Abstract
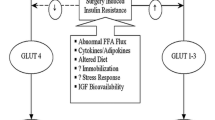
In the development and implementation of the enhanced recovery after surgery (ERAS) program, there has been the need to understand the mechanism and the factors that affect the recovery process. Most of the elements considered by the ERAS® Society to have an impact on recovery have a physiological basis, and the interaction between them characterizes the modulation of the stress response. For example, besides surgical incision, some of them such as pain, hemorrhage, immobilization, and quasi starvation have a synergistic effect. The activation of the sympathetic system and the inflammatory response associated with all these surgical elements characterize the surgical stress response, thus leading to a state of low insulin sensitivity, which represents the most important pathogenic factor modulating the perioperative outcome.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
Notes
- 1.
Please note: the infusion of a 100 ml bag of dextrose 5% (=5 g of glucose) almost doubles the amount of circulating glucose in a 70 kg nondiabetic patient (assuming a glycemia level of 5 mmol/L = 0.9 g/L and a blood volume of 77 ml/kg) [5].
References
Polderman JA, Van Velzen L, Wasmoeth LG, et al. Hyperglycemia and ambulatory surgery. Minerva Anestesiol. 2015;81(9):951–9.
Carli F, Galeone M, Gzodzic B, et al. Effect of laparoscopic colon resection on postoperative glucose utilization and protein sparing: an integrated analysis of glucose and protein metabolism during the fasted and fed States using stable isotopes. Arch Surg (Chicago, IL: 1960). 2005;140(6):593–7.
Eberhart LH, Graf J, Morin AM, et al. Randomised controlled trial of the effect of oral premedication with dexamethasone on hyperglycaemic response to abdominal hysterectomy. Eur J Anaesthesiol. 2011;28(3):195–201.
Hatzakorzian R, Bui H, Carvalho G, Shan WL, Sidhu S, Schricker T. Fasting blood glucose levels in patients presenting for elective surgery. Nutrition (Burbank, Los Angeles County, CA). 2011;27(3):298–301.
Schricker T, Lattermann R, Wykes L, Carli F. Effect of i.v. dextrose administration on glucose metabolism during surgery. JPEN J Parenter Enteral Nutr. 2004;28(3):149–53.
Rice MJ, Pitkin AD, Coursin DB. Review article: glucose measurement in the operating room: more complicated than it seems. Anesth Analg. 2010;110(4):1056–65.
Ghys T, Goedhuys W, Spincemaille K, Gorus F, Gerlo E. Plasma-equivalent glucose at the point-of-care: evaluation of Roche Accu-Chek Inform and Abbott Precision PCx glucose meters. Clin Chim Acta. 2007;386(1–2):63–8.
Karon BS, Griesmann L, Scott R, et al. Evaluation of the impact of hematocrit and other interference on the accuracy of hospital-based glucose meters. Diabetes Technol Ther. 2008;10(2):111–20.
Mitsios JV, Ashby LA, Haverstick DM, Bruns DE, Scott MG. Analytic evaluation of a new glucose meter system in 15 different critical care settings. J Diabetes Sci Technol. 2013;7(5):1282–7.
Karon BS, Donato LJ, Larsen CM, et al. Accuracy of capillary and arterial whole blood glucose measurements using a glucose meter in patients under general anesthesia in the operating room. Anesthesiology. 2017;127(3):466–74.
Shohat N, Muhsen K, Gilat R, Rondon AJ, Chen AF, Parvizi J. Inadequate glycemic control is associated with increased surgical site infection in total joint arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2018;33(7):2312–2321.e2313.
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978–82.
Furnary AP, Zerr KJ, Grunkemeier GL, Starr A. Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg. 1999;67(2):352–60; discussion 360–352.
Thomas MC, Mathew TH, Russ GR, Rao MM, Moran J. Early peri-operative glycaemic control and allograft rejection in patients with diabetes mellitus: a pilot study. Transplantation. 2001;72(7):1321–4.
