Abstract
Objective
Pressure-volume (PV) curves are recorded after induction of complete muscle paralysis, which may limit their clinical use. The feasibility of recording PV curves without paralysis has not been tested. In 19 patients with acute respiratory distress syndrome (ARDS) and no hemodynamic instability we prospectively evaluated whether PV curves can be safely and reliably recorded under deep sedation without neuromuscular blockade.
Methods
After standardized sedation (continuous infusion of midazolam and fentanyl) PV curves were recorded during apneic sedation, defined as absence of respiratory effort during a 6-s expiratory pause and during paralysis induced by cis-atracurium.
Measurements and results
Agreement between PV curve parameters in the two conditions was evaluated. Curves were obtained from 10 cmH2O and from zero end-expiratory pressure in all patients under apneic sedation. In five patients propofol was given in addition to midazolam and fentanyl, and in two of them fluid resuscitation was needed. A strong agreement was found for respiratory system compliance and the lower inflection point and for chest wall compliance in the five patients whose esophageal pressure was measured. The variability of the measurements, however, should be taken into account in clinical practice.
Conclusion
Neuromuscular blockade can be dispensed with when recording PV curves in many ARDS patients. Reliable PV curves can be obtained under anesthesia alone, with no serious adverse effects.
Similar content being viewed by others
Introduction
In patients with acute respiratory distress syndrome (ARDS) the pressure-volume (PV) curve of the respiratory system may provide physiological information that is useful for clinical research and perhaps as an aid to treatment decisions. For instance, a protective ventilatory strategy partially tailored to the lower inflection point (LIP) of the PV curve decreased mortality in patients with ARDS [1]. A study by Ranieri et al. [2] compared changes in bronchoalveolar lavage results and cytokine levels in two groups of patients with acute lung injury and found the inflammatory cytokine profile during the first 36 h to be significantly lower in the group managed with adjustment of the positive end-expiratory pressure (PEEP) and tidal volumes (Vt) according to the PV curve. PV curves are usually recorded after administration of a neuromuscular blocking agent (NMBA) to eliminate spontaneous breathing during the recording, thus minimizing the effect of the chest wall [3]. The few studies investigating the specific effect of chest-wall muscles on the elastic properties of the respiratory system have produced conflicting data. Among studies in humans one found that muscle paralysis had no effect on chest wall compliance (Ccw) or respiratory system compliance [4] while another recorded a dramatic increase in total linear compliance (Clin) following NMBA administration [5]. The need for paralysis is often cited as an important limitation for the use of PV curve measurement particularly as repeated paralysis for multiple measurements may have significant adverse effect. In critically ill patients neuromuscular blockade can adversely affect muscle function [6], promote disuse-related wasting of the diaphragm [7], preclude monitoring of the sedation level [8], be associated with patient awareness or recall of paralysis [9, 10], and potentially contribute to the long-term functional impairment observed after ARDS [11].
The objective of the present study was to determine whether PV curves can be obtained safely and reliably under deep sedation without neuromuscular blockade in patients with ARDS. Our main hypothesis was that deep sedation minimizes the effect of the muscular component of Ccw on PV curves. To investigate this hypothesis we compared PV curves recorded with and without NMBA in patients with ARDS.
Methods and materials
In two intensive care units of the same hospital all 52 patients who received mechanical ventilation for ARDS [12] between July 2000 and August 2001 were screened to be prospectively included in the study, and 20 were enrolled (19 men, 1 woman), 19 of whom could be evaluated. Patients with the following criteria were excluded: documented history of chronic obstructive pulmonary disease, PaO2/FIO2 ratio less than 50 mmHg, presence of a chest tube, severe hemodynamic instability (starting or increase in the dose of vasopressors in the previous 4 h), contraindication for muscle paralysis or patients receiving continuous NMBA or difficulty to maintain plateau pressure at or below 30 cmH2O and SpO2 of 88% or more. The major reasons for exclusion were severe respiratory failure and multiple organ failure. No patient was excluded only because of a continuous infusion of NMBA, but eight of the excluded patients were already receiving NMBA. Patients were ventilated in volume-controlled mode. Tidal volume and respiratory rate were set by the physician in charge of the patient. Patients were ventilated with plateau pressure of 30 cmH2O or less and SpO2 88% or higher. Three ventilatory settings were imposed during the procedure: inspiratory/total time ratio of 0.33, FIO2 of 1, and PEEP at 10 cmH2O for at least 15 min before the measurements. The protocol was approved by the local ethics committee, and informed consent was obtained from the patients' next of kin.
