Abstract
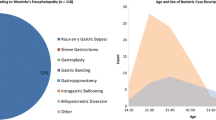
Wernicke encephalopathy (WE) is an acute neurological disorder classically characterized by ataxia, ophthalmoplegia, and altered mental status. This is caused by thiamine deficiency and is usually seen in malnourished populations. However, with the advent and rise of bariatric surgery in the last 50 years, WE has become an increasingly recognized and potentially deadly complication. Here, we review the populations at risk, clinical presentation, and the incidence of WE in the bariatric surgery population from 1985 to 2023. While the predominant procedure shifts throughout the years, the overall incidence of WE per 100,000 cases for the following procedures are sleeve gastrectomy (1.06), gastric band (1.16), RYGB (4.29), and biliopancreatic diversion with duodenal switch (8.92). Thus, early intervention and post-operative supplementation is recommended to prevent WE.




Similar content being viewed by others
References
Shields M, Carroll MD, Ogden CL. Adult obesity prevalence in Canada and the United States. NCHS Data Brief. 2011;56:1–8.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery and endoluminal procedures: IFSO Worldwide Survey 2014. Obes Surg. 2017;27(9):2279–89. https://doi.org/10.1007/s11695-017-2666-x.
Rindi G. Thiamin absorption by small intestine. Acta Vitaminol Enzymol. 1984;6(1):47–55.
Chaves LC, Faintuch J, Kahwage S, et al. A cluster of polyneuropathy and Wernicke-Korsakoff syndrome in a bariatric unit. Obes Surg. 2002;12(3):328–34. https://doi.org/10.1381/096089202321088093.
Dudeja PK, Tyagi S, Kavilaveettil RJ, et al. Mechanism of thiamine uptake by human jejunal brush-border membrane vesicles. Am J Physiol Cell Physiol. 2001;281(3):C786–92. https://doi.org/10.1152/ajpcell.2001.281.3.C786.
Oudman E, Wijnia JW, van Dam M, et al. Preventing Wernicke encephalopathy after bariatric surgery. Obes Surg. 2018;28(7):2060–8. https://doi.org/10.1007/s11695-018-3262-4.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Thomson AD, Cook CCH, Guerrini I, et al. Review Wernicke’s encephalopathy revisited translation of the case history section of the original manuscript by Carl Wernicke ‘Lehrbuch der Gehirnkrankheiten fur Aerzte and Studirende’ (1881) with a commentary. Alcohol Alcohol. 2008;43(2):174–9. https://doi.org/10.1093/alcalc/agm144.
Sechi G, Serra A. Wernicke’s encephalopathy: new clinical settings and recent advances in diagnosis and management. Lancet Neurol. 2007;6(5):442–55. https://doi.org/10.1016/S1474-4422(07)70104-7.
Oudman E, Wijnia JW, Oey MJ, et al. Preventing Wernicke’s encephalopathy in anorexia nervosa: a systematic review. Psychiatry Clin Neurosci. 2018;72(10):774–9. https://doi.org/10.1111/pcn.12735.
Lonsdale D. A review of the biochemistry, metabolism and clinical benefits of thiamin(e) and its derivatives. Evid Based Complement Alternat Med. 2006;3(1):49–59. https://doi.org/10.1093/ecam/nek009.
Ota Y, Capizzano AA, Moritani T, et al. Comprehensive review of Wernicke encephalopathy: pathophysiology, clinical symptoms and imaging findings. Jpn J Radiol. 2020;38(9):809–20. https://doi.org/10.1007/s11604-020-00989-3.
Osiezagha K, Ali S, Freeman C, et al. Thiamine deficiency and delirium. Innov Clin Neurosci. 2013;10(4):26–32.
Mehanna H, Nankivell PC, Moledina J, et al. Refeeding syndrome–awareness, prevention and management. Head Neck Oncol. 2009;1:4. https://doi.org/10.1186/1758-3284-1-4.
Arnold D. British India and the “beriberi problem”, 1798–1942. Med Hist. 2010;54(3):295–314. https://doi.org/10.1017/s0025727300004622.
