Abstract
Objective
To evaluate the incidence, risk factors, foci, isolated organisms, and outcomes of infections in the survivors of out-of-hospital cardiac arrest (OHCA) within the first 7 days after resuscitation.
Design and setting
Retrospective cohort study in the intensive care unit of a university hospital.
Patients and participants
We enrolled 117 survivors of adult nontraumatic OHCA victims who survived more than 24 h between January 1999 and May 2004. We collected patients’ demographics, the causes and initial electrocardiographic rhythm of cardiac arrest, and the process of cardiopulmonary resuscitation. The incidence, clinical presentations and outcomes of infections occurring in the first 7 days after resuscitation were evaluated. Variables were compared between the infected and noninfected patients.
Measurements and results
Among our OHCA survivors asystole was the most common initial rhythm (66%). Eighty-three patients (71%) were found to have infection. Pneumonia was the most common infection (61%) followed by bacteremia (13%). Although the Gram-negative bacteria were responsible for most infections, the most commonly isolated organism was Staphylococcus aureus. The infection group had more patients with dementia and noncardiac causes of OHCA. The survival curves did not differ significantly between infection and noninfection groups.
Conclusions
Infections were common in OHCA survivors during the first 7 days. The most common responsible organisms were Gram-negative bacteria, and the most commonly isolated organism was S. aureus. Infections in the early stage after return of spontaneous circulation did not change the hospital mortality and hospitalization duration.
Similar content being viewed by others
Introduction
With improvements in technique and medication in resuscitation more patients are surviving the out-of-hospital cardiac arrest (OHCA) [1]. Postresuscitation care is becoming increasingly important with the increased return of spontaneous circulation (ROSC) rate. Infections play a major role in postresuscitation care, and appropriate choice of empirical antibiotics for infections is important. Efforts at resuscitation can profoundly decrease the levels of cell-medicated immunity by imposing extreme stress [2]. Moreover, both human and animal studies demonstrate that most postresuscitation infections result from bacterial translocation from the gastrointestinal (GI) tract into the bloodstream due to mesenteric ischemia [3, 4]. However, recent studies show a predominance of infection in the Gram-positive organisms for cardiac arrest survivors [5, 6]. Previous studies on postresuscitation infections have enrolled cardiac arrest patients both inside and outside of hospital patients [5, 6]. There are only few data addressing infections in OHCA survivors, especially in the early stage after ROSC. The objective of this retrospective study was to evaluate the incidence, risk factors, foci, isolated organisms of infections in OHCA survivors in the first 7 days after ROSC.
Materials and methods
This retrospective cohort study approved by the institutional review board (IRB) enrolled survivors of OHCA victims from January 1999 to May 2004. We reviewed both electronic and handwritten medical records of OHCA patients, who were successfully resuscitated in the emergency department (ED) and admitted to the intensive care unit (ICU) of the university hospital from January 1999 to May 2004. This university hospital is a tertiary referred center hospital with about 100,000 ED visits per year [1, 7]. The successfully resuscitated OHCA patients were admitted to the ICU and received postresuscitation care. Eligible samples were from nontraumatic OHCA patients who survived more than 24 h and were older than 18 years old.
From the individual charts we collected the following information: underlying comorbidity (preexisting medical conditions in addition to OHCA), the possible cause and initial electrocardiographic (ECG) rhythm of cardiac arrest, the duration of cardiopulmonary resuscitation (CPR), the presence of witnessed collapse and bystander CPR, the best Glasgow Coma Score (GCS), and highest Acute Physiology and Chronic Health Evaluation (APACHE) II score in the first 24 h after ROSC, mean blood pressure 30 min after ROSC, leukocyte count sampled at resuscitation, development of infection in the first 7 days after ROSC, and laboratory and radiological findings. We also collected the timing of antibiotic administration. The presence or absence of witnessed aspiration, diarrhea, and GI bleeding during the first 24 h after ROSC were recorded. The hospital mortality and the hospitalization duration of the survivors were also recorded.
