Abstract
Summary
Nationwide hip fracture incidence in the Austrian population was assessed over a period of 30 years (1989–2018), including 20 years data from a previous study and a recent 10 years follow-up. While absolute numbers in men continued to increase, absolute numbers in women and age-standardized incidences in both men and women decreased.
Purpose
In the Austrian population ≥ 50 years, nationwide hip fracture incidences over a period of 20 years (1989–2008) have shown an initial steep increase, followed by a leveling-off during the last few years of observation. The purpose of the present study was to follow up on hip fracture incidences for another 10 years (2009–2018) and to analyze trends over the entire period of 30 years.
Methods
ICD-10 code classes S72.0, S72.1, and S72.2 were applied. All data were retrieved from the Statistics Austria database and its hospital discharge register. Annual absolute numbers, crude and age-standardized incidences, and incidence rate ratios (IRR) were stratified by sex and 5-year age intervals, and calculated by using a correction factor for multiple registrations.
Results
Total number of hip fracture cases increased from 13,984 (2009) to 14,640 (2015), and decreased thereafter to 14,457 (2018), despite a persistent increase in men. Age-standardized incidences peaked at 476/100,000 (2010), followed by a decrease to 408/100,000 (2018). The observed overall decrease was mainly driven by the female population. Incidence rate ratios (IRRs) yielded a statistically significant average annual decrease of age-standardized incidences in both women and men (∆IRR 0.984; 0.981–0.987).
Conclusion
While absolute numbers of hip fracture in women showed a slight decrease during the last 10 years of observation, numbers in men continued to increase. Age-standardized incidences nevertheless decreased in both men and women, which may be interpreted as a trend in the right direction. However, due to the rapid aging of the population, it cannot be precluded that this trend will be compromised during the next few decades.
Similar content being viewed by others
Introduction
Osteoporosis is defined as a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture [1]. Among osteoporotic fractures, hip fracture has been recognized as the most serious one because of its consequences in regard to premature death, disability, chronic pain, and diminished quality of life [2].
Austria, located in the southern part of Central Europe, counted some 8.9 million inhabitants in 2019 [3]. Similar to other countries in the European Union, the present-day age pyramid shows a narrow base due to a reduction in birth rates and an increasing percentage of the population 50 years of age and older.
With an age-standardized incidence of 501/100,000 in women, and 264/100,000 in men, Austria is among the countries with the highest hip fracture incidences (and consequently hip fracture risk) worldwide, exceeded only by Sweden and Denmark [4].
In 2011, Austrian hip fracture incidences were reported in women and men aged 50 years and above, over a period of 20 years (1989–2008) [5]. Overall, it was found that the initial rise in age-standardized incidence between 1989 and 2005 was followed by a leveling off until the end of this 20-year period. This trend, however, was driven by a leveling off and subsequent decrease in fracture incidence in women, whereas the incidence in men has continued to rise to the end of the observation period. Interestingly, similar trend breaks have been reported before and thereafter for several other countries, particularly for those of the so-called Western world [6].
The purpose of the present study was to follow up on the incidence of hip fractures in the Austrian population aged 50 years and above for another 10 years (2009–2018), in order to analyze trends over the entire period of 30 years, and to assess whether the leveling off observed during the last few years of the 20 years report continued or changed into a decline or an increase.
Methods
Like in our previous study, hip fracture events were obtained from the Austrian Hospital Discharge Register (AHDR) for the entire Austrian population ≥ 50 years of age [5]. For the present study, hip fractures that occurred between 2009 and 2018, i.e., during a period of 10 years, were included in the analyses. According to the International Classification of Diseases (ICD) in its most recent version (version 10), the code classes S72.0, S72.1, and S72.2 were applied for identification of hip fractures. Data were extracted in 5-year intervals (50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, 85–90, 90–94, and 95 +) and stratified by sex and province (Upper Austria, Lower Austria, Styria, Carinthia, Salzburg, Tyrol, Vorarlberg, Burgenland, and Vienna). It should be noted that ICD coding changed from ICD-9 to ICD-10 in 2000. This change has been described in more detail in the previous study [5].
