Abstract
Brain aging is a complex process involving many functions of our body and described by the interplay of a sleep pattern and changes in the metabolic waste concentration regulated by the microglial function and the glymphatic system. We review the existing modelling approaches to this topic and derive a novel mathematical model to describe the crosstalk between these components within the conceptual framework of inflammaging. Analysis of the model gives insight into the dynamics of garbage concentration and linked microglial senescence process resulting from a normal or disrupted sleep pattern, hence, explaining an underlying mechanism behind healthy or unhealthy brain aging. The model incorporates accumulation and elimination of garbage, induction of glial activation by garbage, and glial senescence by over-activation, as well as the production of pro-inflammatory molecules by their senescence-associated secretory phenotype (SASP). Assuming that insufficient sleep leads to the increase of garbage concentration and promotes senescence, the model predicts that if the accumulation of senescent glia overcomes an inflammaging threshold, further progression of senescence becomes unstoppable even if a normal sleep pattern is restored. Inverting this process by “rejuvenating the brain” is only possible via a reset of concentration of senescent glia below this threshold. Our model approach enables analysis of space-time dynamics of senescence, and in this way, we show that heterogeneous patterns of inflammation will accelerate the propagation of senescence profile through a network, confirming a negative effect of heterogeneity.



Similar content being viewed by others
References
Kennedy BK, Berger SL, Brunet A, Campisi J, Cuervo AM, Epel ES, Franceschi C, Lithgow GJ, Morimoto RI, Pessin JE, Rando TA, Richardson A, Schadt EE, Wyss-Coray T, Sierra F (2014) Geroscience: Linking aging to chronic disease. Cell 159(4):709–713
Whitwell HJ, Bacalini MG, Blyuss O, Chen S, Garagnani P, Gordleeva SY, Jalan S, Ivanchenko M, Kanakov O, Kustikova V, Mariño IP, Meyerov I, Ullner E, Franceschi C, Zaikin A (2020) The human body as a super network: Digital methods to analyze the propagation of aging. Front Aging Neurosci 12:136
Mander BA, Winer JR, Walker MP (2017) Sleep and human aging. Neuron 94(1):19–36
Sundaram S, Hughes RL, Peterson E, Müller-Oehring EM, Brontë-Stewart HM, Poston KL, Faerman A, Bhowmick C, Schulte T (2019) Establishing a framework for neuropathological correlates and glymphatic system functioning in Parkinson’s disease. Neuroscience & Biobehavioral Reviews 103:305–315
Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O’Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T, Deane R, Nedergaard M (2013) Sleep drives metabolite clearance from the adult brain. Science 342:373–377
Jessen NA, Munk A SF, Lundgaard I, Nedergaard M (2015) The glymphatic system: A beginner’s guide. Neurochem Res 40(12):2583–2599
Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, Benveniste H, Vates GE, Deane R, Goldman SA, Nagelhus EA, Nedergaard M (2012) A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med 4(147):147ra111–147ra111
Iliff JJ, Nedergaard M (2013) Is there a cerebral lymphatic system?. Stroke 44(6, Supplement 1):S93–S95
Kress BT, Iliff JJ, Xia M, Wang M, Wei HS, Zeppenfeld D, Xie L, Kang H, Xu Q, Liew JA, Plog BA, Ding F, Deane R, Nedergaard M (2014) Impairment of paravascular clearance pathways in the aging brain. Ann Neurol 76(6):845–861
Verheggen ICM, Boxtel MPJV, Verhey FRJ, Jansen JFA, Backes WH (2018) Interaction between blood-brain barrier and glymphatic system in solute clearance. Neuroscience & Biobehavioral Reviews 90:26–33
Tarasoff-Conway JM, Carare RO, Osorio RS, Glodzik L, Butler T, Fieremans E, Axel L, Rusinek H, Nicholson C, Zlokovic BV, Frangione B, Blennow K, Ménard J, Zetterberg H, Wisniewski T, deLeon MJ (2015) Clearance systems in the brain — implications for Alzheimer disease. Nat Rev Neurol 11(8):457–470
Abbott NJ, Patabendige AAK, Dolman DEM, Yusof SR, Begley DJ (2010) Structure and function of the blood–brain barrier. Neurobiol Dis 37(1):13–25
Yin K-J, Cirrito JR, Yan P, Hu X, Xiao Q, Pan X, Bateman R, Song H, Hsu F-F, Turk J, Xu J, Hsu CY, Mills JC, Holtzman DM, Lee J-M (2006) Matrix metalloproteinases expressed by astrocytes mediate extracellular amyloid-beta peptide catabolism. J Neurosci 26(43):10939–10948
Wilcock DM, Munireddy SK, Rosenthal A, Ugen KE, Gordon MN, Morgan D (2004) Microglial activation facilitates Aβ plaque removal following intracranial anti-Aβ antibody administration. Neurobiol Dis 15(1):11–20
Hawkes CA, McLaurin J (2009) Selective targeting of perivascular macrophages for clearance of β-amyloid in cerebral amyloid angiopathy. Proceedings of the National Academy of Sciences 106(4):1261–1266
Morrone CD, Liu M, Black SE, McLaurin J (2015) Interaction between therapeutic interventions for Alzheimer’s disease and physiological Aβ clearance mechanisms. Front Aging Neurosci 7:64
Salter MW, Stevens B (2017) Microglia emerge as central players in brain disease. Nat Med 23(9):1018–1027
Tay TL, Savage JC, Hui CW, Bisht K, Tremblay M-E (2016) Microglia across the lifespan: from origin to function in brain development, plasticity and cognition. The Journal of Physiology 595 (6):1929–1945
