Abstract
Purpose
The purpose of this study was to prospectively compare rectal resection (RR) with colonic resection on sexual, urinary and bowel function and quality of life in both short-term and long-term.
Methods
Eighty-three patients who underwent RR were compared to 53 patients who underwent a colonic resection leaving the rectum in situ (RIS). A questionnaire assessing sexual, urinary and bowel functioning with a quality of life questionnaire (SF-36) was sent to all participants preoperatively, 3 and 12 months postoperatively and approximately 8 years after the onset of the study.
Results
Short-term dysfunction included diminished sexual activity in female RR patients at 3 months and significantly more erectile dysfunction in RR patients 1 year postoperatively. Long-term dysfunction included more frequent and more severe erectile dysfunction in RR patients compared to RIS patients. These short-term and long-term outcomes did not influence overall quality of life. The incidence of urinary dysfunction was comparable between both groups. Bowel functioning was significantly better in the RIS group compared to the RR group 3 months and 1 year postoperatively.
Conclusions
Patients who underwent RR experienced up to 1 year postoperatively more sexual and bowel function problems than RIS patients. However, short-term and long-term dysfunction did not influence overall quality of life. Erectile dysfunction in male RR patients persisted in time, whereas other aspects of sexual, urinary and bowel function after RR and colonic resection are similar after a median follow-up of 8.5 years.
Similar content being viewed by others
Introduction
In recent years, rectal surgery has changed dramatically. It has progressed from removal of the rectum and anus with a permanent colostomy to the present era with total mesorectal excision (TME) and sphincter-saving surgery [1]. Improvements in treatment and early detection of rectal cancer indicate that more patients will be treated for rectal cancer and, therefore, more patients will live with the consequences of the treatment of this disease [2,3]. Mesorectal excision improves oncological outcome but it may result in decreased sexual, urogenital and anorectal function [4–6], unless careful attention is given to nerve preservation [7].
In the Western world, similar increasing incidences of disease are seen for inflammatory bowel disease (IBD) [8]. Although reports are inconsistent to what extent surgery is required for IBD, resections for benign disease are performed according to the TME principle. Therefore, this group of patients is also at risk for nerve damage, which can consequently cause functional disorders postoperatively. The impact of functional disorders, for example, loss of sexual function, is probably even greater after surgery for benign disease in younger patients, although the risk of postoperative disorders is considerably lower in this population [9].
The awareness and a better understanding of sexual and bladder physiology [10] and pelvic anatomy [11–13] have shifted the focus of research towards nerve-preserving techniques with functional results and quality of life as main clinical endpoints. However, the importance of the topic is not reflected in the relatively scarce available studies. Moreover, previous studies are difficult to interpret because data were often retrospectively collected and, therefore, baseline function was not available.
In the present era with an increased number of rectal resections (RR) and the alarming percentages in retrospective studies of decreased postoperative sexual, urogenital and anorectal function, prospective evaluation is warranted. However, sexual function is influenced by many factors and, until recently, no validated questionnaire was available for assessing sexual functioning. Furthermore, not all patients are sexually active, and patients who are, tend to avoid some questions about sexual functioning.
By comparing functional outcome of RR patients with patients operated in the abdomen for other causes, the possible confounders might be smaller than comparing RR patients with a gender- and age-matched group of patients from the general population, as both groups are experiencing similar distress of having a disease and undergoing surgery.
Therefore, the aim of the present study was to prospectively compare the long-term sexual and urinary function between patients who underwent RR according to TME principles and a control group of patients after either a hemicolectomy or subtotal colectomy or an ileocolic resection. Bowel function and quality of life were secondary endpoints.
Materials and methods
Between 1997 and 2000, patients of 16 years and older who underwent RR or colonic resection at the Academic Medical Centre in Amsterdam, the Netherlands were included in the study. Patients who underwent an emergency procedure were not included in the study, as were patients scheduled for a sigmoidal resection. Furthermore, patients who received postoperative radiotherapy were excluded from the study. To enable comparison with baseline results, only patients who returned their preoperative questionnaires were eligible. A total of 136 patients (63 males and 73 females) with a written informed consent were included: 83 patients in the RR group and 53 in the colonic resection group with the rectum in situ (RIS). All patients received the treatment according to the group they were allocated for.