Data on the average annual resident population ≥ 50 years in all Austrian provinces and in 5-year age intervals was retrieved from the database of Statistics Austria. Annual crude incidence rates were calculated by relating yearly hip fracture cases corrected for multiple registrations to 100,000 persons in the population ≥ 50 years, stratified by sex, and 5-year age intervals. Age-standardized incidences were obtained by relating corrected hip fracture cases to the average Austrian population in each 5-year age interval both during 2009–2018 and during 1989–2018 for comparability with previous results on 1989–2008 [5].
In order to take into account multiple registrations for the same diagnosis within 1 year, the number of aggregate discharge diagnoses was corrected in two different ways. In one analysis, a correction factor of 0.9 was applied throughout to facilitate comparability with our previous study results 1989–2008, based on the same factor drawing on results from Germany and data from two Austrian hospitals [5, 7]. In addition, we assessed age group– and sex-specific correction factors for the period 2009–2018. For this purpose, non-aggregate data from the Austrian social insurance authorities with anonymized documentation of hip fracture discharge diagnoses according to ICD-10 S.72 without sub-codes were available for 2014–2016 from approximately 98% of the Austrian population ≥ 50 years. In this dataset of 49,397 discharge entries, re-admissions were defined as occurring within 6 months after the preceding discharge. (Re-)admission dates were calculated from hospital days associated with each discharge entry. Correction factors were assessed for age groups 50–69, 70–79, 80–89, and 90 + years, according to age at discharge or at first discharge in case of re-admissions, and in both sexes. Since sub-codes of S72 were not available from data of the Austrian social insurance authorities, a regional database of hip fracture discharges in Vorarlberg, the westernmost Austrian province, was utilized. This database contains anonymized entries, on personal level though, on 4386 hospital discharges due to ICD-10 S72 from 2003 to 2013, including sub-codes of S72. From this information, the proportion of re-admissions was ascertained in women and men both for all S72 diagnoses and for S72.0, S72.1, and S72.2 diagnoses only, with re-admissions defined as occurring within 6 months after a preceding discharge. The nationwide correction factor based on all S72 diagnoses was hence adapted accordingly.
The average annual change of hip fracture incidence during 2009–2018 was evaluated using Poisson and negative binomial regression models that were fit to corrected annual hip fracture counts with population size as offset variable. Covariates were age (in intervals of 5 years), sex, province, and year in the entire dataset. In further analyses stratified by sex and by age in 5-year intervals, the appropriate covariates were controlled for. Defining the variable “year” as continuous covariate yielded incidence rate ratios (IRRs) for average annual change for the 10-year observation period. Goodness of model fit was assessed using the ratios of both deviance and Pearson’s χ2 to the degrees of freedom (df) as measures of deviation from equidispersion, i.e., the departure from equality of variance and mean in the distribution of hip fracture occurrences, as well as the Akaike and Bayesian Information Criteria (AIC and BIC, respectively). For each evaluation, the one model was chosen with deviance/df and χ2/df ratios closest to 1 and the minimum AIC and BIC values. Applying a 0.05 significance level, IRRs were considered statistically significant when the ratio of 1 was outside the 95% confidence interval. All analyses were conducted in IBM SPSS Statistics, version 25 (IBM Corp., Armonk, NY).
Results
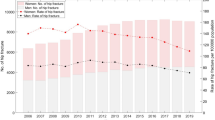
During the period of 2009–2018, the total number of hip fracture cases amounted to 14,640 in 2015, using a correction factor of 0.9 (Table 1). Incidence rates reached their maximum in 2010 in both sexes and decreased thereafter. Crude female and male incidences in 2010 amounted to 638 and 288, respectively, and decreased to 526 and 268 in 2018, respectively. When age-standardized for the average Austrian population 2009–2018, female and male incidences corrected by a factor of 0.9 were 629 and 296, respectively, in 2010, decreasing to 534 and 260, respectively, in 2018 (Table 1).
