Abstract
Purpose
Micro-UltraSound (microUS) is a new imaging modality capable of identifying and targeting suspicious areas, which might further increase the diagnostic yield of prostate biopsy (PBx). Aim of this review is to provide insights into the usefulness of microUS for the sub-stratification of prostate cancer (PCa), clinically significant PCa (i.e., any Gleason score ≥ 7 PCa; csPCa) along with non-organ-confined disease in patients undergoing PBx.
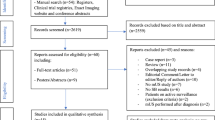
Methods
A PubMed literature search was performed using keywords: prostate cancer diagnosis, prostate cancer diagnosis surveillance, systematic biopsy, target biopsy, micro-ultrasound, and prostate risk identification using micro-ultrasound.
Results
MicroUS could significantly improve multiparametric magnetic resonance imaging (mpMRI) findings by adding valuable anatomical and pathological information provided by real-time examination. Furthermore, microUS target biopsy could replace systematic biopsy in clinical practice by reducing the detection of clinically insignificant (ciPCa) and increasing that of csPCa. Finally, microUS may be useful in predicting the presence of non-organ confined PCa before radical prostatectomy and it could also be an effective add-on tool for patient monitoring within the active surveillance program.
Conclusion
MicroUS may represent an attractive step forward for the management of csPCa as a complementary or alternative tool to mpMRI. Nevertheless, further longitudinal studies are warranted, and the strength of the evidence is still suboptimal to provide clear recommendations for daily clinical practice.
Similar content being viewed by others
Availability of data and materials
Not applicable.
References
Gandaglia G, Albers P, Abrahamsson P-A et al (2019) Structured population-based prostate-specific antigen screening for prostate cancer: the European Association of Urology position in 2019. Eur Urol 76:142–150. https://doi.org/10.1016/j.eururo.2019.04.033
Klotz L, Chin J, Black PC et al (2021) Comparison of multiparametric magnetic resonance imaging-targeted biopsy with systematic transrectal ultrasonography biopsy for biopsy-naive men at risk for prostate cancer: a phase 3 randomized clinical trial. JAMA Oncol 7:534. https://doi.org/10.1001/jamaoncol.2020.7589
Kasivisvanathan V, Rannikko AS, Borghi M et al (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 378:1767–1777. https://doi.org/10.1056/NEJMoa1801993
van der Leest M, Cornel E, Israël B et al (2019) Head-to-head comparison of transrectal ultrasound-guided prostate biopsy versus multiparametric prostate resonance imaging with subsequent magnetic resonance-guided biopsy in biopsy-naïve men with elevated prostate-specific antigen: a large prospective multicenter clinical study. Eur Urol 75:570–578. https://doi.org/10.1016/j.eururo.2018.11.023
Rouvière O, Puech P, Renard-Penna R et al (2019) Use of prostate systematic and targeted biopsy on the basis of multiparametric MRI in biopsy-naive patients (MRI-FIRST): a prospective, multicentre, paired diagnostic study. Lancet Oncol 20:100–109. https://doi.org/10.1016/S1470-2045(18)30569-2
Ahmed HU, El-Shater Bosaily A, Brown LC et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389:815–822. https://doi.org/10.1016/S0140-6736(16)32401-1
Ahdoot M, Wilbur AR, Reese SE et al (2020) MRI-targeted, systematic, and combined biopsy for prostate cancer diagnosis. N Engl J Med 382:917–928. https://doi.org/10.1056/NEJMoa1910038
Drost F-JH, Osses DF, Nieboer D et al (2019) Prostate MRI, with or without MRI-targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD012663.pub2
Kasivisvanathan V, Stabile A, Neves JB et al (2019) Magnetic resonance imaging-targeted biopsy versus systematic biopsy in the detection of prostate cancer: a systematic review and meta-analysis. Eur Urol 76:284–303. https://doi.org/10.1016/j.eururo.2019.04.043
Mottet N, van den Bergh RCN, Briers E et al (2021) EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer—2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 79:243–262. https://doi.org/10.1016/j.eururo.2020.09.042
Sathianathen NJ, Omer A, Harriss E et al (2020) Negative predictive value of multiparametric magnetic resonance imaging in the detection of clinically significant prostate cancer in the prostate imaging reporting and data system era: a systematic review and meta-analysis. Eur Urol 78:402–414. https://doi.org/10.1016/j.eururo.2020.03.048
Hugosson J, Månsson M, Wallström J et al (2022) Prostate cancer screening with PSA and MRI followed by targeted biopsy only. N Engl J Med 387:2126–2137. https://doi.org/10.1056/NEJMoa2209454
Williams C, Ahdoot M, Daneshvar MA et al (2022) Why does magnetic resonance imaging-targeted biopsy miss clinically significant cancer? J Urol 207:95–107. https://doi.org/10.1097/JU.0000000000002182