At the onset of this study, surgery without preoperative radiotherapy was the standard treatment for operable rectal cancer. For this reason and the fact that a large proportion of the patients were operated on for IBD, none of the patients were irradiated preoperatively. All RR patients were operated on according to the TME technique. Patient characteristics are listed in Table 1. Pathological tumour stage was assessed in patients after RR (n = 25): A, T1–2 N0 M0 in 8 out of 25 patients (32%); B, T3–4 N0 M0 in 12 out of 25 patients (48%); C, T1–4 N1–2 M0 in 5 out of 25 patients (20%). None of the patients were diagnosed with metastatic disease (D, T1–4 N1–2 M1). In 5 out of 25 patients (20%), the circumferential resection margin (CRM) was involved.
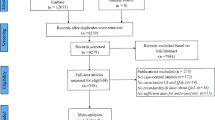
Questionnaires were sent to all patients preoperatively and 3 and 12 months postoperatively. All patients were contacted again after a median follow-up of 8 years and 6 months (range, 7–10 years) and asked to fill in the same questionnaire. General practitioners and local authorities were contacted to ask whether patients were still alive and to provide address information in order to minimise loss to follow-up. Details about the study cohort and the response rates at the different time-points are listed in Fig. 1.
To assess sexual and urinary functioning, a questionnaire containing specific questions on sexual and urinary function was sent to all patients preoperatively, at 3 and 12 months after the operation and after at least 7 years. This disease-related questionnaire contained 26 questions subdivided into 2 subscales: sexual functioning (20 items) and micturition (6 items). Patients were asked about sexual activity, body image and sexual enjoyment (seven items) with additional questions for females (sexual arousal, dyspareunia, orgasm, incontinence during intercourse (six items)) and males (erection, retrograde ejaculation, incontinence during intercourse (seven items)). To assess urinary functioning, patients were asked about frequency (three items) and incontinence (three items). All questions described three to five possible answers; these answers were scored in a 0 to 5 range, with higher scores indicating more functional problems.
Bowel function was assessed by 12 items (the number of stools during the day and at night, stool consistency, soiling or incontinence during the day or at night, incontinence for gas, ability to distinguish between flatus and faeces, need for anti-diarrhoeal medication, dietary restrictions and incidence of perianal skin irritation), which were formulated as three-option to five-option multiple-choice questions. These scores were adjusted to create a composite score that not only focussed exclusively on incontinence but also covered the complete bowel function and were analysed by the validated Gastro-Intestinal Functional Outcome (GIFO) score [14]. The resulting GIFO score was linearly transformed to fit in a score range from 0 to 100, with higher scores indicating a better overall function.
Furthermore, all patients received a general quality of life questionnaire (SF-36) at all time-points. The SF-36 is a validated, widely used questionnaire in postoperative patients, consisting of eight multi-item scales: physical functioning (PF), role physical (RP), bodily pain (BP), general health perception (GH), vitality (VT), social functioning (SF), role emotional (RE) and mental health (MH). The scores are linearly transformed to fit in a score range from 0 to 100, with higher scores indicating better health-related quality of life status [15]. Results of the study population were compared with the general population (n = 1,742) using data from a study by Aaronson et al. This study translated and validated the SF-36 health survey for the Dutch population [16].
Statistical analysis
Patients were instructed to answer the questions based on the last 3 months at all time-points. In the first item of the questionnaire assessing sexual function, patients were asked if they had been sexually active in the last 3 months. If the answer was negative, patients continued with the questionnaires assessing urinary function and bowel function. Male and female patients were analysed separately for sexual functioning. Furthermore, postoperative deterioration of sexual functioning was evaluated. In order to do so, relative dysfunction scores were obtained by subtracting the baseline score from the score at each subsequent time-point. For each patient, the postoperative relative scores with respect to the several items in the questionnaire were calculated. In this way, even patients who filled in one postoperative questionnaire could be evaluated. Bowel function could only be assessed in the absence of a stoma.