In addition, age group- and sex-specific correction factors were calculated and applied to assess hip fracture cases. Based on data of the Austrian social insurance authorities for all S72 diagnoses, these correction factors were 0.86, 0.82, 0.83, and 0.87 for women, and 0.89, 0.84, 0.84, and 0.86 for men aged 50–69, 70–79, 80–89, and 90 + years, respectively. Further sex-specific adjustment for the sub-codes S72.0, S72.1, and S72.2 based on the regional database in Vorarlberg resulted in only slight changes, yielding final correction factors of 0.87, 0.84, 0.84, and 0.88 for women, and 0.89, 0.85, 0.84, and 0.86 for men, 50–69, 70–79, 80–89, and 90 + years of age, respectively, that were applied to aggregate discharge data 2009–2018. Upon correction with these age- and sex-specific factors, the total number of hip fracture cases amounted to 13,879 in 2015 (Supplementary Table), and crude female and male hip fracture incidences in 2010 amounted to 602 and 275, respectively, declining to 498 and 256 in 2018, respectively. Age-standardized incidences in women and men 2010 were 595 and 283, respectively, and declined to 505 and 247, respectively, in 2018 (Supplementary Table).
Analysis of incidence rate ratios (IRRs) during 2009–2018 yielded a statistically significant average annual decrease of age-standardized incidences in both women and men (Table 1, Supplementary Table). Notably, the extent of the decrease was almost identical using either method of correction for multiple registrations. For both sexes, an IRR of 0.984 (95% CI 0.981–0.987) was observed, corresponding to an average annual decrease in hip fracture incidence of 1.6% (1.3–1.9%) from 2009 to 2018. In women, the rate ratio of 0.979 (95%–CI 0.977–0.982) applying a correction factor of 0.9, and 0.980 (95% CI 0.977–0.982) using age- and sex-specific correction factors corresponded to an average decline in annual incidences of 2.1% and 2.0% (2.3–1.8%), respectively, and men’s IRR of 0.986 (95% CI 0.982–0.989) equaled an average annual decline of 1.4% (1.1%–1.8%). Accordingly, IRRs were < 1 in all 5-year age groups, and this reduction was significant in most age groups in both women and men (Table 1 and Supplementary Table). In detail, applying a correction factor of 0.9, the most salient annual changes were observed in men aged 50–54 (− 3.7%, 95% CI − 2.0– − 5.4%) and 55–59 years (− 2.8%, 95% CI − 1.3– − 4.2%), and in women aged 55–59 (− 2.0%, 95% CI − 0.5– − 3.4%), 60–64 (− 2.1%, 95% CI − 0.7– − 3.4%), 75–79 (− 2.9%, 95% CI − 2.4– − 3.5%), 80–84 (− 3.0%, 95–CI − 2.6– − 3.5%), and 85–89 years (− 2.1%, 95% CI − 1.7– − 2.5%). By contrast, no significant changes were seen in men aged 60–64, 70–74, 90–94, and 95 + years, and in women aged 50–54, 70–74, and 95 + years (Table 1). Using age- and sex-specific correction factors, the results were almost identical (Supplementary Table).
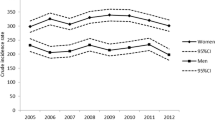
Results for the years 1989–2008 include data from [5] and are displayed in Fig. 1 (aggregate data) and Fig. 2 (age-standardized incidences).
Considering the entire period of 30 years (1989–2018), and applying a correction factor of 0.9, age-standardized hip fracture incidences peaked in 2003 at 689/100,000 women, and in 2006 at 294/100,000 men. A continuously decreasing incidence can be observed ever since for both sexes, falling to 517/100,000 and 242/100,000 in 2018 among women and men, respectively (Fig. 2).
Discussion
The findings of the present nationwide study indicate that in the Austrian female population aged 50 years and above, absolute numbers of hip fractures remained fairly stable until 2015, and thereafter slightly decreased until 2018. The plateau observed in the present study perpetuates the plateau observed during the last years of the previous study which had revealed a marked and sustained increase of hip fracture cases between 1989 and 2006. In contrast, absolute numbers in the male population continued their steady but small rise since 1989, even during the last 10 years of observation.
The true relevance of these findings becomes more evident considering that during the last 10 years of observation the number of women and men aged 50 years and above has markedly increased in Austria, similar to other countries of the so-called Western World. For example, the increase in the Austrian male population aged 50 years and above between 2009 and 2018 was 23%, and that in the female population of the same age amounted to 17%, corresponding to an overall average increase of 20% for the entire population aged 50 years and above.