PV curves were obtained with apneic sedation and NMBA-induced paralysis, in random order. A computer-controlled Servo Ventilator 900C (Siemens, Lund, Sweden) was used for tracing the curves with the oscillating low-flow insufflation method [13, 14]. After an expiration prolonged to 6 s during which the pressure was either maintained at PEEP (10 cmH2O) or brought to zero PEEP (ZEEP), a predefined target volume (1500 ml in our study) was insufflated during a 6-s-long inspiratory phase. Then after an end-inpiratory pause of 3 s the “clinical” RR, Vt, and PEEP 10 were applied. During insufflation the pressure was measured at airway opening. Esophageal pressure was recorded in seven patients who had marked spontaneous breathing activity before the procedure. The esophageal balloon (diameter 5.3 mm; Marquat, France) was positioned in the esophagus and inflated with 0.5 ml air. The validity of the pressure measurement was verified using the “occlusion test” and the balloon fixed in that position [15]. In two patients no reliable measurement could be obtained. Each PV curve was analyzed using a mathematical model that divides the curve into three segments separated by a LIP and upper inflection point (UIP) [16]. PV curves were obtained from a PEEP of 10 cmH2O and then from zero end-expiratory pressure. Comparison of LIP and UIP was performed from the ZEEP curves. Clin was defined as the slope of the linear part of the PV curve. Ccw and lung compliance were measured in patients by functional esophageal balloon. Alveolar recruitment was calculated by plotting the curve obtained from PEEP on the same volume axis as the ZEEP curve, using lung volume variation measured during a passive expiration from PEEP. Recruitment was defined as the volume difference between the curves for a given elastic pressure [14] and was measured at 20, 25, and 30 cmH2O elastic pressure.
At the time of inclusion all patients were sedated with continuous infusion of midazolam and fentanyl. The level of sedation was first standardized to obtain a modified Ramsay score of 5 before recording the PV curves; an increase in sedation was required to achieve this score in 12 patients. Apneic sedation was defined as absence of respiratory effort on the flow-time curve during an end-expiratory pause of 6-s. To achieve apneic sedation increasing doses of midazolam (up to 10 mg/h) and fentanyl (up to 300 μg/h) were administered as a continuous infusion; increments were 2 mg/h for midazolam and 50 μg/h for fentanyl every 10 min. When full doses failed to achieve apnea, a continuous infusion of propofol was added with 150 mg/h increments every 10 min. Five patients received norepinephrine and for one of them, the vasopressor was combined with dobutamine. A drop in oxygen saturation to SpO2 less than 88% or a decrease in mean arterial pressure greater than 10% of baseline despite 500 ml intravenous fluid administration prompted discontinuation of the procedure. The degree of neuromuscular blockade was quantified using the posttetanic count, defined as the number of evoked responses of the adductor pollicis muscle to 20 ulnar nerve stimulations following a 5-s tetanic stimulation [17]. The nerve was stimulated with a posttetanic count innervator device (Fisher Paykel, Auckland, New Zealand) connected to skin surface electrodes. Full paralysis was defined as a posttetanic count less than 5 and was achieved using cis-atracurium administration. If paralysis was the first condition achieved, recording of PV curves for the second condition (apneic sedation) was started only after full recovery of diaphragmatic paralysis (train of four = 4 at the adductor pollicis). If apneic sedation was recorded first and spontaneous breathing activity was initially present, the second recording was started after recovery of a spontaneous breathing activity during an expiratory pause. The level of the sedation required to perform the PV curve was kept only for the duration of the measurements.
Agreement between PV curve parameters and alveolar recruitment recorded in both conditions was evaluated using the method of Bland and Altman [18]. These results were expressed as bias, limits, and 95% confidence interval (95%CI) of bias. Bias was significant if 0 was not included in the 95%CI. Other results were expressed as mean ± standard deviation. Means were compared using the Wilcoxon test. Differences with p values less than 0.05 were considered statistically significant. StatView software (version 5.1, SAS Institute) was used for all analysis.