Baird TA, Parsons MW, Phan T, et al. Persistent poststroke hyperglycemia is independently associated with infarct expansion and worse clinical outcome. Stroke. 2003;34(9):2208–14.
Stranders I, Diamant M, van Gelder RE, et al. Admission blood glucose level as risk indicator of death after myocardial infarction in patients with and without diabetes mellitus. Arch Intern Med. 2004;164(9):982–8.
Szczudlik A, Slowik A, Turaj W, et al. Transient hyperglycemia in ischemic stroke patients. J Neurol Sci. 2001;189(1-2):105–11.
Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125(5):1007–21.
Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D. Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg. 2013;257(1):8–14.
Ross-Huot MC, Laferriere A, Gi CM, Khorashadi M, Schricker T, Coderre TJ. Effects of glycemic regulation on chronic postischemia pain. Anesthesiology. 2011;115(3):614–25.
Hermanides J, Qeva E, Preckel B, Bilotta F. Perioperative hyperglycemia and neurocognitive outcome after surgery: a systematic review. Minerva Anestesiol. 2018;84(10):1178–88.
Krueger JJ, Brotschi B, Balmer C, Bernet V, Latal B. Postoperative hyperglycemia and 4-year neurodevelopmental outcome in children operated for congenital heart disease. J Pediatr. 2015;167(6):1253–1258.e1251.
Deane AM, Horowitz M. Dysglycaemia in the critically ill – significance and management. Diabetes Obes Metab. 2013;15(9):792–801.
Sim MA, Liu W, Chew STH, Ti LK. Wider perioperative glycemic fluctuations increase risk of postoperative atrial fibrillation and ICU length of stay. PLoS One. 2018;13(6):e0198533.
Halkos ME, Puskas JD, Lattouf OM, et al. Elevated preoperative hemoglobin A1c level is predictive of adverse events after coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2008;136(3):631–40.
Gustafsson UO, Thorell A, Soop M, Ljungqvist O, Nygren J. Haemoglobin A1c as a predictor of postoperative hyperglycaemia and complications after major colorectal surgery. Br J Surg. 2009;96(11):1358–64.
Noordzij PG, Boersma E, Schreiner F, et al. Increased preoperative glucose levels are associated with perioperative mortality in patients undergoing noncardiac, nonvascular surgery. Eur J Endocrinol. 2007;156(1):137–42.
Abdelmalak BB, Knittel J, Abdelmalak JB, et al. Preoperative blood glucose concentrations and postoperative outcomes after elective non-cardiac surgery: an observational study. Br J Anaesth. 2014;112(1):79–88.
Sato H, Carvalho G, Sato T, Lattermann R, Matsukawa T, Schricker T. The association of preoperative glycemic control, intraoperative insulin sensitivity, and outcomes after cardiac surgery. J Clin Endocrinol Metab. 2010;95(9):4338–44.
Yki-Jarvinen H, Utriainen T. Insulin-induced vasodilatation: physiology or pharmacology? Diabetologia. 1998;41(4):369–79.
Das UN. Is insulin an anti-inflammatory molecule? Nutrition (Burbank, Los Angeles County, CA). 2001;17(5):409–13.
Kahn CR. Insulin resistance, insulin insensitivity, and insulin unresponsiveness: a necessary distinction. Metabolism. 1978;27(12 Suppl 2):1893–902.
Thorell A, Nygren J, Ljungqvist O. Insulin resistance: a marker of surgical stress. Curr Opin Clin Nutr Metab Care. 1999;2(1):69–78.
Thorell A, Loftenius A, Andersson B, Ljungqvist O. Postoperative insulin resistance and circulating concentrations of stress hormones and cytokines. Clin Nutr (Edinburgh, Scotland). 1996;15(2):75–9.
Tsubo T, Kudo T, Matsuki A, Oyama T. Decreased glucose utilization during prolonged anaesthesia and surgery. Can J Anaesth/Journal canadien d’anesthesie. 1990;37(6):645–9.