Consequently, the age-standardized incidence in the Austrian female population has in fact significantly decreased between 2009 and 2018, indicating that the trend reversal observed during the years 2005 and 2006 sustained. Surprisingly and irrespective of the fact that absolute numbers continued to rise, age-standardized hip fracture incidence in men decreased during the past 10 years as well, albeit to a smaller extent compared to women. Similarly, results from a study in the westernmost Austrian province Vorarlberg during 2003–2013 had shown a declining age-standardized hip fracture incidence in women but no clear trend for men, whereas absolute numbers stagnated in women but were on the rise in men [8].
Leveling off or even decreases in (age-standardized) hip fracture incidences after initial (steep) increases have been observed for several populations, and even as early as during the second half of the past century [9]. For example, in the female population of Rochester (MN, USA), a steep increase in age-standardized hip fracture incidence was observed between 1930 and 1950, followed by a remarkable decrease until the turn of the century. A similar trend was noted in the male population, too, but the trend reversal occurred some 20 years later than in the female population [9]. In Europe, Finland was among the first countries which exhibited a break in the increasing trend of age-standardized hip fracture incidences [10]. A dramatic increase between 1970 and the mid-1990s was followed by a sustained decrease until 2016, in both women and men. Trend reversals in age-standardized incidence rates have also been reported for other European countries such as Switzerland, Norway, and the UK, but also for some countries in the Asian and Oceania region [9].
Aside from the increasingly constrictive shape of the Austrian population pyramid, several other factors may be considered causative for the decrease in age-standardized hip fracture incidence rates. For example, like in many other countries, an increase in the body mass index (BMI) has been observed in the Austrian population aged 55 years and above, beginning in the early 1980s of the past century [11]. Interestingly, this increase was more pronounced in the female population (+ 7.7%) than in the male population (+ 6.4%), whereby the change in women was mainly driven by those ≥ 75 years of age. Results of observational studies on a possible association between obesity and risk of hip fracture are conflicting. However, a recent meta-analysis of prospective cohort studies including more than three million participants provided strong evidence that obesity in adults is significantly and independently associated with a decreased risk of hip fracture [12]. Interestingly, there is also evidence that the effect of obesity on hip fracture risk may depend on the type of body fat distribution. In this regard, another recent meta-analysis found a strong association between abdominal (or visceral) obesity and an increase in hip fracture risk [13]. Given that abdominal obesity is mainly found in men, as opposed to women, in whom fat is mainly distributed around the hips and thighs, it may be speculated that the protective effect of an increasing BMI in men may at least in part be blunted by the type of body fat distribution itself.
Another possible reason for the marked decrease in hip fracture incidence observed in the female population could lie in the use of estrogen, combined or not combined with gestagens. After its initial use over more than two decades for prevention and treatment of menopause-related symptoms, menopausal hormone therapy (MHT) was approved by the Food and Drug Administration (FDA) for the prevention of osteoporosis in 1988 [14]. Although the effect of estrogen or MHT has not been investigated so far in a large-scale randomized controlled trial with a primary endpoint of fracture risk, a recent systematic review and meta-analysis showed an overall relative hip fracture risk reduction of 28% [15]. Consequently, women who had received their MHT as early as over the first decade after approval for osteoporosis prevention, and who have reached their eighth or ninth decade of life between 2006 and 2018, may have contributed significantly to the leveling off and subsequent decrease in hip fracture incidence during this period. Indeed, among all age groups, we observed the most pronounced reduction in annual incidences 2009–2018 in women aged 75–89 years (Table 1, Supplementary Table).
Improved nutrition and adipose gain during childhood and young adulthood may be another factor leading to a cohort effect characterized by reduced fracture risk in later life. In this regard, it was shown in a Finnish cohort of women born between 1934 and 1944 that hip fracture in later life was associated with increasing Z-scores for height at between 1 and 12 years of age, if this gain in height was not accompanied by an adequate increase in weight [16]. Consequently, the authors concluded that “thinness” in childhood could be a risk factor for hip fracture in later life.
