Abstract
Purpose
Although lymph node metastases to pancreatic and gastroepiploic lymph node stations in transverse colon cancer have been described, the mode of lymphatic spread in this area remains unclear. This study was undertaken to describe possible pathways of aberrant lymphatic spread in the complex anatomic area of the proximal superior mesenteric artery and vein, the greater omentum, and the lower pancreatic border.
Methods
Abdominal specimens obtained from four cadaveric donors were dissected according to the principles of complete mesocolic excision. The vascular architecture of the transverse colon was scrutinized in search of possible pathways of lymphatic spread to the pancreatic and gastroepiploic lymph nodes.
Results
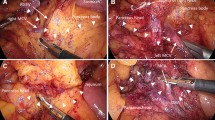
Vascular connections between the transverse colon and the greater omentum at the level of both the hepatic and the splenic flexures could be identified. In addition, small vessels running from the transverse mesocolon to the lower pancreatic border in the area between the middle colic artery and the inferior mesenteric vein were demonstrated. Moreover, venous tributaries to the gastrocolic trunk could be exposed to highlight its surgical importance as a guiding structure for complete mesocolic excision.
Conclusion
The technical feasibility to clearly separate embryologic compartments by predefined tissue planes in complete mesocolic excision was confirmed. However, the vicinity of all three endodermal intestinal segments (foregut, midgut, and hindgut) obviously gives way to vascular connections that might serve as potential pathways for lymphatic metastatic spread of transverse colon cancer.









Similar content being viewed by others
References
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision (CME) and central ligation—technical notes and outcome. Colorectal Dis 11:354–364
Søndenaa K, Quirke P, Hohenberger W, Sugihara K, Kobayashi H, Kessler H, Brown G, Tudyka V, D’Hoore A, Kennedy RH, West NP, Kim SH, Heald R, Storli KE, Nesbakken A, Moran B (2014) The rationale behind complete mesocolic excision (CME) and a central vascular ligation for colon cancer in open and laparoscopic surgery: proceedings of a consensus conference. Int J Colorectal Dis 29:419–428
Heald RJ (1988) The ‘Holy Plane’ of rectal surgery. J R Soc Med 81:503–508
Heald RJ, Moran BJ (1998) Embryology and anatomy of the rectum. Semin Surg Oncol 15:66–71
Stelzner F, Friedrichs N, von Mallek D (2009) Homing areas, enveloping fascias, and lymphatic suction vessels confine cancer growth. New MRI, CT, and clinical investigations of colorectal carcinoma. Chirurg 80:216–222
Jamieson JK, Dobson JF (1909) The lymphatics of the colon: with special reference to the operative treatment of cancer of the colon. Ann Surg 50:1077–1090
West NP, Hohenberger W, Weber K, Perrakis A, Finan PJ, Quirke P (2010) Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol 28:272–278
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol 30:1763–1769
Kobayashi H, West NP, Takahashi K, Perrakis A, Weber K, Hohenberger W, Quirke P, Sugihara K (2014) Quality of surgery for stage III colon cancer: comparison between England, Germany, and Japan. Ann Surg Oncol 21(Suppl 3):S398–S404
Bertelsen CA, Neuenschwander AU, Jansen JE, Wilhelmsen M, Kirkegaard-Klitbo A, Tenma JR, Bols B, Ingeholm P, Rasmussen LA, Jepsen LV, Iversen ER, Kristensen B, Gögenur I, Danish Colorectal Cancer Group (2015) Disease-free survival after complete mesocolic excision with conventional colon cancer surgery: a retrospective, population-based study. Lancet Oncol 16:161–168
Kim WK, Kim H, Ahn DH, Kim MH, Park HW (2003) Timetable for intestinal rotation in staged human embryos and fetuses. Birth Defects Res A Clin Mol Teratol 67:941–945
Culligan K, Coffey JC, Kiran RP, Kalady M, Lavery IC, Remzi FH (2012) The mesocolon: a prospective observational study. Colorectal Dis 14:421–430
Açar Hİ, Cömert A, Avşar A, Çelik S, Kuzu MA (2014) Dynamic article: surgical anatomical planes for complete mesocolic excision and applied vascular anatomy of the right colon. Dis Colon Rectum 57:1169–1175
Gillot C, Hureau J, Aaron C, Martini R, Michels NA (1964) The superior mesenteric vein, an anatomic and surgical study of eighty-one subjects. J Int Coll Surg 41:339–369
Toyota S, Ohta H, Anazawa S (1995) Rationale for extent of lymph node dissection for right colon cancer. Dis Colon Rectum 38:705–711
Hasegawa S, Kawamura J, Nagayama S, Nomura A, Kondo K, Sakai Y (2007) Medially approached radical lymph node dissection along the surgical trunk for advanced right-sided colon cancers. Surg Endosc 21:1657
