Abstract
Objective
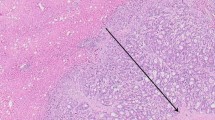
The purpose of this study was to evaluate the effect of intrahepatic microvascular and lymphatic infiltration on survival in cases of colorectal liver metastases.
Materials and methods
Prospectively collected data of 331 patients were analyzed for microvascular invasion (V), lymphatic infiltration (L), and resection margins (R) with respect to overall and disease-free survival.
Results
One-, 3-, and 5-year overall survival rates for R0 resected patients were 89%, 64%, and 39%, respectively. The corresponding survival rates for R1 resected patients were 83%, 42%, and 24% (p < 0.001). The sole presence of microvascular invasion (V1) or lymphatic infiltration (L1) was not associated with a diminished overall survival (p > 0.05). However, patients with a combination of L1V1 had a significantly worse overall survival of 68%, 20%, and 0% when compared to L0V0 patients. This difference was not influenced by the status of the resection margin. No other parameter investigated was found to be of predictive value.
Conclusions
The presence of combined lymphatic and vascular invasion (L1V1) constitutes a predictor of poor overall and disease-free survival. This subgroup of patients might benefit from adjuvant strategies such as chemotherapeutic treatment.



Similar content being viewed by others
References
Belli G, D'Agostino A, Ciciliano F et al (2002) Liver resection for hepatic metastases: 15 years of experience. J Hepatobiliary Pancreat Surg 9:607–613
Bodingbauer M, Tamandl D, Schmid K et al (2007) Size of surgical margin does not influence recurrence rates after curative liver resection for colorectal cancer liver metastases. Br J Surg 94:1133–1138
DeMatteo RP, Fong Y, Blumgart LH (1999) Surgical treatment of malignant liver tumours. Baillieres Best Pract Res Clin Gastroenterol 13:557–574
Fusai G, Davidson BR (2003) Management of colorectal liver metastases. Colorectal Dis 5:2–23
van de Velde CJ (2005) Treatment of liver metastases of colorectal cancer. Ann Oncol 16(Suppl 2):ii144–ii119
Fong Y, Fortner J, Sun RL et al (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230:309–318
Scheele J, Altendorf-Hofmann A, Stangl R, Schmidt K (1996) Surgical resection of colorectal liver metastases: gold standard for solitary and radically resectable lesions. Swiss Surg 4:4–17
Biasco G, Derenzini E, Grazi G et al (2006) Treatment of hepatic metastases from colorectal cancer: many doubts, some certainties. Cancer Treat Rev 32:214–228
Choti MA, Sitzmann JV, Tiburi MF et al (2002) Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg 235:759–766
Minagawa M, Makuuchi M, Torzilli G et al (2000) Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal cancer: long-term results. Ann Surg 231:487–499
Gayowski TJ, Iwatsuki S, Madariaga JR et al (1994) Experience in hepatic resection for metastatic colorectal cancer: analysis of clinical and pathologic risk factors. Surgery 116:703–710
Liu LX, Zhang WH, Jiang HC (2003) Current treatment for liver metastases from colorectal cancer. World J Gastroenterol 9:193–200
Tanaka K, Shimada H, Matsuo K et al (2004) Outcome after simultaneous colorectal and hepatic resection for colorectal cancer with synchronous metastases. Surgery 136:650–659
Pawlik TM, Scoggins CR, Zorzi D et al (2005) Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg 241:715–712
Sasaki A, Aramaki M, Kawano K et al (2002) Prognostic significance of intrahepatic lymphatic invasion in patients with hepatic resection due to metastases from colorectal carcinoma. Cancer 95:105–111
DeOliveira ML, Cunningham SC, Cameron JL et al (2007) Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg 245:755–762
Nakajima T, Kondo Y, Miyazaki M, Okui K (1988) A histopathologic study of 102 cases of intrahepatic cholangiocarcinoma: histologic classification and modes of spreading. Hum Pathol 19:1228–1234
Korita PV, Wakai T, Shirai Y et al (2007) Intrahepatic lymphatic invasion independently predicts poor survival and recurrences after hepatectomy in patients with colorectal carcinoma liver metastases. Ann Surg Oncol 14:3472–3480
Bockhorn M, Jain RK, Munn LL (2007) Active versus passive mechanisms in metastasis: do cancer cells crawl into vessels, or are they pushed? Lancet Oncol 8:444–448
Nagashima I, Takada T, Matsuda K et al (2004) A new scoring system to classify patients with colorectal liver metastases: proposal of criteria to select candidates for hepatic resection. J Hepatobiliary Pancreat Surg 11:79–83
Nordlinger B, Guiguet M, Vaillant JC et al (1996) Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer 77:1254–1262
Ueno H, Mochizuki H, Hashiguchi Y et al (2004) Predictors of extrahepatic recurrence after resection of colorectal liver metastases. Br J Surg 91:327–333
Parks R, Gonen M, Kemeny N et al (2007) Adjuvant chemotherapy improves survival after resection of hepatic colorectal metastases: analysis of data from two continents. J Am Coll Surg 204:753–761
Cady B, McDermott WV (1985) Major hepatic resection for metachronous metastases from colon cancer. Ann Surg 201:204–209
Liska V, Treska V, Holubec L et al (2007) Recurrence of colorectal liver metastases after surgical treatment: multifactorial study. Hepatogastroenterology 54:1741–1744
Kohne CH, Folprecht G (2004) Current perspectives in the treatment of metastatic colorectal cancer. Ann Oncol Suppl 4:iv43–iv53
McCarthy M (2003) Antiangiogenesis drug promising for metastatic colorectal cancer. Lancet 361:1959
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bockhorn, M., Sotiropoulos, G., Neuhaus, J. et al. Prognostic impact of intrahepatic lymphatic and microvascular involvement in cases of colorectal liver metastases. Int J Colorectal Dis 24, 845–850 (2009). https://doi.org/10.1007/s00384-009-0674-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-009-0674-6