Abstract
Diffuse alveolar haemorrhage (DAH) secondary to anti-neutrophil cytoplasmic antibodies (ANCA)-associated vasculitis (AAV) is a rare life-threatening condition presenting with severe respiratory failure. The management of AAV-related DAH consists of remission induction immunosuppressive therapy, which requires time to be effective, with significant fatality rates despite appropriate treatment. Extracorporeal membrane oxygenation (ECMO) can support gas exchanges providing the time necessary for immunosuppressive treatment to control the underlying disease in cases refractory to the conventional ventilation techniques. Despite severe preexisting bleeding has been considered a relative contraindication, ECMO has proven to be life-saving in several cases of respiratory failure associated with pulmonary haemorrhage due to various causes, including AAV. We reviewed the clinical presentation and course of two patients affected by AAV-related DAH treated at our Institution between 2012 and 2017, whose management required the use of veno-venous ECMO. We reviewed the current literature on the role of ECMO in the support of these patients. In both patients, ECMO provided life support and allowed disease control, in combination with immunosuppressive treatment. Despite systemic anticoagulation, clinical improvement was achieved without exacerbation of the pulmonary bleeding. We performed a literature review, and summarized available data confirming the effectiveness and safety of ECMO in AAV-related DAH. ECMO has a life-saving role in the management of patients with severe respiratory failure due to ANCA-associated pulmonary capillaritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anti-neutrophil cytoplasmic antibodies (ANCA)-associated vasculitides (AAV) are a group of systemic disorders characterized by inflammation and necrosis of small-and-medium-size vessels. Although most organs can be affected, pulmonary involvement is one of the most frequent manifestations. Every level of the pulmonary vasculature may be damaged, with a predilection for pulmonary capillaries. The derangement of the alveolar basement membrane resulting from the widespread injury of the pulmonary capillaries promotes the extravasation of red blood cells into the pulmonary alveolar spaces. This condition, known as diffuse alveolar haemorrhage (DAH), is one of the most serious complications and one of the strongest predictors of early mortality in the course of AAV [1, 2], with 1-year mortality rate varying between 18 and 50% [3, 4]. Extracorporeal membrane oxygenation (ECMO) is a tool that provides life support in case of severe acute respiratory failure refractory to the conventional ventilation approaches [5, 6]. ECMO was introduced in 1972 for the support of respiratory failure of the newborns and, since then, has been applied to an increasing number of complex conditions [7, 8]. Veno-arterial ECMO (VA-ECMO) is used in cardiac or cardiorespiratory failure, while veno-venous ECMO (VV-ECMO) is employed in respiratory failure without cardiac compromise, offering temporary life support. Recent technological advances have made AAV-related DAH a potential indication for ECMO, even if a certain degree of systemic anticoagulation is required, which represents an issue of concern in case of DAH. Therefore, balancing risks and benefits is crucial, as supporting gas exchanges and sparing time for immunosuppressive agents to explicate their effect are counterbalanced by the need for anticoagulation in the course of a major bleeding.
Methods and search strategy
Here, we describe the clinical presentation and management of two patients, affected by AAV, who presented with severe respiratory failure refractory to the conventional ventilation techniques treated at Policlinico San Matteo, Pavia, in 2012 and 2017, respectively. Written informed consent was obtained from involved patients. We performed a review of the available literature concerning the role of ECMO in the treatment of AAV-related DAH. We searched PubMed for English-language sources, from inception until January 2018, combining the following keywords: extracorporeal membrane oxygenation and ANCA-associated vasculitides or vasculitis. We identified 20 cases of DAH secondary to AAV supported with ECMO, six of which were excluded due to lack of complete clinical data.