Results
The first condition was paralysis in 11 patients and apneic sedation in 9 patients. Before randomization 9 patients had at least one inspiratory effort during the 6-s expiratory pause despite Ramsay 5 sedation. The mean duration between the two conditions was 48 ± 16 min when the first condition was paralysis, and 56 ± 23 min when it was apneic sedation. In 15 patients apneic sedation was achieved using midazolam and fentanyl, with mean continuous hourly doses of midazolam and fentanyl during the procedure of 0.12 mg/kg and 4.1 μg/kg, respectively; no adverse hemodynamic or respiratory events were recorded. In the five remaining patients inspiratory or expiratory efforts occurred despite maximal continuous doses of midazolam and fentanyl (10 mg/h midazolam and 300 μg/h fentanyl), and propofol was therefore added as a continuous infusion. The mean propofol dose was 0.66 ± 0.23 mg/kg and the mean infusion duration was 14 ± 4 min. A blood pressure drop requiring infusion of 500 ml fluid occurred in two patients, both of whom recovered their baseline blood pressure values after administration of about 250 ml fluid. The mean cis-atracurium dose needed to achieve full paralysis was 0.19 ± 0.04 mg/kg. In one patient poor quality of the recorded signal in both conditions precluded reliable automatic modeling. Therefore PV curves were studied in 19 patients, whose main characteristics are shown in Table 1. PV curves maneuvers were always well tolerated with no side effect.
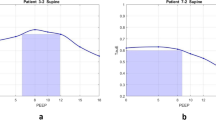
Measurements of mean Clin, Ccw, lung compliance, PEEPtot, volume retained by PEEP, LIP, and UIP in the two conditions are summarized in Table 2. Regarding PV curve characteristics, mean Clin did not differ significantly with paralysis and apneic sedation. The bias of agreement for Clin was –0.2 ml/cmH2O with a 95%CI of bias of –3.5 to 3.0. The limits of agreement are shown in Fig. 1. Values of the bias of agreement for compliance measured at 20, 30, and 40 cmH2O of airway pressures were of the same magnitude. In the five patients with reliable Pes recordings Ccw did not differ significantly between apneic sedation and paralysis. The bias of agreement for Ccw was –0.7 ml/cmH2O with a 95%CI of bias of –5.3 to 3.9. Mean LIP did not differ significantly between paralysis and apneic sedation (bias –0.3 cmH2O and 95%CI –1.0 to 0.4; Fig. 2), nor did the mean UIP differ significantly (bias –0.4 cmH2O and 95%CI –1.9 to 1.2). In eight patients no UIP was recorded under paralysis or apneic sedation; one patient had an UIP (17.2 cmH2O) under paralysis but not under apneic sedation, and two had an UIP under apneic sedation but not under paralysis (mean UIP 17.5 ± 1 cmH2O). Mean PEEPtot just before PV curve recording did not differ significantly under paralysis and apneic sedation. The mean ratio of recruited volume at 20 cmH2O over the volume retained by PEEP was 28.6 ± 18.8% under paralysis and 27.5 ± 17.1% under apneic sedation (p = 0.64). Bias of agreement for alveolar recruitment was 9.6 ml and –2.2 ml at 15 and 20 cmH2O of airway pressure, respectively, and corresponding 95%CIs were –29.7 to 48.9 and –29 to 24.6. Figure 3 shows data for alveolar recruitment at 20 cmH2O. Plots for UIP and recruitment at P25 and P30 are presented in the Electronic Supplementary Material.
Bland and Altman plot of the agreement for linear compliance (Clin) with and without paralysis in 19 patients. The figure shows the difference in Clin values in the same patients compared with mean Clin as well as the mean of differences (bias) and limits of agreement ( ± 2 SD of differences). Bias = –0.2 ml/cmH2O; 95% confidence interval 3.5 to 3.1; 1.96 SD = 16.1
Bland and Altman plot of the agreement for LIP in the 16 patients with an LIP. The figure shows the difference in LIP values in the same patients compared with mean LIP as well as the mean of differences (bias) and limits of agreement ( ± 2 SD of differences). Bias = –0.3 ml; 95% confidence interval = –1.0 to 0.4; 1.96 SD = 3.1
Bland and Altman plot of the agreement for recruitment measured at 20 cmH2O of airway pressure (P20) in 17 patients. The figure shows the difference in P20 recruitment values in the same patients compared with mean P20 recruitment as well as the mean of differences (bias) and limits of agreement ( ± 2 SD of differences). Bias = –2.2 ml; 95% confidence interval: 29 to 24.6; 1.96 SD = 124.3
Discussion
The main findings from this study are as follows: (a) in most patients receiving mechanical ventilation for ARDS PV curves were recorded during apneic sedation without NMBA administration and without major side effects. (b) PV curves recorded with apneic sedation and paralysis showed a high level of agreement for Clin of the respiratory system, linear Ccw, LIP, UIP. (c) Due to the high individual variability the clinical interpretation of the PV curve should be made with caution in individual cases.
