Abstract
Gynecology outpatient units are in charge of treating different gynecological diseases such as tumorous, cancer, urinary incontinence, gynecological pain, and abnormal discharge. On-time attention is thus needed to avoid severe complications, patient dissatisfaction, and elevated healthcare costs. There is then an urgent need for assessing whether the gynecology outpatient departments are cost-effective and what interventions are required for improving clinical outcomes. Despite this context, the studies directly concentrating on diagnosis and improvement of these departments are widely limited. To address these concerns, this paper aims to provide a Discrete-event Simulation (DES) modelling framework to help healthcare managers gain a better understanding of the gynecology outpatient services and evaluate improvement strategies. First, the patient journey through the gynecology outpatient service is mapped. To correctly represent the system uncertainty, collected data is then processed through input analysis. Third, the data is used to model and simulate the real gynecology outpatient unit. This model is later validated to determine whether it is statistically equivalent to the real system. After this, using performance metrics derived from the simulation model, the gynecology outpatient department is analyzed to identify potential improvements. We finally pretest potential interventions to define their viability during implementation. A case study of a mixed-patient type environment in a public gynecology outpatient unit is presented to verify the applicability of the proposed methodology. The results evidenced that appointment lead times could be efficiently reduced using this approach.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Gynecology outpatient units are responsible for treating many different and diverse conditions and chronic diseases such as such as cancers, urinary incontinence, gynecological pain, and abnormal discharge. Timely attention is thus needed to avoid severe complications, patient dissatisfaction, higher mortality, and increased healthcare costs. However, public healthcare systems are increasingly lacking in necessary resources and therefore need to manage scarce resources in an optimal manner. As such, there is an urgent need to monitor and evaluate the cost-effectiveness of gynecology outpatient departments as well as developing and assessing possible interventions which could alleviate such problems, with the aim of improving the efficiency of services as well as clinical outcomes.
With these considerations in mind, this paper aims to provide a Discrete-event Simulation (DES) modelling framework to help healthcare managers gain a better understanding of the gynecology outpatient services as well as facilitating the evaluation of improvement strategies. We initially focus on the entire patient pathway through the gynecology outpatient service and characterize the different phases of care, resource limitations, critical variables, and their interrelations. Following this, improvement strategies are identified and evaluated.
Despite the problems we have outlined, research directly concentrating on performance assessment and improvement of gynecology outpatient units has been severely limited [1]. In the current paper, we focus on developing a DES model for such units particularly in view of the fact that the animation features commonly found in simulation packages facilitate engagement with healthcare managers, thus enabling development of realistic and accurate models. Easy visualization of key relationships in the models is also an important aspect [2].
Such an approach has been used previously, to a limited extent, to help improve provision across a number of healthcare specialties. For example, a simulation model to characterize appointment-based hospitals facilities, with a particular focus on capacity deficiencies [3]; a similar approach was adopted by [4], who were concerned with improving appointment scheduling. In [5], the authors likewise focused on reducing patient waiting times and improving resource utilization. On a different tack, a simulation analysis was performed for reducing queues in a mixed-patient outpatient department [6]. In this case, two improvement scenarios were designed and assessed with regard to the simultaneous impact of operations, scheduling, resource allocation on patient waiting time, clinic overtime and resource utilization in general. As a result, an improvement proposal achieved a reduction of up to 70% in patient waiting times and 25% in physical space requirements. On a similar note, a framework using discrete-event simulation was provided to model stroke care and evaluate the impact of discharge queues and patient-centered care [7]. However, on a cautionary note, they also stressed that the availability of suitable data could prove to be a limitation on modeling healthcare services. Also, on a related theme to the current one, some previous work has been carried out using DES to improve Gynecology and Obstetrics departments with respect to reducing appointment lead times which are associated with poor patient satisfaction, variable and diverse healthcare services, and the development of long-term and severe complications with corresponding increases in fetal, infant and maternal mortality [8].