Wiley KD, Gupta M. Vitamin B1 (Thiamine) Deficiency. StatPearls; 2023.
Chandrakumar A, Bhardwaj A, Jong GWt. Review of thiamine deficiency disorders: Wernicke encephalopathy and Korsakoff psychosis. J Basic Clin Physiol Pharmacol. 2019;30(2):153–62. https://doi.org/10.1515/jbcpp-2018-0075.
Berhoumi AE, Laoudiyi D, Doumiri M, et al. [Gayet-Wernicke encephalopathy with normal thiamine level: a case report]. Pan Afr Med J. 2021;38:16. Encephalopathie de Gayet-Wernicke avec taux de thiamine normale: a propos d’un cas. https://doi.org/10.11604/pamj.2021.38.16.25888.
Donnino MW, Vega J, Miller J, et al. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50(6):715–21. https://doi.org/10.1016/j.annemergmed.2007.02.007.
Galvin R, Bråthen G, Ivashynka A, et al. EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol. 2010;17(12):1408–18. https://doi.org/10.1111/j.1468-1331.2010.03153.x.
Lange J, Königsrainer A. Malnutrition as a complication of bariatric surgery - a clear and present danger? Visc Med. 2019;35(5):305–11. https://doi.org/10.1159/000503040.
Isasa Rodriguez L, Fernandez Lopez MDC, Maldonado Castro GF. Acute neuropathy after gastric reduction surgery. Med Clin (Barc). 2019;153(4):e17-e18. Neuropatia relacionada con la cirugia bariatrica. https://doi.org/10.1016/j.medcli.2018.11.009.
Simonik I, Bonaventura J, Tvaruzek J, et al. Wernicke s encephalopathy as rare complication after sleeve gastrectomy. Rozhl Chir. 2019 98(2):66–70. Wernickeova encefalopatie jako vzacna komplikace po sleeve gastrectomy.
Patel S, Gomez V. A case of ascending sensory neuropathy due to acute onset thiamine deficiency after intragastric balloon placement. Obes Surg. 2019;29(10):3404–5. https://doi.org/10.1007/s11695-019-03967-5.
Benichou A, Buscot M, Boyer S, et al. [Gayet-Wernicke’s encephalopathy after bariatric surgery]. Presse Med. 2019;48(9):982–985. Encephalopathie de Gayet-Wernicke apres chirurgie bariatrique. https://doi.org/10.1016/j.lpm.2019.08.003.
Casalnuovo CA, Vera Cedeno CA, Refi CA, et al. Wernicke encephalopathy after sleeve gastrectomy. Obes Surg. 2020;30(12):5129–30. https://doi.org/10.1007/s11695-020-04778-9.
Dihn D, Chien K, Ma L. Case report: Wernicke encephalopathy following Roux-en-Y gastric bypass. Am Fam Physician. 2020;102(4):197–8.
Kandlakunta H, Gurala D, Philipose J, et al. A Case of Wernicke’s encephalopathy in a pregnant woman with a history of sleeve gastrectomy. Cureus. 2020;12(8):e9970. https://doi.org/10.7759/cureus.9970.
Lal D, Farrell MC, Krishnamurthy M. Wernicke’s encephalopathy mimicking multiple sclerosis in a young female patient post-bariatric gastric sleeve surgery. J Commun Hosp Intern Med Perspect. 2021;11(5):658–61. https://doi.org/10.1080/20009666.2021.1949792.
Kalbi D, Al Sbihi A, Parekh H, et al. Wernicke encephalopathy after Roux-en-Y gastric bypass in a young patient. BMJ Case Rep. 2022;15(3). https://doi.org/10.1136/bcr-2021-247710.
Gross A, Yu AT, Lara-Reyna J, et al. Duodenal adenocarcinoma in the setting of bariatric surgery: a perfect storm for Wernicke’s encephalopathy. Cureus. 2023;15(1):e33765. https://doi.org/10.7759/cureus.33765.
Young MT, Phelan MJ, Nguyen NT. A decade analysis of trends and outcomes of male vs female patients who underwent bariatric surgery. J Am College Surg. 2016;222(3):226–31. https://doi.org/10.1016/j.jamcollsurg.2015.11.033.