Demographic data were expressed as percentages for categorical data, as mean and standard deviation for normally distributed numerical data and as median and range for non-normally distributed numerical data. The groups were considered to be normally distributed with the Kolmogorov–Smirnov (n > 50) or Shapiro–Wilk (n < 50) score of >0.05. The Mann–Whitney and independent samples t test were used to compare data between the two groups. To analyse changes in outcome parameters over time within each group separately, the Wilcoxon test and the paired samples t test were used. The t test was applied when both groups were normally distributed and the Mann–Whitney or Wilcoxon test was used in the remaining cases.
As the percentages of missing surveys were not significantly different between the RR and the RIS groups, analysis was performed for the subset of patients that returned the questionnaire. For all analyses, a p value less than 0.05 (two-sided) was considered significant. Statistical analyses were performed with Statistical Package for the Social Sciences (SPSS) version 15.0 (SPSS Inc., Chicago, IL, USA).
Results
Sexual functioning
Sexual activity declined from a preoperative rate of 73% (59 out of 81) to 57% (43 out of 76) at 3 months postoperatively in the RR group (p = 0.002), whereas no significant differences between preoperative and postoperative sexual activity could be demonstrated in the RIS group (p = 0.248; Table 2). After approximately 8 years of follow-up, no significant difference in sexual activity was seen between both groups. This effect appeared to be age-dependent: median age in the sexually active RR group and RIS group was 47 (29–79) and 43 (27–68) years, respectively, while median age in the sexually inactive RR group and RIS group was 58 (37–78) and 57 (37–77) years, respectively (p < 0.001). The most profound decrease in sexual activity was found in female patients of the RR group at 3 months postoperatively.
Two of the 12 patients reported regular dyspareunia at 3 months postoperatively, while only 1 of 22 patients experienced regular dyspareunia preoperatively (Table 3). Although most females experienced diminished physical arousal, this problem was seen at all time-points in both groups, and the majority of female participants stated to be satisfied with their sexual life. The ability to have orgasms did not change among female patients in both the RR and the RIS groups. Faecal incontinence during sexual intercourse was not frequently reported and did not have a major influence on sexual activity.
Male sexual function was more impaired in the RR group. Five of 32 patients in the RR group experienced erectile dysfunction regularly at 12 months and another 3 patients reported that erectile dysfunction occurred at all times. Thus, 8 of the male RR patients experienced severe erectile dysfunction at 12 months postoperatively, whereas this problem was reported by 1 of 37 patients preoperatively (p = 0.025). Severe erectile dysfunction persisted in 8 of 22 patients in the RR group after long-term follow-up, whereas no such dysfunction was reported in the RIS group (p = 0.001; Table 4). Besides erection failures, patients who underwent RR experienced less sufficiency of the erection and a shorter duration of the erection. At 12 months and long-term follow-up, four and five patients in the RR group reported to experience less sufficiency of the erection and a shorter duration of the erection at all times, compared with two patients (one in each group) reporting regular insufficiency and a regular shorter duration of the erection preoperatively (p = 0.010). Pain during an orgasm was reported incidentally; preoperatively in 3 of 47 male patients and at 3 months in 9 of 40 male patients (p = 0.046), mainly in the RR group. None of the patients in the RR group experienced retrograde ejaculation preoperatively, but at 12 months postoperatively, 3 of 32 patients reported that retrograde ejaculation occurred at all times. In those patients not reporting any retrograde ejaculation or erectile dysfunction, sexual function was comparable with control patients in the RIS group. Preoperative questionnaires showed that none of the male patients experienced orgasm failures in both groups. At 3 months after RR, 1 of 31 males lost the ability to have an orgasm, with orgasm failures at 1 year in 3 of 32 males. Orgasm failure was also seen in the RIS group: one male patient reported regular orgasm failure at 3 and 12 months postoperatively.
Sexual functional disturbances did not result in significant differences regarding body image, sexual satisfaction and the ability to have orgasms between the two groups, neither in female nor in male patients.
Urinary functioning
The degree of urinary incontinence as reported in the RR and RIS groups at each time interval was not significantly different, as displayed in Table 5. Although an absolute decrease of urinary continence of 11% in the RR group (68 out of 80 to 43 out of 58) and 15% in the RIS group (45 out of 53 to 26 out of 37) was observed after a median interval of 8.5 years, no significant impact of colorectal surgery on overall urinary functioning could be demonstrated.