Case descriptions
Case 1
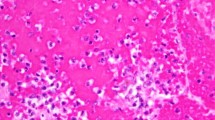
A 45-year-old woman with a 20-day history of polyarthralgia developed acute dyspnea and hemoptysis. She was conducted to the Accident and Emergency Department (A&E) and admitted to the Division of Infectious Diseases. She then developed fever > 38 °C and progressive anemia, with raised acute-phase reactants. Laboratory findings at presentation and during follow-up are shown in Table 1. Although antimicrobial therapy was initiated, the patient’s general conditions worsened with the onset of acute respiratory failure. A chest CT scan showed diffuse ground-glass opacities suggestive of acute respiratory distress syndrome (ARDS) (Fig. 1a). The blood gas exchange parameters were remarkably impaired (pH 7.25, PaO2 49.5 mmHg, PaCO2 63.7 mmHg), and thus, the patient was transferred to the Intensive Care Unit (ICU), intubated, and mechanically ventilated. Bronchial fibroscopy (BFS) revealed active bronchial bleeding, with negative bronchoalveolar lavage (BAL) fluid microbiological tests. Further anemization required the transfusion of 3 units of RBC. For persistent hypoxemia refractory to mechanical ventilation, a full VV-ECMO support was initiated. Immunological tests showed c-ANCA (PR3) positivity (Table 1) and rose suspicion of AAV-related DAH. Therefore, the patient was treated with methylprednisolone (MP) pulses (1 g intravenously/day on 3 consecutive days), plasma exchange (PE), and cyclophosphamide (CyC) pulses. Chest CT scan performed after 8 days demonstrated progressive improvement of lung transparency and resolution of the alveolar bleeding (Fig. 1b). Regular blood gas estimation revealed gradual improvement of respiratory function (Fig. 2) and ECMO support was stopped after 6 days. On day 13, the patient was transferred to our Rheumatology Unit and was discharged from hospital care 23 days later. She completed the remission induction treatment with 6 monthly CyC pulses (1500 mg/month intravenously). After remission achievement and steroid tapering, maintenance immunosuppressive treatment with azathioprine 2 mg/kg/day was started. Steroid treatment and azathioprine were withdrawn after 2 and 3 years, respectively, with clinical stationarity and normal blood acute-phase proteins, despite persistent c-ANCA (PR3)-positivity (Table 1). A recent CT chest scan showed complete resolution of pathological findings (Fig. 1c).
Case 2
In September 2015, a 45-year-old man was admitted to our Rheumatology Unit reporting a 30-day history of ear, nose, and throat (ENT) manifestations, lower limbs oligoarthritis, and tinglings. Laboratory tests and urine sediment analysis at presentation and during follow-up are shown in Table 1. C-ANCA (PR3) antibodies were detected. Electroneurography showed abnormal pattern suggestive of minimal axonal sensorimotor polyneuropathy. Granulomatosis with polyangiitis (GPA) was diagnosed and treatment with prednisone 37.5 mg/day and methotrexate 15 mg/week was initiated, with achievement of clinical remission and ANCA negativisation. Prednisone was gradually tapered. In February 2017, after 1 year of stable disease, the patient presented with low-grade fever, arthralgia, and recurrent ENT symptoms. Laboratory findings revealed increased acute-phase reactants and signs of renal involvement (Table 1). The patient was admitted to our Rheumatology Unit. Blood chemistry showed further worsening of renal function associated with c-ANCA (PR3) positivity (Table 1) and urinary sediment analysis was suggestive of acute glomerulopathy (Table 1). MP pulse therapy (1 g intravenously/day on 3 consecutive days) tapered to oral MP 1 mg/kg/day was started, followed by intravenous CyC (12,5 mg/kg according to EUVAS scheme [9, 10] adjusted for glomerular filtration rate [11]). Hemodialytic replacement therapy was required. Renal biopsy confirmed pauci-immune rapid progressive glomerulonephritis (RPGN). Pulmonary high-resolution CT (HRCT) showed numerous, bilateral nodules localized to the upper and lower pulmonary lobes, consistent with pulmonary involvement of GPA. For the collateral finding of thrombosis of the right inner jugular vein, and site of temporary central venous catheter (CVC), anticoagulation was started. The patient was discharged and continued renal replacement therapy and CyC pulses on the Day-care ward. A few hours after the fourth CyC infusion, the patient was conducted to A&E reporting nausea and hematemesis. On admission, he developed worsening type II respiratory failure (pH 7.28, PaO2 57.8 mmHg, PaCO2 56.3 mmHg), progressive anemia, and acute on chronic kidney disease (Table 1). Two units of RBC were transfused. Chest