Kierdorf K, Prinz M (2017) Microglia in steady state. J Clin Investig 127(9):3201–3209
Niraula A, Sheridan JF, Godbout JP (2016) Microglia priming with aging and stress. Neuropsychopharmacology 42(1):318–333
Ritzel RM, Patel AR, Pan S, Crapser J, Hammond M, Jellison E, McCullough LD (2015) Age- and location-related changes in microglial function. Neurobiol Aging 36(6):2153–2163
Clarke LE, Liddelow SA, Chakraborty C, Münch AE, Heiman M, Barres BA (2018) Normal aging induces A1-like astrocyte reactivity. Proceedings of the National Academy of Sciences 115 (8):E1896–E1905
Mullington JM, Simpson NS, Meier-Ewert HK, Haack M (2010) Sleep loss and inflammation. Best Practice & Research Clinical Endocrinology & Metabolism 24(5):775–784
Hurtado-Alvarado G, Pavón L, Castillo-García SA, Hernández ME, Domínguez-Salazar E, Velázquez-Moctezuma J, Gómez-González B (2013) Sleep loss as a factor to induce cellular and molecular inflammatory variations. Clin Dev Immunol 2013:1–14
Irwin MR, Olmstead R, Carroll JE (2016) Sleep disturbance, sleep duration, and inflammation: A systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry 80 (1):40–52
Bellesi M, deVivo L, Chini M, Gilli F, Tononi G, Cirelli C (2017) Sleep loss promotes astrocytic phagocytosis and microglial activation in mouse cerebral cortex. The Journal of Neuroscience 37 (21):5263–5273
Perry VH, Holmes C (2014) Microglial priming in neurodegenerative disease. Nat Rev Neurol 10(4):217–224
Boespflug EL, Iliff JJ (2018) The emerging relationship between interstitial fluid-cerebrospinal fluid exchange, amyloid-β, and sleep. Biological psychiatry 83:328–336
Carroll JE, Cole SW, Seeman TE, Breen EC, Witarama T, Arevalo JMG, Ma J, Irwin MR (2016) Partial sleep deprivation activates the DNA damage response (DDR) and the senescence-associated secretory phenotype (SASP) in aged adult humans. Brain Behav Immun 51:223–229
Ritzel RM, Doran SJ, Glaser EP, Meadows VE, Faden AI, Stoica BA, Loane DJ (2019) Old age increases microglial senescence, exacerbates secondary neuroinflammation, and worsens neurological outcomes after acute traumatic brain injury in mice. Neurobiol Aging 77:194–206
Baker DJ, Petersen RC (2018) Cellular senescence in brain aging and neurodegenerative diseases: evidence and perspectives. The Journal of clinical investigation 128:1208–1216
Salminen A, Ojala J, Kaarniranta K, Haapasalo A, Hiltunen M, Soininen H (2011) Astrocytes in the aging brain express characteristics of senescence-associated secretory phenotype. Eur J NeuroSci 34(1):3–11
Campisi J (2013) Aging, cellular senescence, and cancer. Annu Rev Physiol 75(1):685–705
Chen NC, Partridge AT, Tuzer F, Cohen J, Nacarelli T, Navas-Martín S, Sell C, Torres C, Martín-García J (2018) Induction of a senescence-like phenotype in cultured human fetal microglia during HIV-1 infection. The Journals of Gerontology: Series A 73(9):1187–1196
Nelson G, Wordsworth J, Wang C, Jurk D, Lawless C, Martin-Ruiz C, von Zglinicki T (2012) A senescent cell bystander effect: senescence-induced senescence. Aging Cell 11(2):345–349
Prattichizzo F, Bonafè M, Olivieri F, Franceschi C (2016) Senescence associated macrophages and “macroph-aging”: are they pieces of the same puzzle?. Aging 8(12):3159–3160
Franceschi C, Campisi J (2014) Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 69(Suppl 1):S4–S9
Franceschi C, Garagnani P, Parini P, Giuliani C, Santoro A (2018) Inflammaging: a new immune–metabolic viewpoint for age-related diseases. Nat Rev Endocrinol 14(10):576– 590
Franceschi C, Zaikin A, Gordleeva S, Ivanchenko M, Bonifazi F, Storci G, Bonafe M (2018) Inflammaging 2018: An update and a model. Semin Immunol 40:1–5
Franceschi C, Garagnani P, Vitale G, Capri M, Salvioli S (2017) Inflammaging and ‘garb-aging’. Trends in Endocrinology & Metabolism 28(3):199–212
Wekerle H (2018) Brain inflammatory cascade controlled by gut-derived molecules. Nature 557 (7707):642–643
Gompertz B (1825) XXIV. On the nature of the function expressive of the law of human mortality, and on a new mode of determining the value of life contingencies. In a letter to Francis Baily, Esq. F. R. S. &c. Philos Trans R Soc Lond 115:513–583
Brown KS, Math B, Forbes WF (1974) A mathematical model of aging processes. II. J Gerontol 29(4):401–409
Periwal A (2013) Cellular senescence in the Penna model of aging. Phys Rev E 88(5):052702
deMedeiros N GF, Onody RN (2001) Heumann-Hötzel model for aging revisited. Phys. Rev. E 64:041915
Taneja S, Mitnitski AB, Rockwood K, Rutenberg AD (2016) Dynamical network model for age-related health deficits and mortality. Phys Rev E 93(2):022309
Farrell SG, Mitnitski AB, Theou O, Rockwood K, Rutenberg AD (2018) Probing the network structure of health deficits in human aging. Phys. Rev. E 98:032302
Farrell SG, Mitnitski AB, Rockwood K, Rutenberg AD (2016) Network model of human aging: Frailty limits and information measures. Phys. Rev. E 94:052409
Weismann A (1889) The duration of life. In: Poulton EB, Schönland S, Shipley AE (eds) Essays upon heredity and kindred biological problems. Authorised translation, Clarendon Press, Oxford