The causes of OHCA were divided into two major parts, namely cardiac causes and noncardiac causes. The cardiac causes included acute coronary syndrome and fatal arrhythmia without electrolyte imbalance. The noncardiac causes included respiratory cause, infectious cause, massive GI bleeding, hyperkalemia, central nervous system (CNS) lesion, and others. Respiratory events included asthma attack, chronic obstructive lung disease with exacerbation, sputum impaction, and suffocation. Infectious causes were considered when previously existing infections were noted at ROSC and no other cause of OHCA could be found. Massive GI bleeding was recorded when hematemesis or bulky tarry stool with profoundly decreased hemoglobin level (<8 gm/dl). Hyperkalemia was considered when blood potassium level exceeded 6 mmol/l, and no other OHCA cause could be found. CNS lesions included brainstem infarct, cerebral ischemic infarct, and subarachoid hemorrhage documented by brain image, such as brain computed tomography (CT) and magnetic resonance image.
The events occurred within 24 h after ROSC were defined as following: witnessed aspiration was defined when such event was documented in the chart; diarrhea was defined as one or more liquid stools per hour within 3 h according to the nurse’s recording; GI bleeding was considered when the guaiac test was positive for stool sample or nasogastric tube drainage. Patients discharged with full GCS (15 points) were considered to have good neurological recovery.
Pneumonia was defined by the presence of new pulmonary infiltrate on chest radiography, persistent for at least 48 h plus two of the followings: body temperature higher than 38.5°C or lower than 35°C, leukocyte count higher than 10,000/µl or lower than 3,000/µl, purulent sputum or change in the character of the sputum. Ventilator-associated pneumonia was considered when a patient on mechanical ventilation at least 48 h developed pneumonia without initial pulmonary infiltrate at ROSC [8, 9]. Urinary tract infection (UTI) was defined by the presence of pyuria plus isolation of more than 105 organisms per milliliter of urine. Bacteremia was defined as positive blood cultures for at least two sets at separate sites or single blood culture with clinical compatibility. Coagulase-negative staphylococci and other common skin flora isolated in single blood culture without clinical risk and compatible disease course were judged as contamination [10, 11, 12, 13]. Intra-abdominal infection was considered when the leukocyte of the ascite was more than 250/µl, or imaging studies of the abdomen including ultrasonography and CT showed swollen or perforated bowel in a febrile patient. Vascular catheter-related infection was defined by positive catheter culture (≥15 colony forming units on semiquantitative culture) considered to be the source of infection. Skin defect associated Infections were defined by the presence of pus and inflammation of the site. Empyema was considered when pleural effusion showed frankly pus plus positive Gram’s stain.
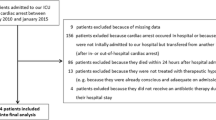
There were 898 OHCA patients in the university hospital during the review period. Of these, 374 gained ROSC; 288 were admitted to ICU. We collected 174 non-traumatic adult patients who were admitted to the ICU of the university hospital. Fifty-six patients survived less than 24 h and one patient with missing data were excluded from final analyses. Finally, 117 patients were included in the study. Figure 1 presents the flow diagram. Their mean age was 71.7±15.4 years; there were 55 men and 62 women. The cardiac causes accounted for one-fourth of OHCA (n=29, 25%). Asystole was the most common initial rhythm of ECG (n=77, 66%) followed by pulseless electrical activity (n=26, 22%) and ventricular tachycardia/fibrillation (n=14, 12%). Forty-five patients (38%) survived hospitalization. Among survivors six patients (5%) were discharged with full GCS (15 points), and 23 (19%) were dependent on others for daily support due to moderate to severe overall disability. Sixteen patients (14%) entered a vegetative state when discharged. Patients were divided into two groups, those with (n=83) and those without infection (n=34), according to the presence or absence of any documented infection in the first 7 days after ROSC. Table 1 compares the demographics, resuscitation condition, and outcome in the two groups. There were more patients with dementia and the noncardiac causes of cardiac arrest in the infection group. All the patients with dementia had infection.
Data were saved in a Microsoft Excel database (Excel 2002; Microsoft, Seattle, Wash., USA) and then analyzed with SPSS software for Windows (release 10.0, SPSS, Chicago, Ill., USA). Mean and standard deviation values were used to describe approximately normally distributed data. Student’s t test was used for comparisons of normally distributed continuous data of the two groups. Binomial variables were analyzed by the χ2 or Fisher’s exact test. Survival curves were determined by the Kaplan-Meier method. The log-rank test was used to compare curves. A p value less than 0.05 was regarded as statistically significant.