CT scan revealed diffuse pulmonary consolidations, suggestive of massive alveolar haemorrhage (Fig. 3a). The patient was intubated, transferred to the ICU, and mechanically ventilated. BFS showed copious lower airways bleeding. Because of further worsening of gas exchange, a full VV-ECMO support was started, with quick restoration of the patient’s oxygen saturation. Considering the anti-PR3-positivity (Table 1) and negative BAL microbiological investigations, the suspicion of GPA-related DAH was confirmed and the patient was treated with MP pulse therapy (1 g intravenously/day on 3 consecutive days), followed by rescue therapy with rituximab (RTX) (375 mg/m2/week on 4 consecutive weeks). Hemodialytic sessions were maintained on a regular basis. During ECMO support, respiratory function significantly improved (Fig. 4) even though the patient developed subcutaneous emphysema and an abdominal hematoma successfully treated with percutaneous thrombin injection. On day 14, ECMO was discontinued. A pulmonary HRCT performed after 17 days revealed gradual improvement of pulmonary ventilation and reabsorption of the alveolar haemorrhage (Fig. 3b). On day 32, the patient was transferred to our Unit and discharged 26 days later. In the following weeks the patient’s general conditions remarkably improved and good pulmonary function was restored. Haemodyalitic sessions were withdrawn with stable renal function (Table 1). A chest CT scan performed in October 2017 revealed the complete resolution of the pulmonary consolidations, with fine residual fibrotic striae (Fig. 3c). In November 2017 maintenance immunosuppressive treatment with rituximab (500 mg/6 months) was started, with persistent clinical remission and ANCA negativity (both IIF and EIA).
Discussion
Hereby, we described two patients affected by severe respiratory failure secondary to AAV-related DAH, whose prognosis would have been poor without the use of ECMO. In both patients, ECMO provided time for life-saving treatments to explicate their effect in halting the pathologic process. No exacerbation of alveolar haemorrhage occurred and the active bleeding stopped after initiating ECMO. With the conventional ventilation, neither of them was likely to survive long enough for the immunosuppressive therapy to be effective.
DAH is a life-threatening condition that can complicate the course of AAV with a protean clinical presentation, ranging from acute respiratory failure to a more subtle course. Although most patients develop a certain degree of hemoptysis, this symptom is missing in about one-third of cases. Constitutional symptoms, cough, dyspnea, and chest pain may occur [12], whereas fall of haemoglobin is a common laboratory finding [13]. The co-existence of DAH and acute glomerulonephritis is typically defined as pulmonary renal syndrome. Although radiological findings are nonspecific and variable with time of onset of the haemorrhage, imaging studies, especially pulmonary HRCT, may provide additional information. Typical patterns can range from lobular or lobar areas of ground-glass opacities to predominant consolidation as a consequence of alveolar filling. Throughout the resolution of the acute haemorrhage, interlobular septal thickening superimposed on areas of ground-glass opacity may give rise to a “crazy-paving” pattern [14]. Nevertheless, additional laboratory tests and bronchoscopy with BAL are necessary, due to the low specificity of symptoms and clinical–radiological signs. BFS with BAL is mandatory to confirm the intra-alveolar haemorrhage and rule out infections or bleeding lesions in the upper airways. An increasingly haemorrhagic appearance of consecutive BAL aliquots and BAL iron staining showing more than 20% hemosiderin-laden macrophages (HLM) are highly suggestive for DAH [15]. DAH represents the main cause for hospitalization and ICU admission in AAV [16, 17]. In a previous case series, we described 90 patients affected by AAV, 10 of whom experienced a life-threatening disease onset manifestation leading to diagnosis in the ICU setting [18]. Cardio-pulmonary acute involvement was the main cause for ICU admission, accounting for 70% of cases, with DAH representing the leading cause of respiratory failure. Treatment of AAV-related DAH should be guided by the recommendations for the management of new onset organ-threatening or life-threatening disease. Remission induction schemes proposed by the recently updated EULAR/ERA-EDTA recommendations suggest a combination of high-dose glucocorticoids (GC) and either CyC or RTX [19]. In case of a major relapse of organ-threatening or life-threatening AAV, treatment as per new disease is recommended.