Changes in smoking patterns in the older population could be another factor contributing to a decline in age-standardized hip fracture incidence. Largely independent of bone mineral density (BMD), smoking has been shown to be one of the strongest risk factors for hip fracture [17]. Consequently, it has been incorporated into different fracture risk calculation tools such as FRAX® and QFracture [18]. However, whereas due to stringent nationwide regulations smoking habits have led to a decrease in prevalence numbers in several countries in the past decade, two cross-sectional surveys (Austrian Health Interview Surveys for 2007 and 2014) revealed even increasing numbers in both men and women, including age groups 65 years and above [19]. It could thus be speculated that if Austrian health authorities had undertaken successful efforts to decrease smoking prevalence, hip fracture incidences may have dropped even more pronouncedly.
Functional ability as reflected by muscle strength, coordination, and balance has been shown to be associated with the risk of falls and consequently hip fracture [20, 21]. Whereas trend analyses on physical activities in the older population have been published for some countries, no such data is available for Austria [22]. However, in recent years, Austria has developed an ambitious framework addressing physical activity in all age groups, involving a network of over 15,000 sports clubs [23]. Thus, it cannot be precluded that the observed decrease in age-standardized hip fracture incidence has also been driven by an increase in physical activity particularly in the older population.
Finally, pharmacological interventions for prevention and treatment of osteoporosis, including increasing and widespread use of vitamin D together with calcium, may have contributed to the observed trend change in hip fracture incidence [24]. Although hip fracture per se has not been a primary endpoint in any of the pivotal trials designed to prove anti-fracture efficacy, there is strong evidence for hip fracture risk reduction through antiresorptive as well as bone-anabolic drugs [25]. In this regard, it is of note that the trend break of rising hip fracture incidence during the 2000s in women was associated with steeply increasing prescriptions of anti-osteoporotic drugs such as bisphosphonates [26, 27].
Analysis of incidence rate ratios (IRRs) during 2009–2018 in the 5-year age groups yielded decreasing annual incidences in women and men, albeit not statistically significant in all age groups. Explanations for inhomogeneous results across age groups remain tentative and speculative. For example, the absence of an effect in men and women aged 90 + and 95 + , respectively, might mirror lower prescription of anti-osteoporotic drugs compared with younger subjects [28]. Also, the onset of the trend break of hip fracture incidence during the 2000s was attenuated in women aged 80 + years compared with younger age groups [27]. The distinct decrease in women aged 75–89 might at least in part be attributed to the effect of menopausal hormone therapy several decades before. Eventually, younger men aged 50–59 years and women aged 55–64 years likewise displayed a significant decrease in hip fracture incidence during 2009–2018, which might reflect their improved nutritional status during childhood as opposed to older generations.
This study has several strengths and limitations. One of the strengths lies in the fact that numbers were calculated based on a nationwide register, which captures all hip fractures that occur within 1 year. Cohort effects that may occur when using incidence data from a specified catchment area in order to extrapolate findings to the entire nation have thus been precluded. Another strength lies in the correction factor that was applied for repeat hospital admissions of the same diagnosis. However, the study has also some limitations. For example, in theory, it might be possible that incorrect hospital discharge diagnoses are entered into the local hospital information system. However, since hip fracture is very costly and remuneration to the local health care provider depends on discharge diagnosis and medical service provided, it appears very unlikely that such procedural inadequacies could significantly affect hip fracture data as stored in the AHDR. Furthermore, rigorous in-hospital quality control programs in Austria ensure that discharge diagnoses are coded correctly by the respective physicians. Potential further limitations may apply to the assessment of the correction factor, variations of which over time could not be accounted for. In this respect, health insurance data from Germany reported a decrease in the correction factor from 1998 to 2009 from above 0.9 to values below 0.9 after the year 2001 [29]. It might thus be speculated that a correction factor of 0.9 represents a valid approximation for our study, in particular for data covering the years 1989–2008. In addition, we strived to assess this factor for a more recent time interval from a nationwide source and a regional database. Interestingly, our finding that the correction factor decreases with advancing age up to 90 years is likewise in line with results from the aforementioned German study [29]. On the other hand, its observed rise after 90 years of age is arguably due to the steep increase in in-hospital mortality [30]. Another limitation of the correction factor used could be the absence of S72 sub-codes in the nationwide dataset from the Austrian social insurance authorities, and different times of data acquisition in the nationwide dataset (2014–2016) vs. the regional database (2003–2013). Despite all these limitations, we deem the applied correction value as the best possible approximation for aggregate discharges in recent years. Moreover, IRRs for annual change 2009–2018 were largely independent of the kind of correction factor applied.