Methodological issues
We took several steps to avoid loss of lung volume throughout the study procedure. The effect of prolonged expiratory and inspiratory pauses was minimized by using relatively long time intervals with standardized ventilation between the two PV curve recordings (at least 10 min). We also kept endotracheal suctioning to a minimum during the study procedure. We found no differences in mean volume retained by PEEP between the two conditions, indicating that absolute lung volume probably remained unchanged. Second, our automatic recording and modeling method was highly reproducible and minimized bias in curve analysis and interpretation. Third, we monitored the depth of neuromuscular blockade using the posttetanic count. The blockade of the diaphragm is much slower (with efficient dose) than that of the adductor pollicis [19]. Then the TOF cannot be used. A posttetanic count less than 5 was required; this value indicated an at least 80% decrease in diaphragm strength and therefore a greater than 80% decrease in intercostal muscle strength [19]. This high level of muscle paralysis provided an optimal contrast with the apneic sedation condition. When paralysis was the first condition assigned by randomization, we waited until full muscle function recovery before starting apneic sedation. The diaphragmatic neuromuscular recovery is much faster than the peripheral muscles.
Feasibility and safety
PV curves in the apneic sedation condition were successfully recorded using midazolam and fentanyl alone in 15 patients, none of whom experienced arterial hypotension. We fixed a threshold for the injection rate of the two sedative drugs and added the short-lasting sedative-hypnotic propofol for no longer than 15 min if needed to abolish inspiratory effort. Of the five patients who required addition of a propofol infusion two experienced arterial hypotension followed by a return to normal blood pressure values within 4 min of initiating moderate fluid expansion; no change in oxygenation was observed in these patients. The low propofol dose and administration as a continuous infusion (instead of a bolus) explain the good hemodynamic safety profile. However, we did not perform invasive hemodynamic assessments or specifically evaluated other potential middle term adverse effects of this procedure. The risk associated with the use of NMBA implies that they should be given only if the potential benefit justifies these risks. Although PV curves were recorded in 20 patients, the software failed to model the curve accurately in one because of large cardiac oscillations superimposed on the insufflation pressure in both conditions and this patient was excluded from the analysis.
Agreement between PV curves
The low value for the bias regarding Clin indicates that there was no systematic deviation between the two recording methods of the PV curve for this parameter. The interindividual variability in the measurements was statistically low since the standard deviation in interindividual differences accounted for only 12% of the mean Clin value. This standard deviation determines the B and A limits of agreement and consequently the number of patients outside these limits. A single patient fell outside the limits of agreement. In this patient, although criteria for ARDS were present, the elastic properties of the respiratory system differed markedly from those found in the other patients: Clin of the respiratory system was high in both conditions (121 ml/cmH2O with paralysis and 138 ml/cmH2O with apneic sedation) but was less than 90 ml/cmH2O during paralysis in all other patients. Thus respiratory system compliance in this patient was probably abnormally high at baseline before the onset of ARDS. However, despite the satisfactory statistical agreement between the two methods the maximal difference between the two conditions in our population was 16 ml/cmH2O, explained both by variation due to paralysis and by the intraindividual variability in this measurement. The high level of statistical agreement for Clin can also be ascribed to the good agreement for Ccw in both conditions. Although available for only five patients, bias accounted for 3% of linear Ccw in the paralysis condition, and the SD (47.5) of bias for only 20% of compliance. These findings establish that the elastic properties of the respiratory system are similar with apneic sedation and with paralysis in ARDS patients. Nevertheless, the highest difference between values obtained in the two conditions was of 30% and, as observed for Clin, and the method should make one cautious regarding individual application of the PV curve.