Although immunosuppressive treatment has significantly increased the survival rate in patients affected by AAV, supportive approaches for complications affecting vital organs may be necessary. ECMO is an advanced circulatory and ventilatory support system used as salvage therapy for patients with refractory hypoxemia and/or cardiac failure when the conventional treatment fails [20]. During severe respiratory failure unresponsive to the conventional mechanical ventilation, ECMO can be applied, preventing severe hypoxia and removing carbon dioxide until the restoration of the pulmonary function. Recent developments in ECMO technology [5, 21] have reduced complications associated with this procedure, safely extending its employment to other life-threatening conditions, including trauma, cardio-pulmonary resuscitation, and interstitial lung diseases [7, 8]. Despite the increased application of ECMO for severe respiratory failure over the last years, its effectiveness is still controversial. In a recent international, randomized trial involving 249 patients presenting with severe ARDS (mainly due to infectious causes), 60-day mortality was not significantly lower with ECMO compared with the conventional treatment, a strategy which included crossover to ECMO in case of refractory hypoxemia [22]. Further studies are needed to clarify the effective role of ECMO in the support of severe respiratory failure unresponsive to mechanical ventilation. Because of the rarity and the high mortality rate of DAH secondary to AAV, the evidence for the use of ECMO in this condition is restricted to a small number of case reports [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43]. We performed a review of the current literature concerning the role of ECMO in the management of AAV-related DAH. Fourteen case descriptions provided with comprehensive clinical data are summarized in Tables 2 and 3. DAH occurred at disease onset in all cases. ANCA were positive in all cases, anti-PR3/anti-MPO positivity: 78.6%/21.4%. As soon as life-threatening AAV was suspected, remission induction therapy with a combination of high-dose GC and immunosuppressive agents (CyC or RTX) was started in 13 cases (92.8%). Four patients (28.6%) also received adjuvant treatment with intravenous immunoglobulin. Twelve patients (85.7%) underwent PE and nine (64.3%) required renal replacement therapy because of RPGN. The mean duration of ECMO support was 10.1 ± 4.8 days, in line with our two case descriptions (respectively 6 and 14 days). All patients survived and were discharged from hospital care. The patients described above did not receive the same protocol of CyC. In case 1, diagnosed and treated few years previously, remission induction regimen was represented by 6 monthly CyC pulses (1500 mg/month) [44]. Nevertheless, cumulative dose of CyC was similar compared to EUVAS scheme and this approach resulted in an excellent clinical response, demonstrated by the persistence of sustained drug-free remission. In case 2, our patient developed DAH following CyC administration. Due to the concomitant kidney involvement, AAV-related DAH was suspected and promptly treated. Nevertheless, differential diagnosis should take into account the very rare occurrence of CyC-induced lung toxicity, which has been anecdotally reported [45, 46].
Despite its life-saving potential, ECMO enhances an inflammatory response, resulting in a pro-thrombotic state, which requires anticoagulation to prevent thromboembolism developing in the non-endothelial surfaced circuit. Bleeding is the main complication in patients undergoing ECMO. Risk factors include constant anticoagulation therapy and coagulopathy secondary to clotting factors consumption [47,48,49]. The use of heparin-coated ECMO has proved to reduce the daily blood loss, the amount of RBC infusion, and the intravenous heparin dose [21]. Although ECMO has no absolute contraindications, conditions with a significant risk of bleeding or preexisting severe bleeding have been considered relative contraindications. Therefore, balancing harms and benefits of single patient is crucial. On one hand, the occurrence of DAH may represent an issue of concern for ECMO application, as systemic heparinization may exacerbate the pulmonary bleeding; on the other hand, sparing time for the immunosuppressive treatment to be effective can be life-saving in the course of AAV-related DAH. Moreover, ECMO may explicate a direct beneficial effect during DAH, as it allows a significant decrease in ventilator flow rate. Notwithstanding, with the exception of a patient who developed hemothorax in the site of a chest tube inserted for pneumothorax and a case of asymptomatic heparin-induced thrombocytopenia, no bleeding events occurred among AAV-related DAH requiring ECMO reported in the literature. In one of our cases, the course in ICU was complicated by an abdominal hematoma successfully treated with percutaneous thrombin injection. Our cases demonstrate how a prompt referral by intensivists and A&E physicians to specialist hospitals to allow the early initiation of ECMO can dramatically improve the clinical outcome.
