Summary
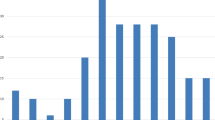
Treatment results in 65 patients with borrelial lymphocytoma (22 on the ear lobe and 43 on the breast), registered at the Department of Infectious Diseases, University Medical Centre Ljubljana, from January 1986 to March 1995, are presented. When lymphocytoma was the sole manifestation of Lyme borreliosis or associated with erythema migrans only patients were treated orally with doxycycline, phenoxymethylpenicillin or amoxicillin for 14 days, or azithromycin for 5 days (15, 19, six and 12 patients, respectively). When signs and symptoms of disseminated borrelial infection were present (seven patients) or clinically suspected (six patients) patients received ceftriaxone or penicillin G i.v. for 14 days. Lymphocytoma disappeared within a few weeks after the institution of treatment. The speed of regression depended on the duration of lymphocytoma before the institution of therapy. The number of patients was too low and pretreatment characteristics were too heterogeneous to enable a reliable comparison of the efficacy of different antibiotics. It appears that the effectiveness of doxycycline and azithromycin is comparable and that amoxicillin performs well, but some findings may indicate that phenoxymethylpenicillin is less effective than some newer antibiotics. The optimal agent, dosage and duration of therapy for borrelial lymphocytoma have not been determined.
Zusammenfassung
Die Behandlungsergebnisse von 65 Patienten mit Borrelien-Lymphozytom (22 am Ohr und 43 an der Brust), die in der Abteilung für Infektionskrankheiten der Universitätsklinik Ljubljana von Januar 1986 bis März 1995 registriert wurden, werden mitgeteilt. Wenn das Lymphozytom die einzige Manifestation der Lyme-Borreliose war oder mit einem Erythema migrans einherging, wurden die Patienten 14 Tage lang oral mit Doxycyclin, Phenoxymethylpenicillin oder Amoxicillin oder 5 Tage lang mit Azithromycin behandelt (15, 19, sechs und 12 Patienten in den entsprechenden Gruppen). Wenn die Zeichen einer generalisierten Borrelieninfektion vorhanden waren (sieben Patienten) oder ein entsprechender Verdacht bestand (sechs Patienten), wurden die Patienten 14 Tage lang mit Ceftriaxon oder Penicillin G i.v. behandelt. Das Lymphozytom verschwand innerhalb weniger Wochen nach Therapiebeginn. Die Geschwindigkeit der Rückbildung war davon bestimmt, wie lange das Lymphozytom vor Therapiebeginn schon bestanden hatte. Für einen zuverlässigen Vergleich der Wirksamkeit der verschiedenen Antibiotika-Therapien waren die Anzahl der Patienten zu klein und die prätherapeutischen Daten zu heterogen. Die Wirksamkeit von Doxycyclin und Azithromycin scheint vergleichbar gut zu sein; Amoxicillin ist offensichtlich ebenfalls wirksam. Einige Daten weisen darauf hin, daß Phenoxymethylpenicillin möglicherweise weniger wirksam ist als einige der neueren Antibiotika. Das optimale Antibiotikum, Dosierung und Behandlungsdauer des Borrelien-Lymphozytoms konnten noch nicht festgelegt werden.
Similar content being viewed by others
References
Hovmark, A., Asbrink, E., Weber, K., Kaudevitz, P. Borrelial lymphocytoma. In:Weber, K., Burgdorfer, W., Schierz, G. (eds.): Aspects of Lyme borreliosis. Springer-Verlag, Berlin, Heidelberg, New York 1993, pp. 122–130.
Strle, F., Pleterski-Rigler, D., Stanek, G., Pejovnik-Pustinek, A., Ružić, E., Cimperman, J. Solitary borrelial lymphocytoma: report of 36 cases. Infection 20 (1992) 201–206.
Asbrink, E., Hovmark, A., Olsson, L. Lymphadenosis benigna cutis solitaria — borrelial lymphocytoma in Sweden. Zbl. Bakt. (Suppl. 18) (1989) 156–163.
Asbrink, E., Hovmark, A. Cutaneous manifestations in IxodesborneBorrelia spirochetosis. Inter. J. Derm. 26 (1987) 215–223.
Asbrink, E., Hovmark, A. Early and late cutaneous manifestations in Ixodes-borne borreliosis (erythema migrans borreliosis, Lyme borreliosis). Ann. N.Y. Acad. Sci. 539 (1988) 4–15.
Preac-Mursic, V., Wilske, B., Schierz, G. EuropeanBorrelia burgdorferi isolated from humans and ticks. Culture conditions and antibiotic susceptibility. Zbl. Bakt. Hyg. A 263 (1986) 112–118.
Barbour, A. G. Isolation and cultivation of Lyme disease spirochetes. Yale J. Biol. Med. 57 (1984) 521–525.
Berger, B. W., Johnson, R. C., Kodner, C., Coleman, L. Cultivation ofBorrelia burgdorferi from erythema migrans and perilesional skin. J. Clin. Microbiol. 30 (1992) 359–361.
Steere, A. C., Hutchinson, G. J., Rahn, D. W. A., Sigal, L. H., Craft, J. E., DeSanna, E. T., Malawista, S. E. Treatment of the early manifestations of Lyme disease. Ann. Intern. Med. 99 (1983) 22–26.
Weber, K., Schierz, G., Wilske, B., Preac-Mursic, V. Das Lymphozytom — eine Borreliose? Z. Hautkr. 60 (1985) 1585–1598.
Hovmark, A., Asbrink, E., Olsson, I. The spirochetal etiology of lymphadenosis benigna cutis solitaria. Acta Derm. Venerol. (Stockholm) 66 (1986) 479–484.
Weber, K., Neubert, U., Thurmayr, R. Antibiotic therapy in early erythema migrans disease and related disorders. Zbl. Bakt. Hyg. (A) 263 (1986) 377–388.
Bianchi, G. Die Penicillinbehandlung der Lymphozytome. Dermatologica 100 (1950) 270–273.
Weber, K. Therapy of cutaneous manifestations. In:Weber, K., Burgdorfer, W., Schierz, G. (eds.): Aspects of Lyme borreliosis. Springer-Verlag, Berlin, Heidelberg, New York 1993, pp. 312–327.
Krbkova, L., Stanek, G.: Duration of antibiotic therapy of Lyme borreliosis in children's age. In: Program and Abstracts of the VIth International Conference on Lyme borreliosis, Bologna, Italy, 1994, PO53W.
Krbkova, L., Stanek, G.: Schedules for the therapy of Lyme borreliosis in children. Symposium on the therapy and prophylaxis for Lyme borreliosis. Portoroz, Slovenia, 1995, pp. 24.
Hercogova, J., Valesova, M., Meluzinova, E., Bojar, M., Janovska, D., Hulinska, D.: Erythema migrans: therapy in children and adults. Symposium on the therapy and prophylaxis for Lyme borreliosis. Portoroz, Slovenia, 1995, pp. 35.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Strle, F., Maraspin, V., Pleterski-Rigler, D. et al. Treatment of borrelial lymphocytoma. Infection 24, 80–84 (1996). https://doi.org/10.1007/BF01780665
Issue Date:
DOI: https://doi.org/10.1007/BF01780665