To our knowledge, no previous studies have compared respiratory system and chest wall mechanical properties as assessed by the PV curve with and without neuromuscular blockade in a homogeneous population of patients with ARDS. In a study of 13 ICU patients Conti et al. [20] found that total pulmonary and Ccw were identical with apneic sedation and with paralysis. However, the population was heterogeneous in terms of diagnoses and sedative drugs (thiopental or propofol), and the sedation target was not defined clearly. Furthermore, the two conditions were studied in the same order in all patients (sedation first), and effective compliance, i.e., Vt divided by change in pressure, was recorded instead of total PV curves. Two studies of thoracopulmonary elastic properties in healthy anesthetized subjects showed that chest wall mechanics were similar with and without neuromuscular blockade. Westbrook et al. [4] measured thoracic and pulmonary volumes (using plethysmography) as well as total compliance and Ccw at 45% of functional residual capacity in five healthy subjects under three conditions: wakefulness, apneic anesthesia with pentothal monosodium and meperidine, and muscle paralysis with a constant infusion of succinylcholine chloride, in that order. Anesthesia decreased the functional residual capacity and the total compliance of the respiratory system. Nevertheless, addition of the NMBA did not significantly lower compliance and induced a nonsignificant increase in Ccw. Behrakis et al. [21] obtained similar results regarding effective thoracopulmonary compliance. Thus the results of published studies in healthy individuals indicate that an anesthetic-sedative combination exerts major effects on elastic thoracopulmonary properties, whereas neuromuscular blockade has no additive effects.
The relative contributions of lung volume loss and paralysis on Ccw in ARDS are not well known. Here and in an earlier study [20] Ccw values in apneic sedation were similar to those usually found in healthy awake individuals and lower than those found in healthy individuals during sleep. In some animal studies the decrease in compliance has been explained by histological edema [22]. However, the muscular component of chest-wall elastic properties seemed to play only a minor role in our patients with ARDS.
Inflection points and recruitment agreements
The LIP is viewed as the mean value of a range of opening pressures and its presence reflects the recruitability of the lung [23, 24, 25]. In our study, agreement between the two conditions was perfect regarding presence of the LIP. All the patients with a LIP on paralysis condition had also a LIP on deep sedation condition. Thus the PV curve recorded under sedation alone was reliable for determining the presence of recruitment in patients with ARDS.
However, even with a satisfactory statistical agreement the maximum deviation observed between the two conditions in our sample is of 3 cmH2O, which may correspond, at a true LIP of 10 cmH2O, to 7–13 cmH2O in sedation conditions. This value of 3 cmH2O is precisely the observed variability in nearly 40% of the patients with the other methods of PV curve achievement [26]. We therefore need to take into account this variability in the clinical application of LIP.
Reproducibility was unsatisfactory with the standard deviation of agreement accounting for 35% of the mean recruitment value at 15 cmH2O and 49% at 20 cmH2O under paralysis. Recruitment is greatest at the beginning of insufflation and ends around the mean UIP value when present. A single patient fell outside the limits of agreement at 15 cmH2O. The mean recruitment volumes as well as the ratio of mean recruited volume/mean volume retained by PEEP were similar under both conditions. Finally, Clin and LIP values as well as the proportion recruited volumes with respect to the volume retained by PEEP showed no significant difference between the two conditions.
Conclusion
Our study included a majority of patients with primary ARDS, but the results were similar in the five patients with secondary ARDS. It is important to note, however, that we excluded patients with hemodynamic instability. In patients with ARDS and no hemodynamic instability NMBA administration is therefore not indispensable for obtaining PV curves in ARDS patients. Apneic sedation can be used instead as an alternative. However, the level of intraindividual variability in measurements indicates that PV curve without paralysis should be used with caution at the bedside for clinical management. No serious hemodynamic or respiratory adverse events occurred with our sedation regimen. Reducing NMBA use may help to minimize the short- and long-term adverse effects associated with these agents and make easier the performance of repeated measurements of PV curves. Because PV curves are not frequently repeated in a given patient, the risk associated with possible down-side effects of repeated deep sedation is also minimal with our technique.