Tumour pathology stage
In subgroup analysis of patients after RR for rectal cancer, it was found that advanced tumour stage did not significantly influence functional results. However, of the five patients with CRM involvement, only three patients were sexually active preoperatively and two patients at 3 months after the operation. The incidence of urinary incontinence was not significantly increased in patients with advanced tumour stage.
The presence of a stoma
As demonstrated in Table 1, the presence of a stoma occurred in both groups at all time-points, as demonstrated by the 34 out of a total of 121 (28%) patients having a stoma at 3 months. Preoperatively, all but one patient with a stoma were diagnosed with benign disease. The majority of this group of patients was sexually active preoperatively (19 out of 26 patients (73%)) and remained active postoperatively. In the group of patients with a stoma at 3 months after surgery, a large decrease in sexual activity was found from 19 out of 34 (56%) patients preoperatively to 9 out of 34 (26%) patients postoperatively (p = 0.001). This group of patients was mainly diagnosed with malignancies. Significant differences in sexual functioning in patients having a stoma and patients not having a stoma could not be demonstrated nor could an effect on urinary dysfunctioning be found.
Bowel functioning
Bowel function was significantly diminished in RR patients compared to RIS patients at 3 months, with a mean score of 62 (±9) and 74 (±8), respectively (p = 0.001). These differences were still significant after 1 year of follow-up, with a mean score of 63 (±11) and 72 (±9), respectively (p = 0.001). After a median time interval of 8.5 years from initial surgery, bowel function was similar in both groups, with a mean score of 65 (±10) in the RR group and 69 (±10) in the RIS group (Fig. 2).
Bowel functioning over time comparing the RR group and the RIS group. Superscript letter a indicates that the scores are linearly transformed to fit in a score range from 0 to 100, with lower scores indicating more bowel function problems. *p < 0.01 Wilcoxon test preoperative vs. 3 months RR group; ± p < 0.01 Mann–Whitney and independent samples t test RR vs. RIS
Quality of life
Overall quality of life preoperatively, at 3 and 12 months postoperatively and after long-term follow-up is shown in Fig. 3. Preoperatively, quality of life in the RR group was significantly better than the RIS group in all but one (PF) subscale. Three and 12 months after surgery, only the ‘GH’ subscale was significantly better in the RR group compared to the RIS group. At a median time interval of 8 years and 6 months after surgery, no significant differences between the RR and RIS groups were found.
Overall quality of life scores of the general population [16] versus the RR and RIS groups at different time-points. The SF-36 scores are linearly transformed to fit in a score range from 0 to 100, with higher scores indicating a better health-related quality of life status. Significance was tested by the Wilcoxon test (p < 0.05). Asterisk significant differences between the RR group compared to the RIS group. Preoperatively, quality of life in the RR group was significantly better than the RIS group in all but one (PF) subscales. Plus–minus sign significant differences between the RR/RIS group compared to the general population. In comparison with the general population, the preoperative scores from the RR group were significantly lower in three subscales (RP, GH and RE), whereas quality of life in the RIS group was significantly lower in all subscales
The quality of life scores over time within the RR group showed that only the ‘RP’ subscale was significantly diminished at 3 months after surgery in comparison with the preoperative results. Six of eight scales demonstrated significant improvement at 12 months compared to corresponding scores at 3 months postoperatively within the RR group (PF, RP, BP, VT, SF and MH). After more than 8 years of follow-up, quality of life deteriorated compared to the 12 months results in six of eight scales (RP, BP, GH, VT, SF and MH). Within the RIS group, five of eight subscales improved at 3 months postoperatively in comparison with the preoperative scores (RP, BP, VT, SF and MH). From 3 to 12 months, the ‘RP’ scale improved significantly. More than 8 years after surgery, quality of life was not significantly deteriorated in the RIS group, compared to the 12 months results.
Figure 3 demonstrates the quality of life results from the general population and the results from the RR and RIS groups. In comparison with the general population, the preoperative scores from the RR group were significantly lower in three subscales (RP, GH and RE), whereas quality of life in the RIS group was significantly lower in all subscales. After 3 months, both the RR and RIS groups scored lower in three subscales (RP, GH and RE), compared with the general population. Twelve months postoperatively, one (RP) and two (RP and GH) subscales were worse than the general population in the RR and RIS groups, respectively. This difference was still seen after long-term follow-up: two subscales were worse in both groups (RP and GH) and one additional scale was scored worse in the RIS group (RE).