Conclusions
DAH is a life-threatening condition requiring prompt immunosuppressive treatment, which, however, needs time to explicate its effect. ECMO can support gas exchanges, providing the time necessary for induction immunosuppressive treatment to control the underlying disease. In our case series, ECMO supported the respiratory function, permitting the management of pulmonary bleeding, the improvement of radiologic findings, with consequent weaning of the extracorporeal circulation and extubation. No life-threatening bleeding events occurred during ECMO. Although ECMO is a highly invasive procedure with a significant risk of bleeding complications, it should be considered in patients with AAV-related DAH when the conventional mechanical ventilation has failed.
References
Hogan SL, Nachman PH, Wilkman AS, Jennette JC, Falk RJ (1996) Prognostic markers in patients with antineutrophil cytoplasmic autoantibody-associated microscopic polyangiitis and glomerulonephritis. J Am Soc Nephrol 7(1):23–32
Haworth SJ, Savage CO, Carr D, Hughes JM, Rees AJ (1985) Pulmonary haemorrhage complicating Wegener’s granulomatosis and microscopic polyarteritis. BMJ (Clin Res Ed) 290(6484), 1775–1778
Lauque D, Cadranel J, Lazor R, Pourrat J, Ronco P, Guillevin L, Cordier JF (2000) Microscopic polyangiitis with alveolar hemorrhage. A study of 29 cases and review of the literature. Groupe d’Etudes et de Recherche sur les Maladies “Orphelines” Pulmonaires (GERM"O"P). Medicine 79(4):222–233
Gallagher H, Kwan JTC, Jayne DRW (2002) Pulmonary renal syndrome: a 4-year, single-center experience. Am J Kidney Dis 39(1):42–47
Lewandowski K (2000) Extracorporeal membrane oxygenation for severe acute respiratory failure. Crit Care 4(3):156–168
Tulman DB, Stawicki SPA, Whitson BA, Gupta SC, Tripathi RS, Firstenberg MS et al (2014) Veno-venous ECMO: a synopsis of nine key potential challenges, considerations, and controversies. BMC Anesthesiol 14:65
Cordell-Smith JA, Roberts N, Peek GJ, Firmin RK (2006) Traumatic lung injury treated by extracorporeal membrane oxygenation (ECMO). Injury 37(1):29–32
Shin TG, Choi J-H, Jo IJ, Sim MS, Song HG, Jeong YK et al (2011) Extracorporeal cardiopulmonary resuscitation in patients with inhospital cardiac arrest: a comparison with conventional cardiopulmonary resuscitation. Crit Care Med 39(1):1–7
Adu D, Pall A, Luqmani RA, Richards NT, Howie AJ, Emery P et al (1997) Controlled trial of pulse versus continuous prednisolone and cyclophosphamide in the treatment of systemic vasculitis. QJM 90(6):401–409
Rihová Z, Jancová E, Merta M, Zabka J, Rysavá R, Bartůnková J et al (2004) Daily oral versus pulse intravenous cyclophosphamide in the therapy of ANCA-associated vasculitis—preliminary single center experience. Prague Med Rep 105(1):64–68
Haubitz M, Bohnenstengel F, Brunkhorst R, Schwab M, Hofmann U, Busse D (2002) Cyclophosphamide pharmacokinetics and dose requirements in patients with renal insufficiency. Kidney Int 61(4):1495–1501
Krause ML, Cartin-Ceba R, Specks U, Peikert T (2012) Update on diffuse alveolar hemorrhage and pulmonary vasculitis. Immunol Allergy Clin North Am 32(4):587–600
Cordier J-F, Cottin V (2011) Alveolar hemorrhage in vasculitis: primary and secondary. Semin Respir Crit Care Med 32(3):310–321
Hansell DM (2002) Small-vessel diseases of the lung: CT-pathologic correlates. Radiology 225(3):639–653
De Lassence A, Fleury-Feith J, Escudier E, Beaune J, Bernaudin JF, Cordonnier C (1995) Alveolar hemorrhage. Diagnostic criteria and results in 194 immunocompromised hosts. Am J Respir Crit Care Med 151(1):157–163
Janssen NM, Karnad DR, Guntupalli KK (2002) Rheumatologic diseases in the intensive care unit: epidemiology, clinical approach, management, and outcome. Crit Care Clin 18(4):729–748