In conclusion, while absolute numbers of hip fractures showed a steep increase from 1989 to 2006, they remained fairly stable throughout the following 12 years of observation until 2018. This plateau was driven by a slight decrease of hip fracture numbers in the female population, and a “compensatory” slight increase in the male population at the same time. It is of note that the latter increase has persisted since the beginning of the 30-year period of observation, suggesting that “the worse” is not yet over, at least in men. Irrespective of the absolute numbers, and due to a remarkable population growth of the age groups 50 years and above, the overall age-standardized hip fracture incidence rates in fact decreased during the last 10 years of follow-up, in both women and men, albeit the amount of decrease in the latter was less pronounced. Thus, in terms of change in age-standardized incidence, the worst seems to be behind us. However, at the present, it cannot be precluded that due to the rapid aging of the Austrian population, this trend in the right direction will be compromised in the next few decades.
Change history
14 November 2021
The original version was revised due to an update in the funding note.
References
[Anonymous] (1991) Consensus development conference: prophylaxis and treatment of osteoporosis. Am J Med 90:107–110
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Eva Huber-Bachmann and Laura Bammer (ed) (2021) Austria. Data. Figures. Facts. Statistics Austria Federal Institution under Public Law Guglgasse 13, 1110 Vienna, Vienna.
Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper C, IOF Working Group on Epidemiology and Quality of Life (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–56
Dimai HP, Svedbom A, Fahrleitner-Pammer A, Pieber T, Resch H, Zwettler E, Chandran M, Borgstrom F (2011) Epidemiology of hip fractures in Austria: evidence for a change in the secular trend. Osteoporos Int 22:685–692
Ballane G, Cauley JA, Luckey MM, Fuleihan G (2014) Secular trends in hip fractures worldwide: opposing trends East versus West. J Bone Miner Res 29:1745–1755
Icks A, Haastert B, Wildner M, Becker C, Meyer G (2008) Trend of hip fracture incidence in Germany 1995–2004: a population-based study. Osteoporos Int 19:1139–1145
Concin H, Brozek W, Benedetto KP, Hafele H, Kopf J, Barenzung T, Schnetzer R, Schenk C, Stimpfl E, Waheed-Hutter U, Ulmer H, Rapp K, Zwettler E, Nagel G (2016) Hip fracture incidence 2003–2013 and projected cases until 2050 in Austria: a population-based study. Int J Public Health 61:1021–1030
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA, IOF CSA Working Group on Fracture Epidemiology (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22:1277–88
Kannus P, Niemi S, Parkkari J, Sievanen H (2018) Continuously declining incidence of hip fracture in Finland: Analysis of nationwide database in 1970–2016. Arch Gerontol Geriatr 77:64–67
Grossschadl F, Stronegger WJ (2013) Long-term trends in obesity among Austrian adults and its relation with the social gradient: 1973–2007. Eur J Public Health 23:306–312
Tang X, Liu G, Kang J, Hou Y, Jiang F, Yuan W, Shi J (2013) Obesity and risk of hip fracture in adults: a meta-analysis of prospective cohort studies. PLoS One 8:e55077
Sadeghi O, Saneei P, Nasiri M, Larijani B, Esmaillzadeh A (2017) Abdominal obesity and risk of hip fracture: a systematic review and meta-analysis of prospective studies. Adv Nutr 8:728–738
Cagnacci A, Venier M (2019) The controversial history of hormone replacement therapy. Medicina (Kaunas) 55. https://doi.org/10.3390/medicina55090602
Zhu L, Jiang X, Sun Y, Shu W (2016) Effect of hormone therapy on the risk of bone fractures: a systematic review and meta-analysis of randomized controlled trials. Menopause 23:461–470
Javaid MK, Eriksson JG, Kajantie E, Forsen T, Osmond C, Barker DJ, Cooper C (2011) Growth in childhood predicts hip fracture risk in later life. Osteoporos Int 22:69–73