Results
Fourteen of 29 (48%) patients with cardiac causes and 69 of 88 (78%) with noncardiac cause of OHCA developed infection (p=0.002). Sixteen patients were diagnosed to have infectious cause of OHCA (11 pneumonia, two intra-abdominal infection, one bacteremia, one UTI, and one drainage wound infection). The infection group also had more patients with initial asystole rhythm. Noncardiac causes of cardiac arrest remained associated with infection after logistic regression analysis (odds ratio=3.270, 95% confidence interval=1.338–7.995, p=0.009). Antibiotic use before OHCA did not differ between these two groups. However, it was not surprising that the infection group had more patients with antibiotic use within 24 h after ROSC. No significant statistical differences were found in the events during CPR and within 24 h, leukocyte count, hospital mortality, or hospitalization duration in survivors between the infection and noninfection groups. The survival curves between the infection and noninfection group did not show significantly statistic difference as well (p=0.237).
There were 83 patients and 105 identified infections in the infection group. The incidence of early infection in OHCA survivors was 168/1000 person-days. Among these patients with infection five were discharged from hospital within 1 month before OHCA episode, seven lived in a nursing home before cardiac arrest, and one patient had both characteristics. Pneumonia was the most common infection (n=71, 61%) followed by bacteremia (n=15, 13%), UTI (n=9, 8%), intra-abdominal infection (n=4, 3%), and others (6, 5%). Other infections were found in three patients with skin defect associated infection, two with empyema, and one with vascular catheter infection. Fourteen patients had more than two infection foci. Among pneumonia patients eight (7%) fulfilled the criteria of ventilator-associated pneumonia in the first 7 days after ROSC.
Gram-negative bacteria were responsible for most infections. However, the single most common isolated organism was Staphylococcus aureus (Table 2). The most commonly isolated organisms of pneumonia were S. aureus, Klebsiella pneumoniae, and Acinetobacter baumannii. Escherichia coli was the most commonly isolated organism of UTI. The most commonly isolated organisms of bacteremia were Staphylococcus spp. (S. aureus and S. epidermis) and Burkholderia cepacia. Twelve patients with pneumonia, one with bacteremia, two with UTI, and four with other infection had more than two isolated organisms.
Discussion
This study examained infection-related issues in the first 7 days after successful resuscitation in OHCA patients who were admitted to the ICU and survived more than 24 h. Infections were common in these patients and the most common infection was pneumonia. Although the most responsible organisms were Gram-negative bacteria, the most commonly isolated organism was S. aureus. Infections in the first 7 days after ROSC did not change hospital mortality or hospitalization duration.
Infectious complications are common in successful resuscitated cardiac arrest patients [4, 5, 6]. Gajic et al. [5] reported new infections in 46% of survivors of cardiac arrest during medical ICU stay. Their study included not only OHCA patients but also in-hospital cardiac arrest patients. One-half of their patients received antibiotics before cardiac arrest. They did not report the overall infection rate among survivors after resuscitation. In our study infections were found in 71% of OHCA survivors in the first 7 days after ROSC. Since it was difficult to determine the exact onset timing of infections in OHCA patients, we hypothesized that infections existed before OHCA could be explored in 1–3 days after cardiac arrest. There were 72 patients with antibiotic use within 24 h after ROSC, but only 4 patients were documented in the charts to have used antibiotic before cardiac arrest. These results suggest that infection work-up is mandatory in OHCA survivors, and early appropriate antibiotic treatment is highly recommended.
Pneumonia was the most common type of infection in the current study. This was compatible to earlier studies. Gajic et al. [5] reported 30% of cardiac arrest patients developed new pneumonia after resuscitation. Rello et al. [6] reported pneumonia in 24% survivors of cardiac arrest who were admitted to medical and surgical ICU. The occurrence of pneumonia was also reported in 29% survivors of ventricular fibrillation [14]. To our knowledge, there are no data concerning the overall incidence of pneumonia in successfully resuscitated OHCA patients. Our data reveal the occurrence of pneumonia in 61% OHCA survivors in the first 7 days, which was higher than the figure in the above studies. This may be due in part to the fact that our study included pneumonia occurring before and after OHCA. The high incidence of suffocation related OHCA in our study may also explain the higher occurrence of pneumonia. Rello et al. [6] reported S. aureus as the most frequently isolated organism of pneumonia in survivors of cardiac arrest. Gram-positive cocci represented 57.1% of isolated organisms of pneumonia in their study. In our study S. aureus, K. pneumoniae, and A. baumannii were the most common isolated organisms of pneumonia. The emergent endotracheal intubation during resuscitation was probably the major reason leading the predominance of S. aureus. It is hard to keep strictly antiseptic conditions in emergent intubation because the patients are usually not well prepared, and aspiration and repeated intubation are common [6]. However, in contrast to the findings of Rello et al. [6], Gram-negative bacteria accounted for 78.9% cases of pneumonia in our study.