Quintero OL, Rojas-Villarraga A, Mantilla RD, Anaya J-M (2013) Autoimmune diseases in the intensive care unit. An update. Autoimmun Rev 12(3):380–395
Monti S, Montecucco C, Pieropan S, Mojoli F, Braschi A, Caporali R (2015) Life-threatening onset of systemic vasculitis requiring intensive care unit admission: a case series. Clin Exp Rheumatol 33(2 Suppl 89):S–S126
Yates M, Watts RA, Bajema IM, Cid MC, Crestani B, Hauser T et al (2016) EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann Rheum Dis 75(9):1583–1594
Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM et al (2009) Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet 374(9698):1351–1363
Knoch M, Köllen B, Dietrich G, Müller E, Mottaghy K, Lennartz H (1992) Progress in veno-venous long-term bypass techniques for the treatment of ARDS. Controlled clinical trial with the heparin-coated bypass circuit. Int J Artif Organs 15(2):103–108
Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C et al (2018) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med 378(21):1965–1975
Hartmann A, Nordal KP, Svennevig J, Noddeland H, Pedersen T, Skarbøvik AJ et al (1994) Successful use of artificial lung (ECMO) and kidney in the treatment of a 20-year-old female with Wegener’s syndrome. Nephrol Dial Transplant 9(3):316–319
Loscar M, Hummel T, Haller M, Briegel J, Wiebecke B, Samtleben W et al (1997) ARDS and Wegener granulomatosis. Der Anaesthesist 46(11):969–973
Matsumoto T, Ueki K, Tamura S, Ideura H, Tsukada Y, Maezawa A et al (2000) Extracorporeal membrane oxygenation for the management of respiratory failure due to ANCA-associated vasculitis. Scand J Rheumatol 29(3):195–197
Mikami M, Mori Y, Yamazaki A, Konta A, Saito D, Owada S (2000) Efficacy of the extra-corporeal lung assist (ECLA) on the alveolar hemorrhage in a case with microscopic polyarteritis nodosa. Nihon Naika Gakkai Zasshi J Jpn Soc Internal Med 89(8):1651–1653
Hernandez MEC, Lovrekovic G, Schears G, Helfaer M, Friedman D, Stafford P et al (2002) Acute onset of Wegener’s granulomatosis and diffuse alveolar hemorrhage treated successfully by extracorporeal membrane oxygenation. Pediatr Crit Care Med 3(1):63–66
Rosengarten A, Elmore P, Epstein J (2002) Long distance road transport of a patient with Wegener’s granulomatosis and respiratory failure using extracorporeal membrane oxygenation. Emerg Med (Fremantle) 14(2):181–187
Ahmed SH, Aziz T, Cochran J, Highland K (2004) Use of extracorporeal membrane oxygenation in a patient with diffuse alveolar hemorrhage. Chest 126(1):305–309
Agarwal HS, Taylor MB, Grzeszczak MJ, Lovvorn HN, Hunley TE, Jabs K et al (2005) Extra corporeal membrane oxygenation and plasmapheresis for pulmonary hemorrhage in microscopic polyangiitis. Pediatr Nephrol 20(4):526–528
Balasubramanian SK, Tiruvoipati R, Chatterjee S, Sosnowski A, Firmin RK (2005) Extracorporeal membrane oxygenation with lepirudin anticoagulation for Wegener’s granulomatosis with heparin-induced thrombocytopenia. ASAIO J 51(4):477–479
Di Maria MV, Hollister R, Kaufman J (2008) Case report: severe microscopic polyangiitis successfully treated with extracorporeal membrane oxygenation and immunosuppression in a pediatric patient. Curr Opin Pediatr 20(6):740–742
Zhong H, Chen J, Li S, Jiang L, Li X, Han B (2008) Extracorporeal membrane oxygenation for pulmonary hemorrhage in microscopic polyangiitis. Chin Med J 121(24):2622–2623
Guo Z, Li X, Jiang L-Y, Xu L-F (2009) Extracorporeal membrane oxygenation for the management of respiratory failure caused by diffuse alveolar hemorrhage. J Extra Corpor Technol 41(1):37–40