Kanis JA, Johnell O, Oden A, Johansson H, De Laet C, Eisman JA, Fujiwara S, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Smoking and fracture risk: a meta-analysis. Osteoporos Int 16:155–162
Beaudoin C, Moore L, Gagne M, Bessette L, Ste-Marie LG, Brown JP, Jean S (2019) Performance of predictive tools to identify individuals at risk of non-traumatic fracture: a systematic review, meta-analysis, and meta-regression. Osteoporos Int 30:721–740
Dorner TE, Brath H, Kautzky-Willer A (2020) Sex-specific trends in smoking prevalence over seven years in different Austrian populations: results of a time-series cross-sectional analysis. BMJ Open 10:e035235,2019-035235
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE (2012) Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev (9):CD007146. https://doi.org/10.1002/14651858.CD007146.pub3
Lang T, Cauley JA, Tylavsky F, Bauer D, Cummings S, Harris TB, Health ABC Study (2010) Computed tomographic measurements of thigh muscle cross-sectional area and attenuation coefficient predict hip fracture: the health, aging, and body composition study. J Bone Miner Res 25:513–9
Sulander T, Martelin T, Sainio P, Rahkonen O, Nissinen A, Uutela A (2006) Trends and educational disparities in functional capacity among people aged 65–84 years. Int J Epidemiol 35:1255–1261
Angel B, Chahrour M, Halbwachs C, Peinhaupt C (2013) Nationaler Aktionsplan Bewegung - NAP.b. Ministry of Health, Vienna, Austria.
Yao P, Bennett D, Mafham M, Lin X, Chen Z, Armitage J, Clarke R (2019) Vitamin D and calcium for the prevention of fracture: a systematic review and meta-analysis. JAMA Netw Open 2:e1917789
Yang XC, Deng ZH, Wen T, Luo W, Xiao WF, Zhao RB, Li YS (2016) Network meta-analysis of pharmacological agents for osteoporosis treatment and fracture prevention. Cell Physiol Biochem 40:781–795
Hiligsmann M, Bruyere O, Roberfroid D, Dubois C, Parmentier Y, Carton J, Detilleux J, Gillet P, Reginster JY (2012) Trends in hip fracture incidence and in the prescription of antiosteoporosis medications during the same time period in Belgium (2000–2007). Arthritis Care Res (Hoboken) 64:744–750
Alves SM, Economou T, Oliveira C, Ribeiro AI, Neves N, Gomez-Barrena E, Pina MF (2013) Osteoporotic hip fractures: bisphosphonates sales and observed turning point in trend. A population-based retrospective study Bone 53:430–436
Brozek W, Reichardt B, Zwerina J, Dimai HP, Klaushofer K, Zwettler E (2016) Antiresorptive therapy and risk of mortality and refracture in osteoporosis-related hip fracture: a nationwide study. Osteoporos Int 27:387–396
Icks A, Haastert B, Glaeske G, Stumpf U, Windolf J, Hoffmann F (2012) Correction factor for the analysis of the hip fracture incidence–differences between age, sex, region, and calendar year. Wien Klin Wochenschr 124:391–394
Brozek W, Reichardt B, Kimberger O, Zwerina J, Dimai HP, Kritsch D, Klaushofer K, Zwettler E (2014) Mortality after hip fracture in Austria 2008–2011. Calcif Tissue Int 95:257–266
Acknowledgements
We would like to thank Dr Michaela Prammer-Waldhoer from Statistics Austria for providing us with the data from the Austrian Hospital Discharge Register.
Funding
Open access funding provided by Medical University of Graz. This study was funded by a medical research fund from the Medical University of Graz.
Author information
Authors and Affiliations
Contributions
All listed authors have seen and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
On behalf of all authors, the corresponding author herewith declares that all three of the following criteria for authorship are met:
1. Substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data;
2. Drafting the article or revising it critically for important intellectual content;
3. Approval of the version to be published and all subsequent versions.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Dimai, H.P., Reichardt, B., Zitt, E. et al. Thirty years of hip fracture incidence in Austria: is the worst over?. Osteoporos Int 33, 97–104 (2022). https://doi.org/10.1007/s00198-021-06086-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06086-z