More generally, the current paper aims to define and evaluate novel improvement strategies through the use of discrete-event simulation for performance evaluation and improvement of Gynecology Outpatient Departments in the Public Sector. In particular, we evaluate three possible interventions: (i) establishing collaborative scenarios with similar departments, (ii) varying installed capacity and (iii) using local search algorithms to determine optimal schedules A case study of a mixed-patient type environment in a public gynecology outpatient unit is presented to validate the applicability of the proposed approach.
The remainder of this paper is organized as follows: In Sect. 2 the legal framework that motivates this study is shown whereas the proposed approach is explained in Sect. 3. In Sect. 4, a case study in an outpatient gynecology department from a Colombian maternal-child hospital is described. Ultimately, Sect. 5 presents the conclusions and future work.
2 The Legal Framework
The right to health has been recognized by the Colombian Institutional Court, in the XXI century, as an institutional, fundamental, autonomous, and irrevocable guarantee since it allows the full enjoyment of the other rights. In accordance with Statutory Law 1751 (2015), the right to health “includes the timely, efficacious and access to high-quality healthcare services for the preservation, improvement, and promotion of health” [9]. Given its connotation of mandatory essential public service, the government must manage, regulate and supervise its provision [10]. Additionally, due to its assistance-oriented nature of this right, the government must adopt public policies directed towards the expansion of coverage and the continuous improvement of service quality so that integral, effective and timely access can be granted [9].
In this sense, Law 100 (1993) and Law 1751 (2015) establish the principles of efficiency, quality, and opportunity as pillars determining healthcare as a substantial public service and fundamental right [9, 11]. Based on these laws, the Information System for Quality (ISQ) serves as a tool for monitoring the quality of service and assisting users in the selection of a healthcare provider [12]. Thereby, by means of the Resolution 256 (2016), the Ministry of Health and Social Protection enacted regulations on ISQ and established the gynecology appointment lead-time as an indicator for monitoring the quality of service provided to women. Such regulations apply to Department, District, and Municipal healthcare entities, among other members of this sector [13]. These considerations have motivated the design and evaluation of initiatives aiming at reducing the gynecology appointment lead time as those described within this paper.
3 Proposed Approach
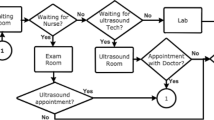
Step 1 “System Characterization”: To suitably model the outpatient gynecology department, it is required to identify their main components (sub-processes) and the associated process data (variables and parameters). This information is then consolidated in a flow diagram through which the modelers will be able to elicit the patient journey, detect interrelations and identify system constraints. The system details should be provided by health service managers, administrative staff, healthcare professionals, and other stakeholders involved in the outpatient unit. Such stakeholders should be highly committed to work closely to the modelers to ensure that the resulting simulation models are realistic and robust (Fig. 1).
Step 2 “Data Preprocessing”: To ensure the robustness of the simulation model, it is necessary to incorporate high-quality data that provide a good representation of the real-world system. The data referring to the process variables and parameters should be collected from reliable information sources linked to the functioning of the outpatient gynecology department under study. The acquisition of such data enables modelers to develop more informative and detailed models which is more beneficial for health service managers when creating multidimensional interventions. If these data are not properly preprocessed, some bias can be introduced into the simulation model. To tackle this problem, three statistical tests are needed. First, a runs test is performed to establish whether a specific variable follows a random behavior or is correlated with other input variables. A homogeneity analysis is later performed to classify data into groups based on their similarity. The Kolgomorov-Smirnov and Kruskal-Wallis tests can be used for underpinning this approach. If the data are not consistent with the homogeneity hypothesis, each group is categorized in accordance with a probability function; alternatively, one probability expression is sufficient to model the variable behavior. The goodness-of-fit is finally assessed through a Chi-square test to determine whether a statistical model provides a good fit for the data. After this, the corresponding parameters are estimated to be incorporated into the simulation model.