Pearl R (1928) The rate of living: Being an account of some experimental studies on the biology of life duration. Knopf, New York
Sohal RS (1986) The rate of living theory: a contemporary interpretation. In: Collatz KG, Sohal RS (eds) Insect aging, Springer, pp 23–44
Medawar PB (1952) An unsolved problem of biology: an inaugural lecture delivered at university college, london, 6 december 1951. H.K. Lewis & Co. for U.C.L., London. Reprinted in [53]
Medawar PB (1957) An unsolved problem of biology. In: The uniqueness of the individual, pp 44–70. Basic Books, New York
Harman D (1998) Extending functional life span. Exp Gerontol 33(1-2):95–112
Emanuel NM (1976) Free radicals and the action of inhibitors of radical processes under pathological states and ageing in living organisms and in man. Q Rev Biophys 9(2):283–308
Nesse RM, Williams GC (1995) Evolution by natural selection. In: Evolution and Healing: New Science of Darwinian Medicine, pp 13–25. Weidenfeld & Nicolson, London
Clarke JM, Smith JM (1961) Two phases of ageing in drosophila subobscura. J Exp Biol 38 (3):679–684
Smith JM (1963) Temperature and the rate of ageing in poikilotherms. Nature 199(4891):400–402
Kirkwood T BL (1977) Evolution of ageing. Nature 270(5635):301–304
Gladyshev GP (1999) Thermodynamic theory of biological evolution and aging. Experimental confirmation of theory. Entropy 1(4):55–68
Olovnikov AM (2003) The redusome hypothesis of aging and the control of biological time during individual development. Biochemistry (Moscow) 68:2–33
Holbek S, Bendtsen KM, Juul J (2013) Moderate stem-cell telomere shortening rate postpones cancer onset in a stochastic model. Phys. Rev. E 88:042706
Mc Auley MT, Mooney KM (2015) Computationally modeling lipid metabolism and aging: A mini-review. Computational and Structural Biotechnology Journal 13:38–46
Mc Auley MT, Guimera AM, Hodgson D, Mcdonald N, Mooney KM, Morgan AE, Proctor CJ (2017) Modelling the molecular mechanisms of aging. Biosci Rep 37(1):BSR20160177
Vijg J, Suh Y (2013) Genome instability and aging. Annu Rev Physiol 75(1):645–668
Arino O, Kimmel M, Webb GF (1995) Mathematical modeling of the loss of telomere sequences. J Theor Biol 177(1):45–57
Olofsson P, Kimmel M (1999) Stochastic models of telomere shortening. Math Biosci 158 (1):75–92
Tan Z (1999) Telomere shortening and the population size-dependency of life span of human cell culture: further implication for two proliferation-restricting telomeres. Exp Gerontol 34(7):831–842
Labbadia J, Morimoto RI (2015) The biology of proteostasis in aging and disease. Ann Rev Biochem 84(1):435–464
Zou J, Guo Y, Guettouche T, Smith DF, Voellmy R (1998) Repression of heat shock transcription factor HSF1 activation by HSP90 (HSP90 complex) that forms a stress-sensitive complex with HSF1. Cell 94(4):471–480
Liepe J, Holzhütter H-G, Bellavista E, Kloetzel PM, Stumpf MichaelPH, Mishto M (2015) Quantitative time-resolved analysis reveals intricate, differential regulation of standard- and immuno-proteasomes. eLife 4:e07545
Proctor CJ, Tsirigotis M, Gray DA (2007) An in silico model of the ubiquitin-proteasome system that incorporates normal homeostasis and age-related decline. BMC Systems Biology 1(1):17
Tavassoly I, Parmar J, Shajahan-Haq AN, Clarke R, Baumann WT, Tyson JJ (2015) Dynamic modeling of the interaction between autophagy and apoptosis in mammalian cells. CPT: Pharmacometrics & Systems Pharmacology 4(4):263–272
Schulzer M, Lee CS, Mak EK, Vingerhoets F JG, Calne DB (1994) A mathematical model of pathogenesis in idiopathic parkinsonism. Brain 117(3):509–516
Raichur A, Vali S, Gorin F (2006) Dynamic modeling of alpha-synuclein aggregation for the sporadic and genetic forms of Parkinson’s disease. Neuroscience 142(3):859–870
Proctor CJ, Tangeman PJ, Ardley HC (2010) Modelling the role of UCH-L1 on protein aggregation in age-related neurodegeneration. PLoS ONE 5(10):e13175
Cloutier M, Wellstead P (2012) Dynamic modelling of protein and oxidative metabolisms simulates the pathogenesis of Parkinson’s disease. IET Systems Biology 6(3):65
Proctor CJ, Pienaar I, Elson JL, Kirkwood ThomasBL (2012) Aggregation, impaired degradation and immunization targeting of amyloid-beta dimers in Alzheimer’s disease: a stochastic modelling approach. Mol Neurodegener 7(1):32
Harman D (1972) The biologic clock: The mitochondria?. J Am Geriatr Soc 20(4):145–147
Kowald A, Kirkwood T BL (2011) Evolution of the mitochondrial fusion-fission cycle and its role in aging. Proceedings of the National Academy of Sciences 108(25):10237– 10242
Pezze PD, Sonntag AG, Thien A, Prentzell MT, Godel M, Fischer S, Neumann-Haefelin E, Huber TB, Baumeister R, Shanley DP, Thedieck K (2012) A dynamic network model of mTOR signaling reveals TSC-independent mTORC2 regulation. Sci Signal 5(217):ra25–ra25
Sonntag AG, Pezze PD, Shanley DP, Thedieck K (2012) A modelling-experimental approach reveals insulin receptor substrate (IRS)-dependent regulation of adenosine monosphosphate-dependent kinase (AMPK) by insulin. FEBS Journal 279(18):3314–3328
Pezze PD, Nelson G, Otten EG, Korolchuk VI, Kirkwood T BL, von Zglinicki T, Shanley DP (2014) Dynamic modelling of pathways to cellular senescence reveals strategies for targeted interventions. PLoS Computational Biology 10(8): e1003728