Berger ER, Huffman KM, Fraker T, et al. Prevalence and risk factors for bariatric surgery readmissions: findings from 130,007 admissions in the metabolic and bariatric surgery accreditation and quality improvement program. Ann Surg. 2018;267(1):122–31. https://doi.org/10.1097/SLA.0000000000002079.
Rios-Diaz AJ, Metcalfe D, Devin CL, et al. Six-month readmissions after bariatric surgery: results of a nationwide analysis. Surgery. 2019;166(5):926–33. https://doi.org/10.1016/j.surg.2019.06.003.
Manzo G, De Gennaro A, Cozzolino A, et al. MR imaging findings in alcoholic and nonalcoholic acute Wernicke’s encephalopathy: a review. BioMed Res Int. 2014;2014:503596. https://doi.org/10.1155/2014/503596.
Thomson AD, Guerrini I, Marshall EJ. The evolution and treatment of Korsakoff’s syndrome: out of sight, out of mind? Neuropsychol Rev. 2012;22(2):81–92. https://doi.org/10.1007/s11065-012-9196-z.
Wilson RB. Pathophysiology, prevention, and treatment of beriberi after gastric surgery. Nutr Rev. 2020;78(12):1015–29. https://doi.org/10.1093/nutrit/nuaa004.
Schabelman E, Kuo D. Glucose before thiamine for Wernicke encephalopathy: a literature review. J Emerg Med. 2012;42(4):488–94. https://doi.org/10.1016/j.jemermed.2011.05.076.
Latt N, Dore G. Thiamine in the treatment of Wernicke encephalopathy in patients with alcohol use disorders. Intern Med J. 2014;44(9):911–5. https://doi.org/10.1111/imj.12522.
Pacei F, Iaccarino L, Bugiardini E, et al. Wernicke’s encephalopathy, refeeding syndrome and wet beriberi after laparoscopic sleeve gastrectomy: the importance of thiamine evaluation. Eur J Clin Nutr. 2020;74(4):659–62. https://doi.org/10.1038/s41430-020-0583-x.
Silk Z, Jones L, Heath D. Refeeding syndrome: an important complication after bariatric surgery. Surg Obes Relat Dis. 2011;7(5):e21–3. https://doi.org/10.1016/j.soard.2010.02.047.
Parrott J, Frank L, Rabena R, et al. American society for metabolic and bariatric surgery integrated health nutritional guidelines for the surgical weight loss patient 2016 update: Micronutrients. Surg Obes Relat Dis. 2017;13(5):727–41. https://doi.org/10.1016/j.soard.2016.12.018.
Kerns JC, Arundel C, Chawla LS. Thiamin deficiency in people with obesity. Adv Nutr. 2015;6(2):147–53. https://doi.org/10.3945/an.114.007526.
Nath A, Tran T, Shope TR, et al. Prevalence of clinical thiamine deficiency in individuals with medically complicated obesity. Nutr Res. 2017;37:29–36. https://doi.org/10.1016/j.nutres.2016.11.012.
Pácal L, Kuricová K, Kaňková K. Evidence for altered thiamine metabolism in diabetes: is there a potential to oppose gluco- and lipotoxicity by rational supplementation? World J Diabetes. 2014;5(3):288–95. https://doi.org/10.4239/wjd.v5.i3.288.
Tang L, Alsulaim HA, Canner JK, et al. Prevalence and predictors of postoperative thiamine deficiency after vertical sleeve gastrectomy. Surg Obes Relat Dis. 2018;14(7):943–50. https://doi.org/10.1016/j.soard.2018.03.024.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Eighteen percent already have thiamine deficiency, and surgery increases risk for developing WE.
• WE should be on the differential in patients with neurologic symptoms or vomiting.
• Post-operative supplementation of thiamine is recommended to prevent WE development.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yu, A.T., Gross, A., Park, K. et al. Wernicke Encephalopathy After Bariatric Surgery: a Literature Review. OBES SURG 33, 3621–3627 (2023). https://doi.org/10.1007/s11695-023-06840-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06840-8