Step 3 “Development and Validation of a DES Model”: The problem under analysis requires the use of DES models in consideration of their capability to record individual entity (patients) experience, compare various improvement scenarios and analyze performance under restriction [14]. To create a DES application, the modeler should select a simulation package (i.e. Arena and Promodel) with animation features that facilitate user engagement. Then, the results derived from Steps 1 and 2 are fully incorporated into the DES model. Once finished, the modeler has to perform rigorous model transparency and validation in order to demonstrate its equivalence with the real outpatient gynecology department. To this end, it is first necessary to outline the performance metrics and simulation run length per replication. It is proposed to run the simulation for a warm-up period and then 10 times to calculate the final sample size (number of runs) that will be employed to verify whether the simulated model is significantly comparable to the real system. The validation is achieved by conducting a comparative test between means (if the data are normally distributed) or medians (if the data follow a non-normal probability function). If the p-value is higher than the alpha level (α = 0.05), the null hypothesis cannot be rejected and the model can be hence deemed a good illustration of the real department. Otherwise, the model should be thoroughly revised and corrected by the modelers and service health managers until achieving an acceptable level of equivalence with the system under analysis. Reliable DES applications provide valuable support for understanding the performance of outpatient gynecology departments and identifying sources of inefficiency in healthcare provision.
Step 4 “Diagnosis”: The use of DES for performance diagnosis of healthcare systems has gained increased prominence recently due to its capacity for measuring and storing system metrics per replication. Such metrics are an important output for conducting a deep analysis of the performance of outpatient gynecology departments and the detection of potential barriers [15, 16]. A crucial component of this step is the capability study which reveals how well the department satisfies the specifications established by the National Institute of Health. In this case, the key parameter is appointment lead-time (ALT) which is intended to be at 8 days as a maximum. In this step, capability indices like sigma level, Pp, Ppk, and DPMO are estimated to determine the gap between the process status and the desired performance.
Step 5 “Pretesting Improvement Strategies”: DES provides a means to pretest improvement scenarios in a safe and effective manner. This is highly beneficial for policymakers who often address the need for optimally allocating resources to improve outpatient gynecology care. Such scenarios should then secure positive change and oriented to a well-defined problem as stated in Step 4. In this context, it is essential to count on the participation of health service managers and clinicians who can develop more solid and realistic initiatives that take into account the multidimensional nature of healthcare. The scenarios are later simulated by the modeler and firstly run 10 times. Afterwards, the final sample size is obtained and the scenarios are simulated again in accordance with the established run length. The resulting ALT is statistically contrasted with the real behavior by implementing a test for differences between means (if the data is normally distributed) or medians (if the data follow a non-normal probability distribution). If the derived p-value is significant (<0.05), the scenario is suggested to be implemented in the real-world since it may reduce the ALT (Confidence level = 95%). Otherwise, it should be discarded.
4 An Illustrative Example: Modeling an Outpatient Gynecology Department from a Maternal-Child Hospital
4.1 System Characterization
A flow diagram was designed to give an overview of the patient journey within an outpatient gynecology department from a maternal-child hospital. In particular, three sub-processes (Scheduling, Billing, and Outpatient Gynecology Care) and three appointment types (First-time, control, and priority) were distinguished (refer to Fig. 2). Our model was supported by a 1-year dataset gleaned from the User Information System (UIS) and comprising all the gynecology appointments booked between 1 January and 31 December (n = 13001 appointments). In this period, 1766 (13.6%) requests were priority appointments, 5717 (43.9%) corresponded to first-time consultations and the rest (5518) were asked for control purposes. The patients are women between the ages of 16 and 43 years old.
The gynecology appointments are requested through the Scheduling unit where two assistants (AS1, AS2) serve in accordance with the work shifts WS1 (8:00–12:00; 14:00–17:00) and WS2 (8:00–13:00; 15:00–17:00) correspondingly. The appointments can be also scheduled by a phone call with the aid of the contact center agent AS3 who operates according to WS1. The appointments are booked based on the availability of gynecologists, consultation rooms and consultation type. Nonetheless, this process is influenced by the late arrival of gynecologists, cancellations of medical agenda (every three weeks) and equipment damage. These failures augment the complexity of the scheduling process and new methodologies can be hence required for responding to the context here presented. The patients are invited to arrive at the hospital 2 h prior to the consultation time in order to obtain the consultation order and invoice from one of the agents (BA1, BA2) who work in the Billing department conformed to WS1 and WS2 correspondingly. The patients then stay at the waiting room up to the consultation time. In Outpatient Gynecology Care, there are six gynecologists who work in accordance with the agenda presented in Table 1.