Oeckinghaus A, Ghosh S (2009) The NF-κ B family of transcription factors and its regulation. Cold Spring Harbor Perspectives in Biology 1 (4):a000034–a000034
Napetschnig J, Wu H (2013) Molecular basis of NF-κ B signaling. Annu Rev Biophys 42(1):443–468
Basak S, Behar M, Hoffmann A (2012) Lessons from mathematically modeling the NF-κ B pathway. Immunol Rev 246(1):221–238
Williams R, Timmis J, Qwarnstrom E (2014) Computational models of the NF-κ B signalling pathway. Computation 2(4):131–158
Scheff JD, Calvano SE, Lowry SF, Androulakis IP (2010) Modeling the influence of circadian rhythms on the acute inflammatory response. J Theor Biol 264(3):1068–1076
McGovern AP, Powell BE, Chevassut TJT (2012) A dynamic multi-compartmental model of DNA methylation with demonstrable predictive value in hematological malignancies. J Theor Biol 310:14–20
Przybilla J, Rohlf T, Loeffler M, Galle J (2014) Understanding epigenetic changes in aging stem cells — a computational model approach. Aging Cell 13(2):320–328
Smith-Vikos T, Slack FJ (2012) MicroRNAs and their roles in aging. J Cell Sci 125(1):7–17
Lai X, Wolkenhauer O, Vera J (2016) Understanding microRNA-mediated gene regulatory networks through mathematical modelling. Nucleic Acids Res 44(13):6019–6035
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G (2013) The hallmarks of aging. Cell 153(6):1194–1217
Pekovic V, Hutchison CJ (2008) Adult stem cell maintenance and tissue regeneration in the ageing context: the role for A-type lamins as intrinsic modulators of ageing in adult stem cells and their niches. J Anat 213(1):5–25
Duscher D, Rennert RC, Januszyk M, Anghel E, Maan ZN, Whittam AJ, Perez MG, Kosaraju R, Hu MS, Walmsley GG, Atashroo D, Khong S, Butte AJ, Gurtner GC (2014) Aging disrupts cell subpopulation dynamics and diminishes the function of mesenchymal stem cells. Scientific Reports 4 (1):7144
Kyrtsos CR, Baras JS (2015) Modeling the role of the glymphatic pathway and cerebral blood vessel properties in Alzheimer’s disease pathogenesis. PLOS ONE 10(10):e0139574
Leloup J-C, Goldbeter A (2008) Modeling the circadian clock: From molecular mechanism to physiological disorders. BioEssays 30(6):590–600
Altinok A, Lévi F, Goldbeter A (2007) A cell cycle automaton model for probing circadian patterns of anticancer drug delivery. Adv Drug Deliv Rev 59(9-10):1036–1053
Irwin MR (2019) Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol 19(11):702–715
Besedovsky L, Lange T, Haack M (2019) The sleep-immune crosstalk in health and disease. Physiol Rev 99(3):1325–1380
Albrecht U, Ripperger JA (2018) Circadian clocks and sleep: Impact of rhythmic metabolism and waste clearance on the brain. Trends Neurosci 41(10):677–688
Rasmussen MK, Mestre H, Nedergaard M (2018) The glymphatic pathway in neurological disorders. The Lancet Neurology 17(11):1016–1024
Obata Y, Castaño A, Boeing S, Bon-Frauches AC, Fung C, Fallesen T, de Agüero MG, Yilmaz B, Lopes R, Huseynova A, Horswell S, Maradana MR, Boesmans W, Berghe PV, Murray AJ, Stockinger B, Macpherson AJ, Pachnis V (2020) Neuronal programming by microbiota regulates intestinal physiology. Nature 578(7794):284–289
Franceschi C, Ostan R, Santoro A (2018) Nutrition and inflammation: Are centenarians similar to individuals on calorie-restricted diets?. Annu Rev Nutr 38(1):329–356
Stenholm S, Head J, Kivimäki M, Hanson L LM, Pentti J, Rod NH, Clark AJ, Oksanen T, Westerlund H, Vahtera J (2018) Sleep duration and sleep disturbances as predictors of healthy and chronic disease–free life expectancy between ages 50 and 75: A pooled analysis of three cohorts. The Journals of Gerontology: Series A 74(2):204–210
Tobaldini E, Fiorelli EM, Solbiati M, Costantino G, Nobili L, Montano N (2018) Short sleep duration and cardiometabolic risk: from pathophysiology to clinical evidence. Nat Rev Cardiol 16 (4):213–224
Gerdes E OW, Zhu Y, Tchkonia T, Kirkland JL (2020) Discovery, development, and future application of senolytics: theories and predictions. The FEBS Journal 287(12):2418–2427
Khosla S, Farr JN, Tchkonia T, Kirkland JL (2020) The role of cellular senescence in ageing and endocrine disease. Nat Rev Endocrinol 16(5):263–275
Musi N, Valentine JM, Sickora KR, Baeuerle E, Thompson CS, Shen Q, Orr ME (2018) Tau protein aggregation is associated with cellular senescence in the brain. Aging Cell 17(6):e12840
Zhang P, Kishimoto Y, Grammatikakis I, Gottimukkala K, Cutler RG, Zhang S, Abdelmohsen K, Bohr VA, Sen JM, Gorospe M, Mattson MP (2019) Senolytic therapy alleviates aβ-associated oligodendrocyte progenitor cell senescence and cognitive deficits in an alzheimer’s disease model. Nat Neurosci 22(5):719–728
Chinta SJ, Woods G, Demaria M, Rane A, Zou Y, McQuade A, Rajagopalan S, Limbad C, Madden DT, Campisi J, Andersen JK (2018) Cellular senescence is induced by the environmental neurotoxin paraquat and contributes to neuropathology linked to parkinson’s disease. Cell Reports 22(4):930–940
Bussian TJ, Aziz A, Meyer CF, Swenson BL, van Deursen JM, Baker DJ (2018) Clearance of senescent glial cells prevents tau-dependent pathology and cognitive decline. Nature 562(7728):578–582