Paden ML, Warshaw BL, Heard ML, Fortenberry JD (2011) Recovery of renal function and survival after continuous renal replacement therapy during extracorporeal membrane oxygenation. Pediatr Crit Care Med 12(2):153–158
Joseph M, Charles AG (2011) Early extracorporeal life support as rescue for Wegener granulomatosis with diffuse alveolar hemorrhage and acute respiratory distress syndrome: a case report and literature review. Pediatr Emerg Care 27(12):1163–1166
Barnes SL, Naughton M, Douglass J, Murphy D (2012) Extracorporeal membrane oxygenation with plasma exchange in a patient with alveolar haemorrhage secondary to Wegener’s granulomatosis. Internal Med J 42(3):341–342
Keller R, Torres S, Iölster T, Kreutzer C, Fraire R, Grassi M et al (2012) Extracorporeal membrane oxygenation and plasmapheresis in the treatment of severe pulmonary hemorrhage secondary to nodose polyarteritis. Arch Argent Pediatr 110(4):e80–e85
Hohenforst-Schmidt W, Petermann A, Visouli A, Zarogoulidis P, Darwiche K, Kougioumtzi I et al (2013) Successful application of extracorporeal membrane oxygenation due to pulmonary hemorrhage secondary to granulomatosis with polyangiitis. Drug Des Devel Ther 7:627–633
Yusuff H, Malagon I, Robson K, Parmar J, Hamilton P, Falter F (2015) Extracorporeal membrane oxygenation for Life-threatening ANCA-positive pulmonary capillaritis. A review of UK experience. Heart Lung Vessel 7(2):159–167
Rawal G, Kumar R, Yadav S (2016) ECMO rescue therapy in diffuse alveolar haemorrhage: a case report with review of literature. J Clin Diagn Res 10(6):OD10–O11
Vanoli J, Riva M, Vergnano B, D’Andrea G, L’Imperio V, Pozzi MR et al (2017) Granulomatosis with polyangiitis presenting with diffuse alveolar hemorrhage requiring extracorporeal membrane oxygenation with rapid multiorgan relapse: a case report. Medicine, 96(13), e6024
Kelly D, Makkuni D, Ail D (2017) Rare cause of respiratory failure in a young woman: isolated diffuse alveolar haemorrhage requiring extracorporeal membrane oxygenation. BMJ Case Rep. https://doi.org/10.1136/bcr-2017-219235
Reinhold-Keller E, Kekow J, Schnabel A, Schmitt WH, Heller M, Beigel A et al (1990) Influence of disease manifestation and antineutrophil cytoplasmic antibody titer on the response to pulse cyclophosphamide therapy in patients with Wegener’s granulomatosis. Arthritis Rheum 37(6):919–924
Myers JL (1993) Diagnosis of drug reactions in the lung. Monogr Pathol 36:32–53
Malik SW, Myers JL, DeRemee RA, Specks U (1996) Lung toxicity associated with cyclophosphamide use. Two distinct patterns. Am J Respir Crit Care Med 154(6 Pt 1):1851–1856
Uziel L, Cugno M, Fabrizi I, Pesenti A, Gattinoni L, Agostoni A (1990) Physiopathology and management of coagulation during long-term extracorporeal respiratory assistance. Int J Artif Organs 13(5):280–287
Brunet F, Belghith M, Mira JP, Lanore JJ, Vaxelaire JF, Dall’ava Santucci J et al (1993) Extracorporeal carbon dioxide removal and low-frequency positive-pressure ventilation. Improvement in arterial oxygenation with reduction of risk of pulmonary barotrauma in patients with adult respiratory distress syndrome. Chest 104(3):889–898
McCoy-Pardington D, Judd WJ, Knafl P, Abruzzo LV, Coombes KR, Butch SH et al (1990) Blood use during extracorporeal membrane oxygenation. Transfusion 30(4):307–309
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Delvino, P., Monti, S., Balduzzi, S. et al. The role of extra-corporeal membrane oxygenation (ECMO) in the treatment of diffuse alveolar haemorrhage secondary to ANCA-associated vasculitis: report of two cases and review of the literature. Rheumatol Int 39, 367–375 (2019). https://doi.org/10.1007/s00296-018-4116-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-018-4116-z