Ultimately, seven process variables were outlined: (i) time between arrivals for first-time appointments, (ii) time between arrivals for control appointments, (iii) time between arrivals for priority consultation (iv) service time in Scheduling division (in-person attention), (v) service time in Scheduling division (call center), (vi) service time in Billing division, and (vii) service time in outpatient gynecology care.
4.2 Data Preprocessing
Once the data collection referring to the seven process variables is finished, a runs test was undertaken to evaluate the independence hypothesis. The outcomes are described in Table 2. The evidence revealed that all the variables were concluded to be independent since the p-values were significant at an error level of 0.05. After validating this assumption, an Analysis of Variance (ANOVA) was performed for each variable in order to distinguish the sub-groups of data (refer to Table 3). It was concluded that the time between arrivals should be modeled independently considering the consultation type (p-value = 0). In turn, service time in the Scheduling division, service time in the Billing division, and service time in outpatient gynecology care were found to be homogeneous since the derived p-values provided enough evidence to accept the homogeneity assumption.
Once the independence and homogeneity analysis are complete, the modelers have to specify the probability expressions that will represent each process variable from Table 3. To this aim, Goodness-of-fit tests were conducted at an error level of 0.05. For example, the Kolmogorov-Smirnov test (KS = 0.162, p-value > 0.15) provided good support for the Triangular assumption of time between arrivals (control appointments). The final results of these tests are detailed in Table 4.
4.3 Development and Validation of a DES Model
A DES model was developed to provide a virtual representation of the outpatient gynecology department under analysis (refer to Fig. 3). To ensure the accuracy and robustness of the DES outcomes, we ran the simulation for 372 days with 9 h per shift-day. After the initial exploration, we found that 100 days can be assumed as a warm-up period. In addition, a pre-sample of 10 runs was undertaken to estimate the required sample size for properly representing the ALT variability. In this project, 35 replications were found to be statistically sufficient for explaining department performance. Next, the ALT values, recorded by Arena 14.5 ® in each replication, were processed to validate the model (Ho: μ = 7.76 days/consultation|Ha: μ ≠ 7.76 days/consultation). To this aim, a 1-sample t-test (C.L. = 0.95) was conducted using Minitab 17 ® software. The resulting p-value (0.86) and t-statistic (−0.18) revealed that the virtual model is statistically compared with the real outpatient gynecology department. Therefore, it can be further used for the diagnosis and evaluation of improvement scenarios.
4.4 Diagnosis
After verifying the suitability of the DES model, the next stage was to determine how capable the outpatient gynecology department is to meet the target set by the National Health Institution (U.S.L. = 8 days/consultation). The capability study revealed that the average ALT is 7.7 days/consultation with a shape of 7.91 days/consultation and a scale of 0.96 days/consultation. Additionally, it was found that 404597 out of 1 million of consultations will have an ALT > 8 days. Complementary to these indices, the Ppu (0.06), Ppk (0.06) and sigma process level (1.74) argue that the performance is poor and then demands profound changes. These results were presented to the health service managers in order to design potential interventions that tackle the problem here described (Fig. 4).
4.5 Pretesting Improvement Scenarios
Discrete-event simulation allows modelers to evaluate changes in outpatient care delivery before implementation in a safe and effective manner [17,18,19]. This is useful to avoid the investment of restricted resources on low effective strategies. However, only a few studies have worked on evaluating the impact of such scenarios through the use of DES [20]. Motivated by the need of addressing this issue and the extended ALT, the researchers and health service managers decided to pretest three alternatives: (i) Establish collaborative scenarios with similar departments, (ii) Varying the installed capacity and (iii) Reassignment of specific outpatient care tasks. These scenarios were then modeled and run with the aid of Arena 14.5 ® software. The impact of each change was statistically studied through Mann-Whitney tests (C.L. = 0.95).