Hickson LJ, Prata L GPL, Bobart SA, Evans TK, Giorgadze N, Hashmi SK, Herrmann SM, Jensen MD, Jia Q, Jordan KL, Kellogg TA, Khosla S, Koerber DM, Lagnado AB, Lawson DK, LeBrasseur NK, Lerman LO, McDonald KM, McKenzie TJ, Passos JF, Pignolo RJ, Pirtskhalava T, Saadiq IM, Schaefer KK, Textor SC, Victorelli SG, Volkman TL, Xue A, Wentworth MA, Gerdes E OW, Zhu Y, Tchkonia T, Kirkland JL (2019) Senolytics decrease senescent cells in humans: Preliminary report from a clinical trial of dasatinib plus quercetin in individuals with diabetic kidney disease. EBioMedicine 47:446–456
Benveniste H, Liu X, Koundal S, Sanggaard S, Lee H, Wardlaw J (2018) The glymphatic system and waste clearance with brain aging: A review. Gerontology 65(2):106–119
Xu M, Bradley EW, Weivoda MM, Hwang SM, Pirtskhalava T, Decklever T, Curran GL, Ogrodnik M, Jurk D, Johnson KO, Lowe V, Tchkonia T, Westendorf JJ, Kirkland JL (2017) Transplanted Senescent Cells Induce an Osteoarthritis-Like Condition in Mice. The Journals of Gerontology: Series A 72(6):780–785
Hall BM, Balan V, Gleiberman AS, Strom E, Krasnov P, Virtuoso LP, Rydkina E, Vujcic S, Balan K, Gitlin I, Leonova K, Polinsky A, Chernova OB, Gudkov AV (2016) Aging of mice is associated with p16(Ink4a)- and β-galactosidase-positive macrophage accumulation that can be induced in young mice by senescent cells. Aging 8(7):1294–1315
Wong WT (2013) Microglial aging in the healthy CNS: phenotypes, drivers, and rejuvenation. Front Cell Neurosci 7:22
Funding
We acknowledge support by the grant of the Ministry of Education and Science of the Russian Federation Agreement No. 074-02-2018-330(1). AZ received MRC grant MR/R02524X/1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is a contribution to the special issue on Immunosenescence: New Biomedical Perspectives - Guest Editors: Claudio Franceschi, Aurelia Santoro, and Miriam Capri
Appendices
Appendix 1: Model detalization
The changes in the concentration of garbage in a certain volume of brain are determined by the balance of its accumulation during neuronal activity on the one hand, and its degradation and clearance by microglial cells and astrocytes on the other. In space-time studies, we neglect the garbage diffusion, assuming it to be much slower than that of SASP molecules (see Eq. 6 below). The dynamics of garbage concentration is then described by the following equation:
where Q(t) denotes the (time-dependent) garbage production rate, γ1 is the rate of spontaneous degradation of garbage, and the two remaining terms describe two mechanisms of active garbage elimination: uptake by astrocytes and microglia (term with γ2) and the effect of glymphatic system (term with γ3).
The rate of garbage uptake by the glial cells depends on the state thereof, which can be active leading to fast cleaning, and normal quiet state associated with slow cleaning. The activation of the healthy glial cells is assumed to be determined by garbage concentration and is described by the function h(R), which we assume to be a sigmoid function of the following form:
where x0 denotes the rate of waste clearance by non-activated microglia, R1 is the activation midpoint, and η1 is the inverse slope of the activation curve (see Fig. 4a).
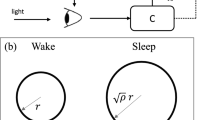
Model functions: a describes activation h(R) of healthy glial cells clearing garbage as a function of the garbage concentration R, whereas the function hR(R) describes an increment of senescent cell proportion, when glial cells are overactivated as a result of garbage accumulation; b illustrates the function hS(S) describing a transition between healthy and senescent cells in the course of interaction with SASP molecules
The glymphatic system is astrocyte-dependent and is activated during sleep. This daily variability is accounted for by the function T(t).
The saturation of both garbage elimination systems is described by normalized nonlinear functions f2,3(R). Given no specific experimental data on either of them, we use a single function obtained from a kinetic description of garbage binding to glia:
where R0 is the saturation curve midpoint (which is the level of garbage concentration, where the elimination rate is half the maximum).
The conversion of glial cells to the senescent state is assumed to be induced by glial overactivation promoted by garbage accumulation, and also by SASP molecules, which are in turn constantly produced by the senescent cells. The progression of glial senescence is described by the following dynamical equation for the fraction of the senescent glia GS (total quantity of glia assumed constant):
where γB is the background (always present) senescence rate, γR and γS control the rates of senescence induced by garbage and SASP, hR(R) and hS(S) are corresponding normalized activation functions, which are assumed to be sigmoid functions:
where RA and SA are senescence activation midpoints for garbage and SASP, ηR and ηS determine the widths of the smoothed step transition (see Fig. 4).
The changes of SASP molecule concentration \(\tilde {S}\) are determined by the balance of their production (by senescent astrocytes and microglia), natural degradation, and diffusion, and are described by the equation:
where σG is the rate of SASP production by senescent cells, σS is SASP degradation rate, D is the diffusion coefficient, and Δ is the Laplacian operator.