Discussion
In the present analysis, the long-term functional results of RR could be reliably assessed because of the high response rate of more than 80% (95 out of 118 patients alive) with a median follow-up of 8.5 years from surgical intervention. This study demonstrates a significant increase of male sexual dysfunction and female sexual inactivity after rectal surgery in comparison with patients who underwent abdominal surgery without dissection in the pelvic cavity. After long-term follow-up, male erectile function after RR was still significantly diminished, whereas other sexual and bladder functions were similar in both groups and comparable to preoperative functioning.
To our knowledge, there are no prospective trials with sexual and urinary functional disorders after rectal surgery as a primary endpoint. Furthermore, the retrospective nature of historical studies with the lack of baseline variables limits the interpretation of previous results. However, we are aware of some shortcomings of the present trial. By evaluating the impact of surgery alone on sexual, urinary and bowel function, we assessed patients who underwent TME for benign or malignant disease. We believe our data are not confounded, as RR patients were all operated on according to the same technique (TME). Furthermore, we not only compared patients after colonic resection with patients after RR, but also compared within patients differences from baseline. However, statistical bias due to the heterogeneous population cannot be ruled out. Over 70% of the study population consisted of patients with benign disease. Reported nerve damage after benign disease is lower compared to rectal cancer surgery. Therefore, the magnitude of the problem of functional disorders as described in the present study is probably even greater if only patients with malignant disease were included. Avoidance of nerve damage is not always possible, especially in case of tumour infiltration, and a radical resection in the narrow male pelvis can be a great challenge. In subgroup analysis of patients after RR for rectal cancer, we could not demonstrate significant differences between tumour stages, possibly due to sample size.
Sexual dysfunction can be influenced postoperatively by other factors than surgery alone, such as the recovery period after surgery, coping with disease and body image. These factors are temporary and are not influencing results after a long-term follow-up. In case of partial nerve damage, initial dysfunction can temporarily be reduced, but can recover in the first years after the initial operation. Therefore, a long-term follow-up of approximately 8 years is valuable and mandatory to assess whether the reduced function is definite or not.
At the onset of this study, validated questionnaires concerning specific sexual problems were not available yet. Therefore, after consultation of the Department of Sexology, we used a Dutch questionnaire to evaluate sexual and urinary function and compared results between and within groups to baseline scores.
Another shortcoming is caused by missing surveys: the fact that patients with a stoma or patients who are sexually inactive cannot answer the questionnaire resulted in a relatively small number of patients. This might be an explanation for the fact that trends in certain functional disorders did not reach statistical significance. Avoidance to communicate about sexual problems is a known problem in most studies conducted on this subject [2]. By excluding sexually inactive patients in the present trial, response rates to the questionnaire assessing sexual function were similar to response rates to the other questionnaires, thereby limiting the possible bias. In the present study, a significant decline in sexual activity was seen in patients with and without a stoma. Although this finding does not inform us about sexual functioning, it is an important aspect in preoperative and postoperative counselling. Furthermore, it seems that distress of having cancer (and a stoma) is causing a higher rate of sexual inactivity in comparison with patients diagnosed with benign disease.
Overall, decreased sexual activity was found after RR, both in male and female patients, but sexual activity returned to baseline levels after 1 year of follow-up. Although reasons for sexual inactivity were not reported, it might be related to the frequently reported dyspareunia after RR, which persisted even after long-term follow-up. A retrospective study on sexual health in women following pelvic surgery for rectal cancer reported a significant influence on functional problems, but this study had a response rate of only 37% [17]. Another retrospective study, with a high response rate of 81%, reported a decrease in sexual activity from 61% preoperatively to 32% postoperatively in female patients [18], which is similar to our findings. More recently, a prospective trial of sexual dysfunction after rectal cancer treatment reported an incidence of male sexual dysfunction of approximately 76% and female sexual dysfunction of approximately 59% [19].