Strategy #1 proposes that an external provider shares 1 gynecologist in case of demand peaks. The Mann-Whitney test revealed that the ALT provided in this scenario is lower than the current performance (refer to Fig. 5a) compared to the real waiting time (p-value = 0; W = 980). On a different tack, Strategy #2 (refer to Fig. 5b) recommends increasing the installed capacity by 8 h. The results proved that ALT can be substantially minimized (p-value = 0; W = 980). Lately, the strategy #3 (refer to Fig. 5c) proposes to assign some activities of outpatient gynecology care to nurse practitioners (i.e. blood pressure measurement, calculate the patient’s weight, fill out the paperwork). In this scenario, the ALT was found to be significantly lower with respect to the standard and current process behavior (p-value = 0; W = 980).
5 Conclusions and Future Work
In this article, we have verified the applicability of discrete-event simulation to reduce the appointment lead-time in outpatient gynecology departments. In particular, the capability analysis foresees that 40.46% of the consultations requests in this unit will have an ALT higher than the maximum allowable limit. To address this problem, three strategies were modeled and simulated with the assistance of health service managers and specialized software. In this project, all the strategies were concluded to be effective since they minimize the appointment lead-time indicator. Through these interventions, severe complications, patient dissatisfaction, higher mortality, and increased healthcare costs can be substantially avoided.
On a different tack, with the use of DES, health service managers and policymakers are able to evaluate the impact of potential improvement strategies before implementation. This is valuable to determine their viability, minimize errors during execution, allocate scant resources better and avoid extra charges. To this end, it is relevant to provide high-quality data and work closely with the modelers so that high accuracy and robustness of these models can be granted.
Our study contributes to the small reported evidence regarding the use of DES models for pretesting improvement scenarios and support viability evaluation. Nevertheless, we aim in future work to incorporate economic evaluation and develop cost-effectiveness indicators that offer a wider overview of the implementation in terms of investment returns and performance improvement. We also plan to consider interactions with other healthcare units (i.e. emergency departments, intensive care units, hospitalization divisions) to underpin integrated planning and resource management within maternal hospitals.
References
Zhang, X.: Application of discrete event simulation in health care: a systematic review. BMC Health Serv. Res. 18(1), 687 (2018)
Brailsford, S.C., Harper, P.R., Patel, B., Pitt, M.: An analysis of the academic literature on simulation and modelling in health care. J. Simul. 3(3), 130–140 (2009)
Elkhuizen, S.G., Das, S.F., Bakker, P.J.M., Hontelez, J.A.M.: Using computer simulation to reduce access time for outpatient departments. BMJ Qual. Saf. 16(5), 382–386 (2007)
Harper, P.R., Gamlin, H.M.: Reduced outpatient waiting times with improved appointment scheduling: a simulation modelling approach. OR Spectr. 25(2), 207–222 (2003)
Santibáñez, P., Chow, V.S., French, J., Puterman, M.L., Tyldesley, S.: Reducing patient wait times and improving resource utilization at British Columbia Cancer Agency’s ambulatory care unit through simulation. Health Care Manag. Sci. 12(4), 392 (2009)
Wijewickrama, A.K.A.: Simulation analysis for reducing queues in mixed-patients’ outpatient department. Int. J. Simul. Model. 5(2), 56–68 (2006)
Gillespie, J., McClean, S., Garg, L., Barton, M., Scotney, B., Fullerton, K.: A multi-phase DES modelling framework for patient-centred care. J. Oper. Res. Soc. 67(10), 1239–1249 (2016)