Nygren J, Thorell A, Efendic S, Nair KS, Ljungqvist O. Site of insulin resistance after surgery: the contribution of hypocaloric nutrition and bed rest. Clin Sci (London, England: 1979). 1997;93(2):137–46.
Uchida I, Asoh T, Shirasaka C, Tsuji H. Effect of epidural analgesia on postoperative insulin resistance as evaluated by insulin clamp technique. Br J Surg. 1988;75(6):557–62.
Wang ZG, Wang Q, Wang WJ, Qin HL. Randomized clinical trial to compare the effects of preoperative oral carbohydrate versus placebo on insulin resistance after colorectal surgery. Br J Surg. 2010;97(3):317–27.
Bagry HS, Raghavendran S, Carli F. Metabolic syndrome and insulin resistance: perioperative considerations. Anesthesiology. 2008;108(3):506–23.
DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237(3):E214–23.
Nakadate Y, Sato H, Sato T, Codere-Maruyama T, Matsukawa T, Schricker T. Body mass index predicts insulin sensitivity during cardiac surgery: a prospective observational study. Can J Anaesth/Journal canadien d’anesthesie. 2018;65(5):551–9.
Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85(1):109–17.
Giannoudis PV, Dinopoulos H, Chalidis B, Hall GM. Surgical stress response. Injury. 2006;37 Suppl 5:S3–9.
Cuthbertson DP, Angeles Valero Zanuy MA, Leon Sanz ML. Post-shock metabolic response. 1942. Nutr Hosp. 2001;16(5):176–82; discussion 175–176.
Puthucheary ZA, Rawal J, McPhail M, et al. Acute skeletal muscle wasting in critical illness. JAMA. 2013;310(15):1591–600.
Biolo G, Fleming RY, Maggi SP, Nguyen TT, Herndon DN, Wolfe RR. Inverse regulation of protein turnover and amino acid transport in skeletal muscle of hypercatabolic patients. J Clin Endocrinol Metab. 2002;87(7):3378–84.
Schricker T, Meterissian S, Lattermann R, et al. Anticatabolic effects of avoiding preoperative fasting by intravenous hypocaloric nutrition: a randomized clinical trial. Ann Surg. 2008;248(6):1051–9.
Kinney JM, Elwyn DH. Protein metabolism and injury. Annu Rev Nutr. 1983;3:433–66.
Schricker T, Gougeon R, Eberhart L, et al. Type 2 diabetes mellitus and the catabolic response to surgery. Anesthesiology. 2005;102(2):320–6.
Donatelli F, Corbella D, Di Nicola M, et al. Preoperative insulin resistance and the impact of feeding on postoperative protein balance: a stable isotope study. J Clin Endocrinol Metab. 2011;96(11):E1789–97.
Herridge MS, Cheung AM, Tansey CM, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683–93.
Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–94.
Morais JA, Chevalier S, Gougeon R. Protein turnover and requirements in the healthy and frail elderly. J Nutr Health Aging. 2006;10(4):272–83.
Muhlbacher F, Kapadia CR, Colpoys MF, Smith RJ, Wilmore DW. Effects of glucocorticoids on glutamine metabolism in skeletal muscle. Am J Physiol. 1984;247(1 Pt 1):E75–83.
Lacey JM, Wilmore DW. Is glutamine a conditionally essential amino acid? Nutr Rev. 1990;48(8):297–309.
Hulshoff A, Schricker T, Elgendy H, Hatzakorzian R, Lattermann R. Albumin synthesis in surgical patients. Nutrition (Burbank, Los Angeles County, CA). 2013;29(5):703–7.
Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340(6):448–54.
Lang CH, Frost RA, Vary TC. Regulation of muscle protein synthesis during sepsis and inflammation. Am J Physiol Endocrinol Metab. 2007;293(2):E453–9.
Brower RG. Consequences of bed rest. Crit Care Med. 2009;37(10 Suppl):S422–8.
