et al (2008) Results, outcome predictors, and complications after stapled transanal rectal resection for obstructed defecation. Dis Colon Rectum 51:186–195 discussion 195
Naldini G (2011) Serious unconventional complications of surgery with stapler for haemorrhoidal prolapse and obstructed defaecation because of rectocoele and rectal intussusception. Color Dis 13:323–327
De Nardi P, Bottini C, Faticanti Scucchi L et al (2007) Proctalgia in a patient with staples retained in the puborectalis muscle after STARR operation. Tech Coloproctol 11:353–356
Jayne DG, Schwandner O, Stuto A (2009) Stapled transanal rectal resection for obstructed defecation syndrome: one-year results of the European STARR Registry. Dis Colon Rectum 52:1205–1212 discussion 1212–4
Madbouly KM, Abbas KS, Hussein AM (2010) Disappointing long-term outcomes after stapled transanal rectal resection for obstructed defecation. World J Surg 34:2191–2196
Kohler K, Stelzner S, Hellmich G et al (2012) Results in the long-term course after stapled transanal rectal resection (STARR). Langenbeck's Arch Surg 397:771–778
Schiano di Visconte M, Nicoli F, Pasquali A et al (2018) Clinical outcomes of stapled transanal rectal resection (STARR) for obstructed defaecation syndrome at 10-year follow-up. Color Dis 20:614–622
Kim M, Meurette G, Lehur PA (2016) Obstructed defecation: STARR or rectopexy? Color Dis 18:438–439
Grassi R, Romano S, Micera O et al (2005) Radiographic findings of post-operative double stapled trans anal rectal resection (STARR) in patient with obstructed defecation syndrome (ODS). Eur J Radiol 53:410–416
Dindo D, Weishaupt D, Lehmann K et al (2008) Clinical and morphologic correlation after stapled transanal rectal resection for obstructed defecation syndrome. Dis Colon Rectum 51:1768–1774
Schwandner T, Hecker A, Hirschburger M et al (2011) Does the STARR procedure change the pelvic floor: a preoperative and postoperative study with dynamic pelvic floor MRI. Dis Colon Rectum 54:412–417
Piloni V, Possanzini M, Bergamasco M et al (2017) Postoperative MR defecography following failed STARR procedure for obstructive defecation syndrome: a three-centre experience. Gastroenterol Res Pract 2017:4392918
Faucheron JL, Barot S, Collomb D et al (2014) Dynamic cystocolpoproctography is superior to functional pelvic MRI in the diagnosis of posterior pelvic floor disorders: results of a prospective study. Color Dis 16:O240–O247
Author information
Authors and Affiliations
Contributions
Arcangelo Picciariello, MD: conception and design of the study, acquisition analysis and interpretation of data, writing the paper, and final approval of the version to be published
Vincenzo Papagni, MD: acquisition analysis and interpretation of the data,and final approval of the version to be published
Gennaro Martines, MD: acquisition analysis and interpretation of the data, and final approval of the version to be published
Michele De Fazio, MD: acquisition analysis and interpretation of the data, and final approval of the version to be published
Rosa Digennaro, MD: acquisition analysis and interpretation of the data, and final approval of the version to be published
Prof Donato F. Altomare, MD: aonception and design of the study, interpretation of the results, writing the paper, and final approval of the version to be published
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Picciariello, A., Papagni, V., Martines, G. et al. Post-operative clinical, manometric, and defecographic findings in patients undergoing unsuccessful STARR operation for obstructed defecation. Int J Colorectal Dis 34, 837–842 (2019). https://doi.org/10.1007/s00384-019-03263-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03263-9