In the present study, 3 of 32 male patients experienced retrograde ejaculation at all times and 8 of 32 patients reported severe erectile dysfunction 1 year after RR. This seems to be comparable with other studies. A prospective study evaluated 29 male patients for functional disorders after RR, by comparing baseline with postoperative results. Thirty percent experienced sexual dysfunction postoperatively [20]; no long-term follow-up data were available. In a review of 13 mainly retrospective studies, erectile dysfunction was recorded in 20% of patients, and in 8 of these studies, loss of ejaculation occurred in 40% of patients after sphincter-saving surgery for rectal cancer. Preoperative radiotherapy, which might contribute to this high rate of sexual dysfunction, was not reported in all but one of these studies. The results for benign disease are better, especially after the introduction of restorative proctocolectomy, with erectile dysfunction rates of 0–4% and loss of ejaculation in 0–17% [9].
The low rate of urinary problems in the present study is in contrast to the literature. All RR patients were operated on according to the same technique (TME), and the surgical team consisted of two specialised surgeons conscious of the risk of nerve damage and, therefore, using sharp dissection under vision along Denonvilliers’ fascia. Furthermore, the study population consisted of a relatively high rate of benign disease. In rectal cancer surgery, one cannot always prevent damage to the nerve plexus in order to achieve a R0 resection. The occurrence of minor or moderate urinary symptoms early after TME has been reported in up to 35% of patients, but little is known about long-term bladder function [21–25]. Theoretically, urinary symptoms such as voiding are associated with damage to the parasympathetic nerves, leading to detrusor denervation and decreased sensitivity of the bladder. Long-term improvement can be expected by a high degree of reversibility of partially damaged nerves and functional compensation by unimpaired nerve pathways [26,27].
Deprived bowel functioning is a well-acknowledged phenomenon after rectal surgery [6,28,29]. In the present study, we also found major bowel dysfunction early after RR. After more than 8 years of adjustment, these differences were no longer significant when compared to the control group.
In this study, we could not demonstrate a significant influence of impaired function on quality of life. By comparing our baseline results for quality of life, the preoperative scores of the RIS group were significantly worse for all but one subscale (PF) compared to the RR group. Possibly, the large proportion of IBD patients in the control group is explaining this finding. This difference in quality of life was less clear after 3 months and was no longer present after more than 8 years. Preoperative scores for quality of life were, as expected, lower than scores of the general population. Apparently, not only the functional outcome of the operation is causing a reduction in quality of life, but the patient’s underlying disease and the need for colorectal surgery as well.
Conclusion
Although results in this prospective comparative study are mainly descriptive and at risk of bias due to small sample size and heterogeneous population, we found significant dysfunction after rectal surgery. The short-term dysfunction included diminished sexual activity in female patients at 3 months and significantly more erectile dysfunction in male patients 1 year postoperatively. Long-term dysfunction included more frequent and more severe erectile dysfunction in RR patients compared to RIS patients. Other aspects of sexual, urinary and bowel function after RR and colonic resection are similar, both in the short-term as after a median follow-up of 8.5 years.