Stabile A, Giganti F, Kasivisvanathan V et al (2020) Factors influencing variability in the performance of multiparametric magnetic resonance imaging in detecting clinically significant prostate cancer: a systematic literature review. Eur Urol Oncol 3:145–167. https://doi.org/10.1016/j.euo.2020.02.005
Hao S, Discacciati A, Eklund M et al (2022) Cost-effectiveness of prostate cancer screening using magnetic resonance imaging or standard biopsy based on the STHLM3-MRI study. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2022.5252
Postema A, Mischi M, de la Rosette J, Wijkstra H (2015) Multiparametric ultrasound in the detection of prostate cancer: a systematic review. World J Urol 33:1651–1659. https://doi.org/10.1007/s00345-015-1523-6
Correas J-M, Halpern EJ, Barr RG et al (2021) Advanced ultrasound in the diagnosis of prostate cancer. World J Urol 39:661–676. https://doi.org/10.1007/s00345-020-03193-0
Salib A, Halpern E, Eisenbrey J et al (2022) The evolving role of contrast-enhanced ultrasound in urology: a review. World J Urol. https://doi.org/10.1007/s00345-022-04088-y
Ghai S, Eure G, Fradet V et al (2016) Assessing cancer risk on novel 29 MHz micro-ultrasound images of the prostate: creation of the micro-ultrasound protocol for prostate risk identification. J Urol 196:562–569. https://doi.org/10.1016/j.juro.2015.12.093
Klotz L, Lughezzani G, Maffei D et al (2020) Comparison of micro-ultrasound and multiparametric magnetic resonance imaging for prostate cancer: a multicenter, prospective analysis. Can Urol Assoc J. https://doi.org/10.5489/cuaj.6712
Pavlovich CP, Hyndman ME, Eure G et al (2021) A multi-institutional randomized controlled trial comparing first-generation transrectal high-resolution micro-ultrasound with conventional frequency transrectal ultrasound for prostate biopsy. BJUI Compass 2:126–133. https://doi.org/10.1002/bco2.59
Fusco F, Emberton M, Arcaniolo D et al (2022) Prostatic high-resolution micro-ultrasound: an attractive step-forward in the management of prostate cancer patients. Prostate Cancer Prostatic Dis. https://doi.org/10.1038/s41391-022-00611-9
Cash H, Hofbauer S, Shore N et al (2022) Prostate cancer detection by novice micro-ultrasound users enrolled in a training program. Société Int Urol J 3:62–68. https://doi.org/10.48083/KKVJ7280
Pavlovich CP, Cornish TC, Mullins JK et al (2014) High-resolution transrectal ultrasound: pilot study of a novel technique for imaging clinically localized prostate cancer. Urol Oncol Semin Orig Investig 32:34.e27-34.e32. https://doi.org/10.1016/j.urolonc.2013.01.006
Abouassaly R, Klein EA, El-Shefai A, Stephenson A (2020) Impact of using 29 MHz high-resolution micro-ultrasound in real-time targeting of transrectal prostate biopsies: initial experience. World J Urol 38:1201–1206. https://doi.org/10.1007/s00345-019-02863-y
Claros OR, Tourinho-Barbosa RR, Fregeville A et al (2020) Comparison of initial experience with transrectal magnetic resonance imaging cognitive guided micro-ultrasound biopsies versus established transperineal robotic ultrasound magnetic resonance imaging fusion biopsies for prostate cancer. J Urol 203:918–925. https://doi.org/10.1097/JU.0000000000000692
Wiemer L, Hollenbach M, Heckmann R et al (2021) Evolution of targeted prostate biopsy by adding micro-ultrasound to the magnetic resonance imaging pathway. Eur Urol Focus 7:1292–1299. https://doi.org/10.1016/j.euf.2020.06.022
Rodríguez Socarrás ME, Gomez Rivas J, Cuadros Rivera V et al (2020) Prostate mapping for cancer diagnosis: the madrid protocol. Transperineal prostate biopsies using multiparametric magnetic resonance imaging fusion and micro-ultrasound guided biopsies. J Urol 204:726–733. https://doi.org/10.1097/JU.0000000000001083
Hofbauer SL, Luger F, Harland N et al (2022) A non-inferiority comparative analysis of micro-ultrasonography and MRI-targeted biopsy in men at risk of prostate cancer. BJU Int 129:648–654. https://doi.org/10.1111/bju.15635
Avolio PP, Lughezzani G, Fasulo V et al (2023) Assessing the role of high-resolution microultrasound among naïve patients with negative multiparametric magnetic resonance imaging and a persistently high suspicion of prostate cancer. Eur Urol Open Sci 47:73–79. https://doi.org/10.1016/j.euros.2022.11.015
Cornud F, Lefevre A, Flam T et al (2020) MRI-directed high-frequency (29MhZ) TRUS-guided biopsies: initial results of a single-center study. Eur Radiol 30:4838–4846. https://doi.org/10.1007/s00330-020-06882-x
Pereira-Arias JG, Sánchez-Vázquez A, Gamarra-Quintanilla M, et al ECOGRAFÍA DE ALTA RESOLUCIÓN PROSTÁTICA
Lughezzani G, Maffei D, Saita A et al (2021) Diagnostic accuracy of microultrasound in patients with a suspicion of prostate cancer at magnetic resonance imaging: a single-institutional prospective study. Eur Urol Focus 7:1019–1026. https://doi.org/10.1016/j.euf.2020.09.013