Appendix 2: Model reductions
Here, we derive and analyze the reduced formulations of the model, as described in the “Reduced formulations of the mode”. All notations are additionally summarized in Table 2.
2.1 Dynamics of garbage concentration
Assuming the rate of spontaneous garbage degradation to be much smaller than that of active garbage cleaning by glial cells, we neglect the term with γ1 in Eq. 1, transforming the latter into:
The factor in square brackets here describes the dependence of garbage elimination rate on time t and concentration of garbage R. Generally speaking, it cannot be factorized into a product of separate functions of t and R. That said, and taking into account the absence of experimental data to quantify all the unknown functions within the bracketed expression, for the sake of model simplicity, we artificially impose the assumption of such factorization, which reduces the equation to the form:
where C(t) characterizes the time dependence of garbage elimination, and f(R) the concentration dependence. For the sake of analytical consideration, we use a simplified piecewise linear saturation function:
and in numerical simulations also the smooth function f(R) = fK(R) as defined in Eq. 3.
Following this approach, we essentially abstract from quantifying the effect of glial cell activation (given by the function h(R) in the full model Eq. 1). If taken into account, glial activation would show up as a section with steeper dependence of garbage elimination rate upon garbage concentration somewhere below the saturation level (at \(R\lesssim R_{0}\)). We argue that this would only have a quantitative impact, while our main qualitative results remain mainly determined by saturation effects, which we necessarily take into account. Therefore, we limit ourselves to a paradigmatic model in the form Eq. 8, considering further detalization currently unattainable due to the aforementioned lack of experimental data.
Hereafter, we assume that R is measured in the units of R0, which implies R0 = 1.
For further simplification, we recall that the fraction of the senescent glia is typically a small value. A quantitative reference for the number or frequency of senescent microglia/macrophages in the aged brain is currently lacking, due in part to the complexity of defining specific criteria for glial senescence in vivo. In a recent study, the percentage of senescent microglia ranged from 1 to 4% of the total population [30]. This is consistent with senescent cell numbers in other tissues and reflects a significant number of dysfunctional senescent cells. Indeed, very small numbers of transplanted senescent cells are enough to cause lasting physical dysfunction [115, 116]. Hence, we assume G = 1 without significant impairment of model precision.
To account for daily variability of garbage production and elimination rates, we assume that Q(t) and C(t) take on different constant values during wakefulness and sleep, these values further respectively denoted as Qw, Cw, and Qs, Cs.
Finally, the simplified version of Eq. 8 which we will analyze reads:
where the upper and the lower symbols correspond to wakefulness and sleep.
As soon as the piecewise linear saturation function fP(R) Eq. 9 is used, Eq. 10 implies accumulation or decay of garbage at a constant rate above the saturation threshold in R:
and reduces to a linear equation below the saturation threshold:
Natural assumptions are:
otherwise, according to Eq. 12, a stationary concentration of garbage \(R_{\infty }=Q_{w}/C_{w}<1\) would be attained even without sleep, thus rendering sleep unnecessary, and
otherwise elimination of garbage during sleep would be impossible.
We measure time in days and denote the duration of sleep as Ts, and that of wakefulness as Tw = 1 − Ts. We note that whenever
Eq. 11 leads to infinite accumulation of garbage; thus, there exists a critical sleep duration \(T_{s}^{\text {crit}}\) determined by
If \(T_{s}>T_{s}^{\text {crit}}\) (sufficient sleep), garbage concentration during sleep falls below the saturation level (R < 1), and during wakefulness may or may not exceed the saturation level. Established dynamics of garbage concentration in this regime is shown in Fig. 5a. Here, we use the values of parameters Qw = 5, Cw = 3, Qs = 0, Cs = 6, which are justified below, along with Ts = 1/3, which corresponds to a sleep duration of 8 h.
Dynamics of the garbage concentration R(t) in the simplified piecewise linear model with Qw = 5, Cw = 3, Qs = 0, Cs = 6: a normal sleep (8 h, Ts = 1/3); b critical regime of sleeping (6 h, Ts = 1/4), maximal value Eq. 17 shown with a red dashed horizontal line; c insufficient sleep (5 h, Ts = 5/24), average trend Eq. 18 shown with a red dashed line
At the critical sleep duration \(T_{s}=T_{s}^{\text {crit}}\), garbage concentration R(t) in the stationary regime demonstrates a saw-like profile with minimum at the saturation threshold R = 1 and with maximum
Established dynamics of garbage concentration in the critical regime is shown in Fig. 5b with the value \(R=R_{\max \limits }^{\text {crit}}\) marked with a red dashed horizontal line. Here, sleep duration is Ts = 1/4 (equivalent to 6 h), other parameters same as above.
If \(T_{s}<T_{s}^{\text {crit}}\) (insufficient sleep), then garbage concentration inevitably rises above the saturation level (R > 1) and accumulates infinitely (while the deficiency of sleep is present) with average rate:
Dynamics of garbage accumulation in this regime is shown in Fig. 5c with the average trend \(R(t) \sim \langle \dot R \rangle \cdot t\) shown with a red dashed line. Here, sleep duration is Ts = 5/24 (5 h).
In order to fit the model parameters to reality, we start with the assumption that garbage production during sleep is negligible compared with that during wakefulness (Qs ≪ Qw), so further we let Qs = 0 for simplicity. The remaining model parameters Qw, Cw, Cs can be quantified using the following considerations for a healthy human.
During sleep, the dynamics of garbage in the unsaturated regime (when R < 1) is described by the linear Eq. 12, which reduces to:
and implies exponential decay of garbage concentration to zero:
with characteristic time scale:
Then, sleep periods greatly exceeding τs (for definiteness, Ts > 2τs) are excessive in the sense that further sleeping does not improve garbage elimination significantly. Estimating this sufficient sleep duration as 8 h, we get τs equal to 4 h, or in the units of days τs ≈ 1/6, which produces an estimate Cs ≈ 6.