References
Amato M, Barbas C, Medeiros D, Magaldi R, Schettino G, Lorenzi-Filho G, Kairalla R, Deheinzelin D, Munoz C, Oliveira R, Takagaki T, Ribeiro Carvalho C (1998) Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338:347–354
Ranieri VM, Suter PM, Tortorella C, De Tullio R, Dayer JM, Brienza A, Bruno F, Slutsky AS (1999) Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA 282:54–61
Matamis D, Lemaire F, Harf A, Brun-Buisson C, Ansquer JC, Atlan G (1984) Total respiratory pressure-volume curves in the adult respiratory distress syndrome. Chest 86:58–66
Westbrook PR, Stubbs SE, Sessler AD, Rehder K, Hyatt RE (1973) Effets of anesthesia and muscle paralysis on respiratory mechanics in normal man. J Appl Physiol 34:81–86
Van Lith P, Neal Johnson F, Turner Sharp (1967) Respiratory elastances in relaxed and paralyzed states in normal and abnormal men. J Appl Physiol 23:475–486
Segredo V, Caldwell JE, Matthay MA, Sharma ML, Gruenke LD, Miller RD (1992) Persistent paralysis in critically ill patients after long-term administration of vecuronium. N Engl J Med 327:524–528
Sassoon CS (2002) Ventilator-associated diaphragmatic dysfunction. Am J Respir Crit Care Med 166:1017–1018
Kress JP, Pohlman AS, O'Connor MF, Hall JB (2000) Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 342:1471–1477
Rotondi AJ, Chelluri L, Sirio C, Mendelsohn A, Schulz R, Belle S, Im K, Donahoe M, Pinsky MR (2002) Patients' recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med 30:746–752
Johnson KL, Cheung RB, Johnson SB, Roberts M, Niblett J, Manson D (1999) Therapeutic paralysis of critically ill trauma patients: perceptions of patients and their family members. Am J Crit Care 8:490–498
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 348:683–692
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R, Committee C (1994) The American-European Consensus Conference on ARDS Definitions, Mechanisms, Relevant Outcomes, and Clinical Trial Coordination. Am J Respir Crit Care Med 149:818–824
Jonson B, Richard JC, Straus C, Mancebo J, Lemaire F, Brochard L (1999) Pressure-volume curves and compliance in acute lung injury: evidence of recruitment above the lower inflection point. Am J Respir Crit Care Med 159:1172–1178
Maggiore SM, Jonson B, Richard JC, Jaber S, Lemaire F, Brochard L (2001) Alveolar derecruitment at decremental positive end-expiratory pressure levels in acute lung injury: comparison with the lower inflection point, oxygenation, and compliance. Am J Respir Crit Care Med 164:795–801
Baydur A, Cha EJ, Sassoon CS (1987) Validation of esophageal balloon technique at different lung volumes and postures. J Appl Physiol 62:315–321
Svantesson C, Drefeldt B, Sigurdsson S, Larsson A, Brochard L, Jonson B (1999) A single computer-controlled mechanical insufflation allows determination of the pressure-volume relationship of the respiratory system. J Clin Monit Comput 15:9–16
Werba A, Klezl M, Schramm W, Langenecker S, Müller C, Gosch M, Spiss CK (1993) The level of neurovascular block needed to suppress diaphragmatic movement during tracheal suction in patients with raised intracranial pressure: a study with vecuronium and atracurium. Anasesthesia 48:301–303
Bland MJ, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 8:307–310
Pansard JL, Chauvin M, Lebrault C, Gauneau P, Duvaldestin P (1987) Effect of an intubating dose of succinylcholine and atracurium on the diaphragm and the adductor pollicis muscle in humans. Anesthesiology 67:326–330
Conti G, Vilardi V, Rocco M, DeBlasi RA, Lappa A, Bufi M, Antonelli M, Gasparetto A (1995) Paralysis has no effect on chest wall and respiratory system mechanics of mechanically ventilated, sedated patients. Intensive Care Med 21:808–812
Behrakis PK, Higgs BD, Baydur A, Zin WA, Milic-Emili J (1983) Respiratory mechanics during halothane anesthesia and anesthesia-paralysis in humans. J Appl Physiol 55:1085–1092
Mutoh T, Lamm W-J, Embree L-J, Hildebrandt J, Albert R-K (1992) Volume infusion produces abdominal distension, lung compression and chest wall stiffening in pigs. J Appl Physiol 72:575–582
Hickling KG (1998) The pressure-volume curve is greatly modified by recruitment. A mathematical model of ARDS lungs. Am J Respir Crit Care Med 158:194–202
Hickling KG (2001) Best compliance during a decremental, but not incremental, positive end-expiratory pressure trial is related to open lung positive end-expiratory pressure. Am J Respir Crit Care Med 163:69–78
Jonson B, Svantesson C (1999) Elastic pressure-volume curves: what information do they convey? Thorax 54:82–87
Mehta S, Stewart TE, MacDonald R, Hallett D, Banayan D, Lapinsky S, Slutsky A (2003) Temporal change, reproducibility, and interobserver variability in pressure-volume curves in adults with acute lung injury and acute respiratory distress syndrome. Crit Care Med 31:2118–2125
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Decailliot, F., Demoule, A., Maggiore, S.M. et al. Pressure-volume curves with and without muscle paralysis in acute respiratory distress syndrome. Intensive Care Med 32, 1322–1328 (2006). https://doi.org/10.1007/s00134-006-0265-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0265-8