In our study the incidence of bacteremia was 13%. This figure is similar to that in the study by Gajic et al. [5]. However, they did not mention the isolated organisms of bacteremia. Gaussorgues et al. [3] reported 39% resuscitated patients of cardiac arrest developed bacteremia. In their prospective study the most common isolated organism in the blood was Streptococcus D, followed by E. coli. Staphylococcus was isolated in only one case of central venous catheter superinfection. In their study 12 of 13 patients in the bacteremic group but none in the nonbacteremic group developed diarrhea. There was a high association between diarrhea and bacteremia. They suggested that an intestinal origin of bacteremia due to intestinal leakage caused by mesenteric ischemia resulted from a low cardiac output. In our study both Staphylococcus spp. and B. cepacia were the most frequently isolated organisms of bacteremia. Since Staphylococcus spp. and B. cepacia are often related to invasive procedures [15, 16, 17], the frequent use of invasive procedures during resuscitation may explain the higher frequency of isolated Staphylococcus and B. cepacia from blood in our study.
In our study 14 of 29 (48%) patients with cardiac causes and 69 of 88 (78%) with noncardiac causes of OHCA developed infection. It is well known that cardiac causes of OHCA are usually sudden and severe in OHCA patients. Most patients with cardiac causes either die away or recover soon, and hence there is less time for infection to develop. The fortunate survivors recovered well after necessary therapeutic intervention, and infection was less common in these patients. Therefore the infection group was associated with fewer cardiac causes of OHCA. Asystole was the most common initial rhythm of ECG in this study. There was lower ventricular fibrillation rate of OHCA patients in Taiwan [7, 18] and Japan [19] than in Western countries [20, 21]. In our series the infection group had more patients with initial asystole rhythm. The infection group also had more patients with underlying comorbidity with dementia. Dementia and noncardiac causes of cardiac arrest were still associated with infection after logistic regression analysis. In our study hospital mortality and hospitalization duration did not differ significantly between the infection and noninfection groups. The common and appropriate use of antibiotics in the survivors of OHCA may explain these results. These results also suggest that infection in the first 7 days after ROSC was probably not the main factor that affected outcome.
There are several limitations in our study. First, because patients who died early may not have been found to have infection, we excluded patients who survived less than 24 h. Therefore not all the adult and nontraumatic OHCA survivors during the review period were enrolled in the study. Second, there are different definitions of infections in different studies, which results in the different incidences of infections. We tried to minimize the difference by using the most commonly used definition of each infection. Third, we were limited by the retrospective design of the study.
Our study described the infections in the first 7 days after resuscitation of OHCA survivors. We found that infections were common among these patients. Although Gram-negative bacteria were responsible for most infections, the most commonly isolated organism was S. aureus. Infections in the first 7 days after ROSC did not change the hospital mortality and hospitalization duration.