In order to estimate the two remaining parameters Qw and Cw, we generally need two additional biologically relevant quantitative model outcomes to correlate with reality. For one of them, we use the critical sleep duration \(T_{s}^{\text {crit}}\), for which from Eq. 16 we get:
Estimating \(T_{s}^{\text {crit}}\approx 0.25\) (6 h), and using the above estimate Cs ≈ 6, we get Qw − Cw ≈ 2. Due to scarcity of quantitative experimental data on the dynamics of garbage concentration in the brain, we further employ the observation of [5, 114] that the rate of garbage elimination during sleep is roughly twice than that during wakefulness, which finally yields Cw ≈ Cs/2 ≈ 3, Qw ≈ Cw + 2 ≈ 5. This set of parameters was used to produce the profiles of R(t) in Fig. 5 and is used hereinafter, unless stated otherwise.
When the piecewise linear saturation function Eq. 9 in the model is replaced by a more realistic smooth function Eq. 3, with parameter values unchanged, the quantitative dynamics R(t) changes, but the qualitative behavior remains. This can be seen in Fig. 6, where panel (a) corresponds to normal sleep duration (8 h) and panel (b) shows the accumulation of garbage in case of sleep deficiency (5 h of sleep). Remarkably, the expression for average trend Eq. 18 still produces a good estimate for garbage accumulation rate in the saturation regime (shown with the red dashed line in the figure).
2.2 Dynamics of glial senescence
The sigmoid activation functions hR(R) and hS(S) Eq. 5 from dynamical equation for the fraction of senescent glia Eq. 4 for the sake of analysis can be written in the step form:
where H(⋅) is the Heaviside step function.
The balance equation for the unnormalized SASP concentration Eq. 6 allows for arbitrary rescaling of its variable of state, which allows eliminating one of its parameters. We make such rescaling by introducing a normalized SASP concentration variable S according to:
so that the unitary concentration S = 1 is now defined as the (actually unattainable) stationary concentration of SASP, which would be achieved if all the glia were senescent (GS = 1). In this notation, the balance Eq. 6 transforms into
where the parameter σS determines the characteristic time scale τS of SASP concentration equilibration
2.3 Local dynamics of garbage and senescence
To characterize the joint dynamics of glial senescence and SASP, we first consider their local dynamics, which implies DΔS = 0 in Eq. 25. This corresponds to the absence of diffusion D = 0, or to the spatially uniform case with ΔS = 0.
Assuming the time scale τS of SASP dynamics to be much smaller (faster) than that of glial senescence, we can replace S in Eq. 4 by its quasi-steady-state approximation from Eq. 25, which is
Additionally, in order to focus on garbage-induced senescence, we neglect the background (garbage-independent) senescence by taking γB = 0. This way Eq. 4 is transformed into
Model Eq. 4 implies that the quantity of senescent glia never decreases. In the version Eq. 28 with step functions Eq. 23 taken for hR(⋅) and hS(⋅) senescence at best does not progress (GS = const) while R < RA and GS < SA, and increases otherwise.
In other words, while senescence remains below its threshold (GS < SA), the accumulation of senescent glial cells is conditioned by garbage and occurs only when the latter exceeds its respective threshold (R ≥ RA).
As soon as senescence due to its course-of-life accumulation exceeds its threshold (GS ≥ SA), the right-hand side of Eq. 28 becomes positive regardless of the garbage level, which implies the monotonous accumulation of glial senescence due to a positive feedback via SASP even in the absence of further induction by garbage.
In this view, R = RA is the “garbaging” threshold; its temporary overshoot by garbage concentration leads to an increase in the quantity of senescent glia, which however stabilizes (does not accumulate any more) once the garbage overshoot ends. The garbage increase, in turn, may be caused by a temporary deficiency or deprivation of sleep, as it follows from the garbage balance Eq. 8, according to the results of the Section 2.1. The height and the duration of a garbage concentration peak induced by a particular episode of sleep restriction depend increasingly upon the severity and the duration of sleep deficiency.
We illustrate this by simulating the joint dynamics of garbage concentration and glial senescence according to the Eq. 8 and Eq. 28 with smooth nonlinearities Eq. 3, Eq. 5. Parameters of garbage dynamics Eq. 8 are as in Section 2.1, and for senescence dynamics Eq. 28, due to the lack of real data, we pick indicative quantities γR = γS = 10− 4, along with activation function parameters in Eq. 5RA = 15, ηR = 1, SA = 0.1, ηS = 0.005. In Fig. 7a, we show the simulation result on a time interval of 350 days. Most of the time, the sleep duration is 8 h (Ts = 1/3), except for two episodes of sleep restriction (Ts = 5/24 or 5 h) lasting for 10 and 20 days, which correspond to the first two peaks in the garbage dynamics (the upper panel in Fig. 7a), and two episodes of complete sleep deprivation (Ts = 0) lasting for 3 and 7 days, which correspond to the latter two peaks in the garbage dynamics. Indeed, we observe more pronounced garbage peaks as the duration of sleep deprivation or restriction is increased (the 2nd and the 4th peaks, compared with the 1st and the 3rd). Expectedly, complete sleep deprivation (the 3rd and the 4th peaks) produces a steeper increase of garbage than sleep deficiency (the 1st and the 2nd peaks). We have chosen the garbaging threshold value RA = 15 so that only the more severe episodes of sleep restriction (20 days of sleep deficiency or 7 days of complete sleep deprivation) lead to the accumulation of glial senescence (the lower panel in Fig. 7a).