References
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1:1479–1482
Engel J, Kerr J, Schlessinger-Raab A et al (2003) Quality of life in rectal cancer patients: a four-year prospective study. Ann Surg 238:203–213
Pahlman L (2001) The rectal cancer debate. Eur J Surg Oncol 27:439
Marijnen CA, van de Velde CJ, Putter H et al (2005) Impact of short-term preoperative radiotherapy on health-related quality of life and sexual functioning in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol 23:1847–1858
Vironen JH, Kairaluoma M, Aalto AM, Kellokumpu IH (2006) Impact of functional results on quality of life after rectal cancer surgery. Dis Colon Rectum 49:568–578
Peeters KC, van de Velde DJ, Leer JW et al (2005) Late side effects of short-course preoperative radiotherapy combined with total mesorectal excision for rectal cancer: increased bowel dysfunction in irradiated patients—a Dutch colorectal cancer group study. J Clin Oncol 23:6199–6206
Pocard M, Zinzindohoue F, Haab F et al (2002) A prospective study of sexual and urinary function before and after total mesorectal excision with autonomic nerve preservation for rectal cancer. Surgery 131:368–372
Gismera CS, Aladren BS (2008) Inflammatory bowel diseases: a disease(s) of modern times? Is incidence still increasing? World J Gastroenterol 14:5491–5498
Keating JP (2004) Sexual function after rectal resection. ANZ J Surg 74:248–259
Enker WE (1992) Potency, cure, and local control in the operative treatment of rectal cancer. Arch Surg 127:1396–1401
Wallner C, Lange MM, Bonsing BA et al (2008) Causes of faecal and urinary incontinence after total mesorectal excision for rectal cancer based on cadaveric surgery. J Clin Oncol 26:4466–4472
Lee JF, Maurer VM, Block GE (1973) Anatomic relations of pelvic autonomic nerves to pelvic operations. Arch Surg 107:324–328
Heald RJ, Moran BJ, Brown G et al (2004) Optimal total mesorectal excision for rectal cancer is by dissection in from of Denonvilliers’ fascia. Br J Surg 91:121–123
van Duijvendijk P, Slors JF, Taat CW et al (1999) Functional outcome after colectomy and ileorectal anastomosis compared with proctocolectomy and ileal pouch-anal anastomosis in familial adenomatous polyposis. Ann Surg 230:648–654
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Aaronson NK, Muller M, Cohen PD et al (1998) Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol 51:1055–1068
Platell CF, Thompson PJ, Makin GB (2004) Sexual health in women following pelvic surgery for rectal cancer. Br J Surg 91:465–468
Hendren SK, O’Connor BI, Liu M et al (2005) Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg 242:212–223
Lange MM, Marijnen CAM, Maas CP et al (2009) Risk factors for sexual dysfunction after rectal cancer treatment. Eur J Cancer 45:1578–1588
Sterk P, Shekarriz B, Gunter S et al (2005) Voiding and sexual dysfunction after deep rectal resection and total mesorectal excision: prospective study on 52 patients. Int J Colorectal Dis 20:423–427
Lange MM, Maas CP, Marijnen CAM (2008) Urinary dysfunction after rectal cancer treatment is mainly caused by surgery. Br J Surg 95:1020–1028
Jayne DG, Brown JM, Thorpe H et al (2005) Bladder and sexual function following resection for rectal cancer in a randomized clinical trial of laparoscopic versus open technique. Br J Surg 92:1124–1132
Maas CP, Moriya Y, Steup WH et al (2000) A prospective study on radical and nerve-preserving surgery for rectal cancer in the Netherlands. Eur J Surg Oncol 26:751–757
Maeda K, Maruta M, Utsumi T et al (2003) Bladder and male sexual functions after autonomic nerve-sparing TME with or without lateral node dissection for rectal cancer. Tech Coloproctol 7:29–33
Maurer CA (2005) Urinary and sexual function after total mesorectal excision. Recent Results Cancer Res 165:196–204
Kneist W, Junginger T (2007) Long-term urinary dysfunction after mesorectal excision: a prospective study with intraoperative electrophysiological confirmation of nerve preservation. Eur J Surg Oncol 33:1068–1074
Del RC, Sanchez-Santos R, Oreja V et al (2004) Long-term urinary dysfunction after rectal cancer surgery. Colorectal Dis 6:198–202
van Duijvendijk P, Slors JF, Taat CW et al (2002) Prospective evaluation of anorectal function after total mesorectal excision for rectal carcinoma with or without preoperative radiotherapy. Am J Gastroenterol 97:2282–2289
van Duijvendijk P, Slors JF, Taat CW et al (2003) A prospective evaluation of anorectal function after total mesorectal excision in patients with a rectal carcinoma. Surgery 133:56–65
Acknowledgments
Obituary
In November 2009, Frederik Slors passed away. As a colorectal surgeon in the AMC in Amsterdam, he contributed to the accomplishment of this study. We lost in him a skilful surgeon and a highly appreciated colleague.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Doeksen, A., Gooszen, J.A.H., van Duijvendijk, P. et al. Sexual and urinary functioning after rectal surgery: a prospective comparative study with a median follow-up of 8.5 years. Int J Colorectal Dis 26, 1549–1557 (2011). https://doi.org/10.1007/s00384-011-1288-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-011-1288-3