References
Weng TI, Huang CH, Ma MH, Chang WT, Liu SC, Wang TD, Chen WJ (2004) Improving the rate of spontaneous circulation for out-of-hospital cardiac arrests with a formal, structured emergency resuscitation team. Resuscitation 60:137–142
Soppi E, Lindroos M, Nikoskelainen J, Kalliomaki JL (1984) Effect of cardiopulmonary resuscitation-induced stress on cell-mediated immunity. Intensive Care Med 10:287–292
Gaussorgues P, Gueugniaud PY, Vedrinne JM, Salord F, Mercatello A, Robert D (1988) Bacteremia following cardiac arrest and cardiopulmonary resuscitation. Intensive Care Med 14:575–577
Cerchiari EL, Safar P, Klein E, Diven W (1993) Visceral, hematologic and bacteriologic changes and neurologic outcome after cardiac arrest in dogs. The visceral post-resuscitation syndrome. Resuscitation 25:119–136
Gajic O, Festic E, Afessa B (2004) Infectious complications in survivors of cardiac arrest admitted to the medical intensive care unit. Resuscitation 60:65–69
Rello J, Valles J, Jubert P, Ferrer A, Domingo C, Mariscal D, Fontanals D, Artigas A (1995) Lower respiratory tract infections following cardiac arrest and cardiopulmonary resuscitation. Clin Infect Dis 21:310–314
Huang CH, Chen WJ, Ma MH, Chang WT, Lai CL, Lee YT (2002) Factors influencing the outcomes after in-hospital resuscitation in Taiwan. Resuscitation 53:265–270
Nakos G, Tsangaris H, Liokatis S, Kitsiouli E, Lekka ME (2003) Ventilator-associated pneumonia and atelectasis: evaluation thourgh bronchoalveolar lavage fluid analysis. Intensive Care Med 29:555–563
Dennesen P, Veerman E, van Nieuw Amerongen A, Jacobs J, Kessels A, van der Keybus P, Ramsay G, van der Ven A (2003) High levels of sulfated mucins in bronchoalveolar lavage fluid of ICU patients with ventilator-associated pneumonia. Intensive Care Med 29:715–719
Weinstein MP, Towns ML, Quartey SM, Mirrett S, Reimer LG, Parmigiani G, Reller LB (1997) The clinical significance of positive blood cultures in the 1990s: a prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin Infect Dis 24:584–602
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W, Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ (2002) Health care-associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med 137:791–797
Siegman-Igra Y, Fourer B, Orni-Wasserlauf R, Golan Y, Noy A, Schwartz D, Giladi M (2002) Reappraisal of community-acquired bacteremia: a proposal of a new classification for the spectrum of acquisition of bacteremia. Clin Infect Dis 34:1431–1439
Lark RL, Saint S, Chenoweth C, Zemencuk JK, Lipsky BA, Plorde JJ (2001) Four-year prospective evaluation of community-acquired bacteremia: epidemiology, microbiology, and patient outcome. Diagn Microbiol Infect Dis 41:15–22
The Hypothermia After Cardiac Arrest Study Group (2002) Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 346:549–556
Taylor MD, Napolitano LM (2004) Methicillin-resistant Staphylococcus aureus infections in vascular surgery: increasing prevalence. Surg Infect (Larchmt) 5:180–187
Saeed Abdulrahman I, Al-Mueilo SH, Bokhary HA, Ladipo GO, Al-Rubaish A (2002) A prospective study of hemodialysis access-related bacterial infections. J Infect Chemother 8:242–246
Ahmad K, Khan UF, Hafeez A (2004) Control of Burkholderia (Pseudomonas) bacteremia in the intensive care and paediatric units. J Coll Physicians Surg Pak 14:102–104
Ko PC, Ma MH, Yen ZS, Shih CL, Chen WJ, Lin FY (2004) Impact of community-wide deployment of biphasic waveform automated external defibrillators on out-of-hospital cardiac arrest in Taipei. Resuscitation 63:167–174
Nishiuchi T, Hiraide A, Hayashi Y, Uejima T, Morita H, Yukioka H, Shigemoto T, Ikeuchi H, Matsusaka M, Iwami T, Shinya H, Yokota J (2003) Incidence and survival rate of bystander-witnessed out-of-hospital cardiac arrest with cardiac etiology in Osaka, Japan: a population-based study according to the Utstein style. Resuscitation 59:329–335
Valenzuela TD, Roe DJ, Cretin S, Spaite DW, Larsen MP (1997) Estimating effectiveness of cardiac arrest intervention: a logistic regression survival model. Circulation 96:3308–3313
Herlitz J, Eek M, Engdahl J, Holmberg M, Holmberg S (2003) Factors at resuscitation and outcome among patients suffering from out of hospital cardiac arrest in relation to age. Resuscitation 58:309–317
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsai, MS., Chiang, WC., Lee, CC. et al. Infections in the survivors of out-of-hospital cardiac arrest in the first 7 days. Intensive Care Med 31, 621–626 (2005). https://doi.org/10.1007/s00134-005-2612-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2612-6