Abstract
Purpose
Symptomatic rectocele results in obstructed defecation and constipation. Surgical repair may provide symptomatic relief. A variety of surgical procedures have been used in the rectocele repair to enhance anatomical and functional results and to improve long-term outcomes.
Methods
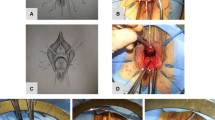
In this prospective study, we treated 25 selected women suffering from simple symptomatic rectocele with transperineal repair using porcine dermal acellular collagen matrix Biomesh (Permacol®). Watson score and SF-36 questionnaire were used to evaluate postoperative outcomes and quality of life.
Results
Follow-up ranged from 12 to 24 months, the mean total Watson score was significantly lower than the preoperative score (P < 0.001), and every patient has improved functional outcomes. There were no major intraoperative or postoperative complications. Two cases of urinary infection and 4 patients delayed wound healing were reported. Those patients who were sexually active prior to surgery have not experienced problems with sexual function or dyspareunia.
Conclusions
Despite lack of comparative study in literature, rectocele repair with Permacol® by the transperineal approach seems an effective and safe procedure that avoids some of the complications associated with synthetic mesh use.
Similar content being viewed by others
References
Dietz HP, Steensma AB (2006) The role of childbirth in the aetiology of rectocele. BJOG 113:264–267
Capps WF (1975) Rectoplasty and perineoplasty for the symptomatic rectocele: a report of fifty cases. Dis Colon Rectum 18:237–244
Sarles JC, Arnaud A, Selezneff I, Olivier S (1989) Endorectal repair of rectocele. Int J Color Dis 4:167–171
Neal Ellis C (2005) Treatment of obstructed defecation. Clin Colon Rectal Surg 18(2):85–95
Smart NJ, Mercer-Jones MA (2007 Sep) Functional outcome after transperineal rectocele repair with porcine dermal collagen implant. Dis Colon Rectum 50(9):1422–1427
Milito G, Cadeddu F, Grande M, Selvaggio I, Farinon AM (2009) Advances in treatment of obstructed defecation: biomesh transperineal repair. Dis Colon Rectum 52:2051
Altomare DF, Rinaldi M, Veglia A, Petrolino M, De Fazio M, Sallustio P (2002) Combined perineal and endorectal repair of rectocele by circular stapler: a novel surgical technique. Dis Colon Rectum 45:1549–1552
Maher C, Baessler K (2006) Surgical management of posterior vaginal wall prolapse: an evidence-based literature review. Int Urogynecol J Pelvic Floor Dysfunct 17:84–88
Ayabaca SM, Zbar AP, Pescatori M (2002) Anal continence after rectocele repair. Dis Colon Rectum 45:63–69
Zbar AP, Lienemann A, Fritsch H, Beer-Gabel M, Pescatori M (2003) Rectocele: pathogenesis and surgical management. Int J Color Dis 18(5):369–384
American College of Gastroenterology Constipation Task Force (2005) An evidence-based approach to the management of chronic constipation in North America. Am J Gastroenterol 100(Suppl 1):S1–S4
Kahn MA, Stanton SI (1997) Posterior colporrhaphy: its effects on bowel and sexual function. Br J Obstet Gynaecol 104:882–886
Khubchandani IT, Clancey JP, Rosen L, Riether RD, Stasik JJ (1997) Endorectal repair rectocele revisited. Br J Surg 84:89–91
Stojkovic SG, Balfour L, Burke D, Finan PJ, Sagar PM (2003) Does the need to self-digitate or the presence of a large or nonemptying rectocoele on proctography influence the outcome of transanal rectocoele repair? Color Dis 5:169–172
Hanson JM, Aspin B, Spalding LJ, Varma JS (2004) Transperineal repair of rectocele using porcine collagen. Color Dis 6(suppl 1):36
Altman D, Zetterstrom J, Lopez A et al (2005) Functional and anatomic outcome after transvaginal rectocele repair using collagen mesh: a prospective study. Dis Colon Rectum 48:1233–1241
Watson SJ, Loder PB, Halligan S, Bartram CI, Kamm MA, Phillips RK (1996) Transperineal repair of symptomatic ectocele with Marlex mesh: a clinical, physiological and radiologic assessment of treatment. J Am Coll Surg 183:257–261