Meguid MM, Debonis D, Meguid V, Hill LR, Terz JJ. Complications of abdominal operations for malignant disease. Am J Surg. 1988;156(5):341–5.
Jagoe RT, Goodship TH, Gibson GJ. The influence of nutritional status on complications after operations for lung cancer. Ann Thorac Surg. 2001;71(3):936–43.
Von Meyenfeldt MF, Meijerink WJ, Rouflart MM, Builmaassen MT, Soeters PB. Perioperative nutritional support: a randomised clinical trial. Clin Nutr (Edinburgh, Scotland). 1992;11(4):180–6.
Bozzetti F, Gavazzi C, Miceli R, et al. Perioperative total parenteral nutrition in malnourished, gastrointestinal cancer patients: a randomized, clinical trial. JPEN J Parenter Enteral Nutr. 2000;24(1):7–14.
Veterans Affairs Total Parenteral Nutrition Cooperative Study Group. Perioperative total parenteral nutrition in surgical patients. N Engl J Med. 1991;325(8):525–32.
Shaw JH, Wolfe RR. Glucose and urea kinetics in patients with early and advanced gastrointestinal cancer: the response to glucose infusion, parenteral feeding, and surgical resection. Surgery. 1987;101(2):181–91.
Shaw JH. Influence of stress, depletion, and/or malignant disease on the responsiveness of surgical patients to total parenteral nutrition. Am J Clin Nutr. 1988;48(1):144–7.
Hasselager R, Gogenur I. Core muscle size assessed by perioperative abdominal CT scan is related to mortality, postoperative complications, and hospitalization after major abdominal surgery: a systematic review. Langenbecks Arch Surg. 2014;399(3):287–95.
Schricker T, Wykes L, Meterissian S, et al. The anabolic effect of perioperative nutrition depends on the patient’s catabolic state before surgery. Ann Surg. 2013;257(1):155–9.
Downs JH, Haffejee A. Nutritional assessment in the critically ill. Curr Opin Clin Nutr Metab Care. 1998;1(3):275–9.
Hoffer LJ, Bistrian BR. Appropriate protein provision in critical illness: a systematic and narrative review. Am J Clin Nutr. 2012;96(3):591–600.
Allison SP. Malnutrition, disease, and outcome. Nutrition (Burbank, Los Angeles County, CA). 2000;16(7–8):590–3.
Allison SP, Lobo DN, Stanga Z. The treatment of hypoalbuminaemia. Clin Nutr (Edinburgh, Scotland). 2001;20(3):275–9.
Matthews DE, Motil KJ, Rohrbaugh DK, Burke JF, Young VR, Bier DM. Measurement of leucine metabolism in man from a primed, continuous infusion of L-[1-3C]leucine. Am J Physiol. 1980;238(5):E473–9.
Prelack K, Dwyer J, Yu YM, Sheridan RL, Tompkins RG. Urinary urea nitrogen is imprecise as a predictor of protein balance in burned children. J Am Diet Assoc. 1997;97(5):489–95.
Berg A, Rooyackers O, Bellander BM, Wernerman J. Whole body protein kinetics during hypocaloric and normocaloric feeding in critically ill patients. Crit Care (London, England). 2013;17(4):R158.
Lattermann R, Carli F, Wykes L, Schricker T. Perioperative glucose infusion and the catabolic response to surgery: the effect of epidural block. Anesth Analg. 2003;96(2):555–62, table of contents.
Lattermann R, Carli F, Wykes L, Schricker T. Epidural blockade modifies perioperative glucose production without affecting protein catabolism. Anesthesiology. 2002;97(2):374–81.
Schricker T, Wykes L, Carli F. Epidural blockade improves substrate utilization after surgery. Am J Physiol Endocrinol Metab. 2000;279(3):E646–53.
Chandra RK. Nutrition, immunity, and infection: present knowledge and future directions. Lancet (London, England). 1983;1(8326 Pt 1):688–91.