Ortiz, M.A., McClean, S., Nugent, C.D., Castillo, A.: Reducing appointment lead-time in an outpatient department of gynecology and obstetrics through discrete-event simulation: a case study. In: García, C.R., Caballero-Gil, P., Burmester, M., Quesada-Arencibia, A. (eds.) UCAmI 2016. LNCS, vol. 10069, pp. 274–285. Springer, Cham (2016). https://doi.org/10.1007/978-3-319-48746-5_28
Congreso de la República de Colombia: Law 1751 (2015). Por medio de la cual se regula el derecho fundamental a la salud y se dictan otras disposiciones, 16 February 2015. http://www.secretariasenado.gov.co/senado/basedoc/ley_1751_2015.html#26
Constitución Política de Colombia (1991). http://www.secretariasenado.gov.co/index.php/constitucion-politica
Congreso de la República de Colombia: Law 100 (1993). Por la cual se crea el sistema de seguridad social integral y se dictan otras disposiciones, 23 December 1993. http://www.secretariasenado.gov.co/senado/basedoc/ley_0100_1993.html#T%C3%8DTULO%20PRELIMIN
Ministerio de Salud y Protección Social: Decree 780 (2016). Por medio del cual se expide el Decreto Único Reglamentario del Sector Salud y Protección Social, 6 May 2016. https://www.minsalud.gov.co/Normatividad_Nuevo/Decreto%200780%20de%202016.pdf
Ministerio de Salud y Protección Social: Resolution 256 (2016). Por la cual se dictan disposiciones en relación con el Sistema de Información para la Calidad y se establecen los indicadores para el monitoreo de la calidad en salud, 5 February 2016. http://www.acreditacionensalud.org.co/sua/Documents/Resoluci%C3%B3n%200256%20de%20201620SinfCalidad.pdf
Karnon, J., Stahl, J., Brennan, A., Caro, J.J., Mar, J., Möller, J.: Modeling using discrete event simulation: a report of the ISPOR-SMDM modeling good research practices task force–4. Med. Decis. Making 32(5), 701–711 (2012)
Izquierdo, N.V., Lezama, O.B.P., Dorta, R.G., Viloria, A., Deras, I., Hernández-Fernández, L.: Fuzzy logic applied to the performance evaluation. Honduran coffee sector case. In: Tan, Y., Shi, Y., Tang, Q. (eds.) ICSI 2018. LNCS, vol. 10942, pp. 164–173. Springer, Cham (2018). https://doi.org/10.1007/978-3-319-93818-9_16
Günal, M.M., Pidd, M.: Discrete event simulation for performance modelling in health care: a review of the literature. J. Simul. 4(1), 42–51 (2010)
Ortiz Barrios, M., Felizzola Jiménez, H., Nieto Isaza, S.: Comparative analysis between ANP and ANP- DEMATEL for six sigma project selection process in a healthcare provider. In: Pecchia, L., Chen, L.L., Nugent, C., Bravo, J. (eds.) IWAAL 2014. LNCS, vol. 8868, pp. 413–416. Springer, Cham (2014). https://doi.org/10.1007/978-3-319-13105-4_62
Ortiz, M.A., López-Meza, P.: Using computer simulation to improve patient flow at an outpatient internal medicine department. In: García, C.R., Caballero-Gil, P., Burmester, M., Quesada-Arencibia, A. (eds.) UCAmI 2016. LNCS, vol. 10069, pp. 294–299. Springer, Cham (2016). https://doi.org/10.1007/978-3-319-48746-5_30
Ortíz-Barrios, M., Jimenez-Delgado, G., De Avila-Villalobos, J.: A computer simulation approach to reduce appointment lead-time in outpatient perinatology departments: a case study in a maternal-child hospital. In: Siuly, S., et al. (eds.) HIS 2017. LNCS, vol. 10594, pp. 32–39. Springer, Cham (2017). https://doi.org/10.1007/978-3-319-69182-4_4
Mohiuddin, S., et al.: Patient flow within UK emergency departments: a systematic review of the use of computer simulation modelling methods. BMJ Open 7(5), e015007 (2017)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this paper
Cite this paper
Ortiz-Barrios, M., Lopez-Meza, P., McClean, S., Polifroni-Avendaño, G. (2019). Discrete-Event Simulation for Performance Evaluation and Improvement of Gynecology Outpatient Departments: A Case Study in the Public Sector. In: Duffy, V. (eds) Digital Human Modeling and Applications in Health, Safety, Ergonomics and Risk Management. Healthcare Applications. HCII 2019. Lecture Notes in Computer Science(), vol 11582. Springer, Cham. https://doi.org/10.1007/978-3-030-22219-2_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-22219-2_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-22218-5
Online ISBN: 978-3-030-22219-2
eBook Packages: Computer ScienceComputer Science (R0)