Pescatori M, Milito G, Fiorino M, Cadeddu F (2009) Complications and reinterventions after surgery for obstructed defecation. Int J Color Dis 24:951–959
Kahn MA, Stanton SL, Kumar D, Fox SD (1999) Posterior colporrhaphy is superior to the transanal repair for treatment of posterior vaginal wall prolapse. Neurourol Urodyn 18:70–71
Nieminen K, Hiltunen K, Laitinen J, Oksala J, Heinonen P (2003) Transanal or vaginal approach to rectocele repair: results of a prospective randomized study. Neurourol Urodyn 22:547–548
Arnold MW, Stewart WR, Aguilar PS (1990) Rectocele repair. Four years’ experience. Dis Colon Rectum 33:684–687
Nieminen K, Hiltunen KM, Laitinen J, Oksala J, Heinonen PK (2004) Transanal or vaginal approach to rectocele repair: a prospective, randomized pilot study. Dis Colon Rectum 47:1636–1642
Maher C, Baessler K, Glazener CM, Adams EJ, Hagen S (2004) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4:CD004014
Fischer F, Farke S, Schwandner O, Bruch HP, Schiedeck T (2005) Functional results after transvaginal, transperineal and transrectal correction of a symptomatic rectocele. Zentralbl Chir 130:400–404
Milley PS, Nichols DH (1969) A correlative investigation of the human rectovaginal septum. Anat Rec 163:443–452
Richardson AC (1993) The rectovaginal septum revisited: its relationship to rectocele and its importance in rectocele repair. Clin Obstet Gynecol 36:976–983
Porter WE, Steele A, Walsh P, Kohli N, Karram MM (1999) The anatomic and functional outcomes of defect-specific rectocele repair. Am J Obstet Gynecol 181:1353–1359
Abramov Y, Gandhi S, Goldberg R et al (2004) Does discrete site-specific defect repair carry better objective and subjective outcomes than standard posterior colporrhaphy? Neurourol Urodyn 23:437–439
Weber AM, Walters MD, Piedmonte MR (2000) Sexual function and vaginal anatomy in women before and after surgery for pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 182:1610–1615
Singh K, Cortes E, Reid WM (2003) Evaluation of the fascial technique for surgical repair of isolated posterior vaginal wall prolapse. Obstet Gynecol 101:320–324
Maher CF, Qatawneh A, Baessler K, Schluter P (2004) Midline rectovaginal fascial plication for repair of rectocele and obstructed defecation (abstract 166). Obstet Gynecol 104:685–689
Abramov Y, Kwon C, Gandhi S, Goldberg R, Sand PK (2003) Long-term anatomic outcome of discrete site-specific defect repair versus standard posterior colporrhaphy for the correction of advanced rectocele: a 1 year follow-up analysis. Neurourol Urodyn 22:520–521
Sand PK, Koduri S, Lobel RW, Winkler HA, Tomezsko J, Culligan PJ, Goldberg R (2001) Prospective randomized trial of polyglactin 910 mesh to prevent recurrence of cystoceles and rectoceles. Am J Obstet Gynecol 184:1357–1362
Dwyer PL, O’Reilly BA (2004) Transvaginal repair of anterior and posterior compartment prolapse Atrium polypropylene mesh. BJOG 111:831–836
Salvatore S, Soligo M, Meschia M, Luppino G, Piffarotti P, Arcarci V (2002) Prosthetic surgery for genital prolapse: functional outcome. Neurourol Urodyn 21:296–297
Zimmermann EF, Hayes RS, Daniels IR, Smart NJ, Warwick AM (2017 Oct) Transperineal rectocele repair: a systematic review. ANZ J Surg 87(10):773–779
Leventoğlu S, Menteş BB, Akin M, Karen M, Karamercan A, Oğuz M (2007 Dec) Transperineal rectocele repair with polyglycolic acid mesh: a case series. Dis Colon Rectum 50:2085–2092
Author information
Authors and Affiliations
Contributions
G.L. was responsible for manuscript writing, study design, data collection, and interpretation.
M.C. was responsible for editing and drafting the manuscript.
S.G. and M.G. and D.M. were responsible for study design and performed the specimen analyses.
G.M. performed surgery and were responsible for data interpretation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lisi, G., Campanelli, M., Grande, S. et al. Transperineal rectocele repair with biomesh: updating of a tertiary refer center prospective study. Int J Colorectal Dis 33, 1583–1588 (2018). https://doi.org/10.1007/s00384-018-3054-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3054-2