Simultaneous dynamics of the garbage concentration R(t) and the fraction of senescent cells GS(t) in a variable sleep quality profile containing 2 periods of sleep deficiency and 2 periods of total sleep deprivation interleaved with normal sleep (see details in the text): a garbage removal rates are at their normal values Cs = 6, Cw = 3, as estimated in Section B.1 ; b age-impeded garbage removal with Cs = 5.7, Cw = 2.85 (95% of the norm) leads to higher garbage peaks and greater accumulation of senescence; c same age-impeded garbage removal on top of pre-existing age-related glial senescence GS(t = 0) = 0.085 triggers the vicious circle of self-sustained SASP-mediated senescence; the hypothetic recovery of senescent glia breaks the vicious circle, as shown in panel (c) by resetting GS at t = 500 back to GS(t = 500) = 0.085
To demonstrate the effect of an age-related decrease of garbage elimination rate upon the dynamics of garbage and glial senescence, we performed a similar simulation with garbage elimination rates Cs = 5.7, Cw = 2.85, which are cut down by 5% compared with the previous simulation, all other conditions unchanged. The result is shown in Fig. 7b, showing higher garbage peaks and longer recovery times; moreover, all four episodes of sleep deficiency now produce glial senescence. The resultant increment of glial senescence over the same simulated time interval is now about 3 times greater than in the previous simulation (cf. Fig. 7a).
In turn, GS = SA is the “inflammaging” threshold. When senescent glia accumulates beyond this threshold (due to accumulation of the above mentioned “garbaging” overshoots during the life course), further progression of senescence becomes monotonous due to self-induction via SASP and does not stop until the end of life. This is illustrated by the simulation result shown in Fig. 7c, where all conditions are the same as in Fig. 7b, except for starting from a higher value of the senescence variable GS(t = 0) = 0.085 and extending the simulated time interval (the relevant part is up to t = 500 days; the remaining part of the graph is discussed below). Here, the senescence variable, once reaching the inflammaging threshold SA = 0.1, continues to grow even in the absence of garbaging peaks.
This feature of our model implies that inflammaging, once set in, never stops, even if the garbage elimination rate recovers to normal. More precisely, our model does not incorporate any mechanisms for inflammaging to stop. This follows from the assumptions that inflammaging is driven by SASP, which in turn is produced by senescent cells, which remain in this state perpetually.
A hypothetic possibility to extinguish inflammaging would require a mechanism to eliminate senescent cells from the brain faster than they build up. Wong [117] and Clarke with colleagues [22] discuss the replacement of aged microglia with young microglia as the “rejuvenative” therapy. These microglial “replacements” may promote the removal of accumulated garbage, and the slowdown of the cellular senescence process, thereby improving cognitive function in aging. Prospects for the role of techniques for clearance of senescent macrophages in prolonging healthspan are actively discussed in the scientific community now [36]. We simulate such recovery of senescent glia by artificially resetting the variable GS to a sub-inflammaging value GS = 0.085, as shown in Fig. 7c at t = 500. The concentration of senescent cells is now reset, self-induction and progression of senescence are stopped, and future behavior will again depend on whether sleep pattern and garbage elimination are normal or not.
2.4 Space-time dynamics of senescence (“propagaging”)
The model in the form of ordinary differential equations considered in Section 2.3, where diffusion is dropped and quasi-steady-state approximation is used to express SASP concentration, applies to the description of the dynamics of glial senescence in the brain taken as a whole, on large time scales up to the lifetime, or in local parts of the brain, while this local senescence does not propagate in space.
In order to describe the progression of senescence with spatial detalization, we revert to the full model consisting of the equations for glial senescence Eq. 4 and SASP balance Eq. 25 including the diffusion term. We focus on propagating solutions where glial senescence propagates itself through the tissue in the wake of diffusing SASP (a phenomenon referred to as propagation of inflammaging [40]). In this regard, we take an initial spatial profile of senescence at the onset of propagation as given, abstracting from its backstory and taking into account the only mechanism of senescence, namely that activated by SASP (γS≠ 0), while assuming γB = 0, γR = 0 in Eq. 4. Although we recognize activation by garbage as the root cause initiating senescence, we consider it as part of the mentioned “backstory,” which is adequately described by local dynamics as in Section 2.3, and hence we omit it in the model of inflammaging propagation.
Finally, we formulate the mathematical model as a system of simultaneous Eqs. 4 and 25 with the assumptions above taken into account:
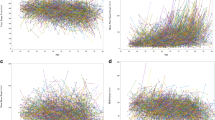
We simulate a two-dimensional system with spatial inhomogeneity introduced into the initial profile of the senescence variable GS, as shown in panel (a) of Fig. 8. To initiate inflammaging propagation, we place a patch with a sufficiently high senescence value in the center of the system. A typical snapshot of the senescence variable in color encoding taken at t = 25 is presented in panel (b) of Fig. 8.
We find that the spatial inhomogeneity of the initial senescence background may lead to faster propagation of the senescence front than it would be in case of homogeneous initial senescence with the same average. To quantify this statement, we calculate the ratio 𝜖 of the tissue volume with high level of senescence (where the condition GS > SA is fulfilled) to the total volume of the tissue. We compute 𝜖 over time in settings with homogeneous and inhomogeneous initial senescence backgrounds with the same average. The resulting plots are shown in Fig. 9 confirming faster propagation of senescence in the inhomogeneous case.
This phenomenon can be explained by quicker propagation of the front in areas with greater initial senescence, which allows the inflammaging to cover quickly larger distance, even though leaving behind some non-inflamed “holes” in places where initial senescence was low. These holes eventually get taken over by the inflammaging propagation process without hindering the fast propagation of the foremost parts of the front.
Rights and permissions
About this article
Cite this article
Gordleeva, S., Kanakov, O., Ivanchenko, M. et al. Brain aging and garbage cleaning. Semin Immunopathol 42, 647–665 (2020). https://doi.org/10.1007/s00281-020-00816-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00281-020-00816-x