Sakaguchi T, Suzuki S, Morita Y, Oishi K, Suzuki A, Fukumoto K, Inaba K, Kamiya K, Ota M, Setoguchi T, Takehara Y, Nasu H, Nakamura S, Konno H (2010) Analysis of anatomic variants of mesenteric veins by 3-dimensional portography using multidetector-row computed tomography. Am J Surg 200:15–22
Yamaguchi S, Kuroyanagi H, Milsom JW, Sim R, Shimada H (2002) Venous anatomy of the right colon. Precise structure of the major veins and gastrocolic trunk in 58 cadavers. Dis Colon Rectum 45:1337–1340
Jin G, Tuo H, Sugiyama M, Oki A, Abe N, Mori T, Masaki T, Atomi Y (2006) Anatomic study of the superior right colonic vein: its relevance to pancreatic and colonic surgery. Am J Surg 191:100–103
Ignjatovic D, Spasojevic M, Stimec B (2010) Can the gastrocolic trunk of Henle serve as an anatomical landmark in laparoscopic right colectomy? A postmortem anatomical study. Am J Surg 199:249–254
Henle FG (1868) Handbuch der systematischen Anatomie des Menschen. Vieweg, Braunschweig, p 371
Ignjatovic D, Stimec B, Finjord T, Bergamaschi R (2004) Venous anatomy of the right colon: three-dimensional topographic mapping of the gastrocolic trunk of Henle. Tech Coloproctol 8:19–21
Voiglio EJ, Boutillier du Retail C, Neidhardt JPH, Caillot JL, Barale F, Mertens P (1998) Gastrocolic vein. Definition and report of two cases of avulsion. Surg Radiol Anat 20:197–201
Lange JF, Koppert S, van Eyck CHJ, Kazemier G, Kleinrensink GJ, Godschalk M (2000) The gastrocolic trunk of Henle in pancreatic surgery: an anatomo-clinical study. J Hepatobiliary Pancreat Surg 7:401–403
Steward JA, Rankin FW (1933) Blood supply of the large intestine: its surgical considerations. Arch Surg 26:843–891
VanDamme JP, Bonte J (1990) Vascular anatomy in abdominal surgery. Georg Thieme, Stuttgart, p 53
Yada H, Sawai K, Taniguchi H, Hoshima M, Katoh M, Takahashi T (1997) Analysis of vascular anatomy and lymph node metastases warrants radical segmental bowel resection for colon cancer. World J Surg 21:109–115
Benedix F, Kube R, Meyer F, Schmidt U, Gastinger I, Lippert H, Colon/Rectum Carcinomas (Primary Tumor) Study Group (2010) Comparison of 17,641 patients with right- and left-sided colon cancer: differences in epidemiology, perioperative course, histology, and survival. Dis Colon Rectum 53:57–64
Meguid RA, Slidell BM, Wolfgang CL, Chang DC, Ahuja N (2008) Is there a difference in survival between right- versus left-sided colon cancers? Ann Surg Oncol 15:2388–2394
West NP, Morris EJ, Rotimi O, Cairns A, Finan PJ, Quirke P (2008) Pathology grading of colon cancer surgical resection and its association with survival: a retrospective observational study. Lancet Oncol 9:857–865
Perrakis A, Weber K, Merkel S, Matzel K, Agaimy A, Gebbert C, Hohenberger W (2014) Lymph node metastasis of carcinomas of transverse colon including flexures. Consideration of the extramesocolic lymph node stations. Int J Colorectal Dis 29:1223–1229
Bertelsen CA, Bols B, Ingholm P, Jansen JE, Jepsen LV, Kristensen B, Neuenschwander AU, Gögenur I (2014) Lymph node metastases in the gastrocolic ligament in patients with colon cancer. Dis Colon Rectum 57:839–845
Hirono S, Tani M, Kawai M, Okada K, Miyazawa M, Shimizu A, Uchiyama K, Yamaue H (2012) Identification of the lymphatic drainage pathways from the pancreatic head guided by indocyanine green fluorescence imaging during pancreaticoduodenectomy. Dig Surg 29:132–139
Morikawa E, Yasutomi M, Shindou K, Matsuda T, Mori N, Hida J, Kubo R, Kitaoka M, Nakamura M, Fujimoto K, Inofusa H, Hatta M, Izumoto G (1994) Distribution of metastatic lymph nodes in colorectal cancer by the modified clearing method. Dis Colon Rectum 37:219–223
Acknowledgments
The authors thank Stefanie Gundlach and Merle Winkler for their support in the anatomical dissections and photographing of the macroscopic specimens, Bettina Facompré for her support in the histologic work-up of the microscopic specimens, and Clemens Franke for his assistance in the processing of the figures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
NPW is supported by Yorkshire Cancer Research, UK and the Pathological Society of Great Britain and Ireland. All authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Stelzner, S., Hohenberger, W., Weber, K. et al. Anatomy of the transverse colon revisited with respect to complete mesocolic excision and possible pathways of aberrant lymphatic tumor spread. Int J Colorectal Dis 31, 377–384 (2016). https://doi.org/10.1007/s00384-015-2434-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2434-0