Sountoulides P, Pyrgidis N, Polyzos SA et al (2021) Micro-ultrasound–guided vs multiparametric magnetic resonance imaging-targeted biopsy in the detection of prostate cancer: a systematic review and meta-analysis. J Urol 205:1254–1262. https://doi.org/10.1097/JU.0000000000001639
You C, Li X, Du Y et al (2022) The microultrasound-guided prostate biopsy in detection of prostate cancer: a systematic review and meta-analysis. J Endourol 36:394–402. https://doi.org/10.1089/end.2021.0361
Dias N, Colandrea G, Botelho F et al (2023) Diagnostic accuracy and clinical utility of micro-ultrasound guided biopsies in patients with suspected prostate cancer. Cent Eur J Urol. https://doi.org/10.5173/ceju.2023.198
Ghai S, Perlis N, Atallah C et al (2022) Comparison of micro-US and multiparametric MRI for prostate cancer detection in biopsy-naive men. Radiology 305:390–398. https://doi.org/10.1148/radiol.212163
Lorusso V, Kabre B, Pignot G et al (2022) Comparison between micro-ultrasound and multiparametric MRI regarding the correct identification of prostate cancer lesions. Clin Genitourin Cancer 20:e339–e345. https://doi.org/10.1016/j.clgc.2022.01.013
Avolio PP, Lughezzani G, Paciotti M et al (2021) The use of 29 MHz transrectal micro-ultrasound to stratify the prostate cancer risk in patients with PI-RADS III lesions at multiparametric MRI: a single institutional analysis. Urol Oncol Semin Orig Investig 39:832.e1-832.e7. https://doi.org/10.1016/j.urolonc.2021.05.030
Fasulo V, Buffi NM, Regis F et al (2022) Use of high-resolution micro-ultrasound to predict extraprostatic extension of prostate cancer prior to surgery: a prospective single-institutional study. World J Urol 40:435–442. https://doi.org/10.1007/s00345-021-03890-4
Pedraza AM, Parekh S, Joshi H et al (2023) Side-specific, microultrasound-based nomogram for the prediction of extracapsular extension in prostate cancer. Eur Urol Open Sci 48:72–81. https://doi.org/10.1016/j.euros.2022.12.005
Bhanji Y, Rowe SP, Pavlovich CP (2022) New imaging modalities to consider for men with prostate cancer on active surveillance. World J Urol 40:51–59. https://doi.org/10.1007/s00345-021-03762-x
Eure G, Fanney D, Lin J et al (2018) Comparison of conventional transrectal ultrasound, magnetic resonance imaging, and micro-ultrasound for visualizing prostate cancer in an active surveillance population: a feasibility study. Can Urol Assoc J. https://doi.org/10.5489/cuaj.5361
Albers P, Wang B, Broomfield S et al (2022) Micro-ultrasound versus magnetic resonance imaging in prostate cancer active surveillance. Eur Urol Open Sci 46:33–35. https://doi.org/10.1016/j.euros.2022.09.019
Maffei D, Fasulo V, Avolio PP et al (2023) Diagnostic performance of micro-ultrasound at MRI-guided confirmatory biopsy in patients under active surveillance for low-risk prostate cancer. Prostate. https://doi.org/10.1002/pros.24532
Harland N, Stenzl A (2021) Micro-ultrasound: a way to bring imaging for prostate cancer back to urology. Prostate Int 9:61–65. https://doi.org/10.1016/j.prnil.2020.12.002
Basso Dias A, Ghai S (2023) Micro-ultrasound: current role in prostate cancer diagnosis and future possibilities. Cancers 15:1280. https://doi.org/10.3390/cancers15041280
Calace FP, Napolitano L, Arcaniolo D et al (2022) Micro-ultrasound in the diagnosis and staging of prostate and bladder cancer: a comprehensive review. Medicina (Mex) 58:1624. https://doi.org/10.3390/medicina58111624
Klotz L, Andriole G, Cash H et al (2022) Optimization of prostate biopsy—micro-ultrasound versus MRI (OPTIMUM): a 3-arm randomized controlled trial evaluating the role of 29 MHz micro-ultrasound in guiding prostate biopsy in men with clinical suspicion of prostate cancer. Contemp Clin Trials 112:106618. https://doi.org/10.1016/j.cct.2021.106618
Funding
Rafael Sanchez-Salas certifies that this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
PPA contributed to project development, data collection, and manuscript writing. GGL contributed to project development and manuscript writing. MA contributed to manuscript writing. TH contributed to data collection. AR-B contributed to manuscript writing. NMB contributed to manuscript writing. ML contributed to manuscript writing. RS-S contributed to project development and manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
Rafael Sanchez-Salas certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (e.g., employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patent filed, received, or pending), are the following: Nothing to disclose.
Research involving human participants and/or animals
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Avolio, P.P., Lughezzani, G., Anidjar, M. et al. The diagnostic accuracy of micro-ultrasound for prostate cancer diagnosis: a review. World J Urol 41, 3267–3276 (2023). https://doi.org/10.1007/s00345-023-04521-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04521-w