Windsor JA, Hill GL. Weight loss with physiologic impairment. A basic indicator of surgical risk. Ann Surg. 1988;207(3):290–6.
Watters JM, Clancey SM, Moulton SB, Briere KM, Zhu JM. Impaired recovery of strength in older patients after major abdominal surgery. Ann Surg. 1993;218(3):380–90; discussion 390–383.
Christensen T, Bendix T, Kehlet H. Fatigue and cardiorespiratory function following abdominal surgery. Br J Surg. 1982;69(7):417–9.
Ljungqvist O. Modulating postoperative insulin resistance by preoperative carbohydrate loading. Best Pract Res Clin Anaesthesiol. 2009;23(4):401–9.
Hill GL, Douglas RG, Schroeder D. Metabolic basis for the management of patients undergoing major surgery. World J Surg. 1993;17(2):146–53.
Lopez-Hellin J, Baena-Fustegueras JA, Vidal M, Riera SS, Garcia-Arumi E. Perioperative nutrition prevents the early protein losses in patients submitted to gastrointestinal surgery. Clin Nutr (Edinburgh, Scotland). 2004;23(5):1001–8.
Andersen HK, Lewis SJ, Thomas S. Early enteral nutrition within 24h of colorectal surgery versus later commencement of feeding for postoperative complications. Cochrane Database Syst Rev. 2006;(4):Cd004080.
Martindale RG, McClave SA, Taylor B, Lawson CM. Perioperative nutrition: what is the current landscape? JPEN J Parenter Enteral Nutr. 2013;37(5 Suppl):5s–20s.
Blixt C, Ahlstedt C, Ljungqvist O, Isaksson B, Kalman S, Rooyackers O. The effect of perioperative glucose control on postoperative insulin resistance. Clin Nutr (Edinburgh, Scotland). 2012;31(5):676–81.
Kim TK, Yoon JR. Comparison of the neuroendocrine and inflammatory responses after laparoscopic and abdominal hysterectomy. Korean J Anesthesiol. 2010;59(4):265–9.
Carli F, Halliday D. Continuous epidural blockade arrests the postoperative decrease in muscle protein fractional synthetic rate in surgical patients. Anesthesiology. 1997;86(5):1033–40.
Lugli AK, Donatelli F, Schricker T, Wykes L, Carli F. Epidural analgesia enhances the postoperative anabolic effect of amino acids in diabetes mellitus type 2 patients undergoing colon surgery. Anesthesiology. 2008;108(6):1093–9.
Carli F, Webster J, Nandi P, MacDonald IA, Pearson J, Mehta R. Thermogenesis after surgery: effect of perioperative heat conservation and epidural anesthesia. Am J Physiol. 1992;263(3 Pt 1):E441–7.
Glover EI, Phillips SM, Oates BR, et al. Immobilization induces anabolic resistance in human myofibrillar protein synthesis with low and high dose amino acid infusion. J Physiol. 2008;586(24):6049–61.
Wall BT, Snijders T, Senden JM, et al. Disuse impairs the muscle protein synthetic response to protein ingestion in healthy men. J Clin Endocrinol Metab. 2013;98(12):4872–81.
Krogh-Madsen R, Thyfault JP, Broholm C, et al. A 2-wk reduction of ambulatory activity attenuates peripheral insulin sensitivity. J Appl Physiol (Bethesda, MD: 1985). 2010;108(5):1034–40.
Kortebein P, Symons TB, Ferrando A, et al. Functional impact of 10 days of bed rest in healthy older adults. J Gerontol A Biol Sci Med Sci. 2008;63(10):1076–81.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Schricker, T., Lattermann, R., Carli, F. (2020). Physiology and Pathophysiology of ERAS. In: Ljungqvist, O., Francis, N., Urman, R. (eds) Enhanced Recovery After Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-33443-7_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-33443-7_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-33442-0
Online ISBN: 978-3-030-33443-7
eBook Packages: MedicineMedicine (R0)