Abstract
Background and Aim
Elderly patients are frequently affected by gallstone-related disease. Current guidelines support cholecystectomy after a first acute biliary complication. In the aging, these recommendations are irregularly followed.
Methods
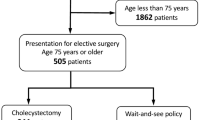
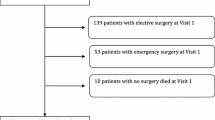
We analyzed data from patients 65 or older admitted between June 30, 2004 and June 30, 2013 with a diagnosis of acute pancreatitis, cholangitis, or cholecystitis. Diagnosis and severity assessment were defined according to current guidelines. Harms, mortality, and cholecystectomy rates were evaluated. Baseline factors independently predicting cholecystectomy were identified.
Results
A total of 491 patients were included. The median age was 78.8 years, and 51.7 % were women. Acute cholecystitis was present in 51.7 %, acute pancreatitis in 36.5 %, and acute cholangitis in 11.8 %. Cholecystectomy was performed in 47.1 %. Age, myocardial infarct, dementia, diabetes, nonmetastatic tumor, and severe liver disease were risk factors for not undergoing surgery. Complications related to hospital stay appeared in 33 % of patients. Surgery, cholecystostomy, and ERCP presented harms in 21–25 %. Overall mortality rate was 5.4 %: 10.4 % in acute cholangitis, 6.8 % in acute cholecystitis, and 2.2 % in acute pancreatitis. Mild cases presented a 1.3 % mortality, while 28.6 % of severe cases died. After discharge, 24.7 % of patients presented a new biliary complication, 9.7 % of them severe. Relapse was more frequent in patients managed without invasive procedures, 42.3 % than in cholecystectomy patients, 9.9 % (p < 0.001) and than in ERCP patients, 19.4 % (p = 0.01).
Conclusions
Cholecystectomy should be recommended to elderly patients after a first acute biliary complication. If not previously performed, ERCP should be offered as an alternative when surgery is contraindicated or refused.


Similar content being viewed by others
References
Khang KU, Wargo JA. Gallstone disease in the elderly. In: Rosenthal RA, Zenilman ME, Katlic MR, eds. Principles and practice of geriatric surgery. Berlin: Springer; 2001:690–710.
Gracie WA, Ransohoff DF. The natural history of silent gallstones: the innocent gallstone is not a myth. N Engl J Med. 1982;307:798–800.
McSherry CK, Ferstenberg H, Calhoun WF, Lahman E, Virshup M. The natural history of diagnosed gallstone disease in symptomatic and asymptomatic patients. Ann Surg. 1985;202:59–63.
Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–1187.
Rosing DK, De Virgilio C, Nguyen AT, El Masry M, Kaji AH, Stabile BE. Cholangitis: analysis of admission prognostic indicators and outcomes. Am Surg. 2007;73:949–954.
Tenner S, Baillie J, DeWitt J, Vege SS. American College of Gastroenterology. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–1415.
Yamashita Y, Takada T, Strasberg SM, et al. TG13 surgical management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:89–96.
Siegel JH, Kasmin FE. Biliary tract diseases in the elderly: management and outcomes. Gut. 1997;41:433–435.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296.
Banks PA, Bollen TL, Dervenis C, et al. Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111.
Yokoe M, Takada T, Strasberg SM, et al. TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2013;20:35–46.
Kiriyama S, Takada T, Strasberg SM, et al. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2013;20:24–34.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
Talukdar R, Clemens M, Vege SS. Moderately severe acute pancreatitis: prospective validation of this new subgroup of acute pancreatitis. Pancreas. 2012;41:306–309.
Kimura Y, Takada T, Strasberg SM, et al. TG13 current terminology, etiology, and epidemiology of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:8–23.
Trust MD, Sheffield KM, Boyd CA, et al. Gallstone pancreatitis in older patients: Are we operating enough? Surgery. 2011;150:515–525.
Riall TS, Zhang D, Townsend CM Jr, Kuo YF, Goodwin JS. Failure to perform cholecystectomy for acute cholecystitis in elderly patients is associated with increased morbidity, mortality, and cost. J Am Coll Surg. 2010;210:668–677.
Aranaz-Andrés JM, Aibar-Remón C, Vitaller-Burillo J, et al. Impact and preventability of adverse events in Spanish public hospitals: results of the Spanish National Study of Adverse Events (ENEAS). Int J Qual Health Care. 2009;21:408–414.
Aranaz-Andrés JM, Ruiz-López P, Aibar-Remón C, et al. Adverse events in general and digestive surgery departments in Spanish hospitals. Cir Esp. 2007;82:268–277.
Júdez Legaristi D, Aibar Remón C, Ortega Maján MT, Aguilella Diago V, Aranaz Andrés JM, Gutiérrez Cía I. Incidence of adverse events in a general surgery unit. Cir Esp. 2009;86:79–86.
Parry G, Cline A, Goldmann D. Deciphering harm measurement. JAMA. 2012;307:2155–2156.
Classen DC, Resar R, Griffin F, et al. “Global trigger tool” shows that adverse events in hospitals may be ten times greater than previously measured. Health Aff. 2011;30:581–589.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Adverse events and harms definitions:
Thromboembolic disease
Deep vein thrombosis confirmed with Doppler ultrasound or pulmonary embolism confirmed with computer tomography, gammagraphy, or cardiac ultrasound.
Acute kidney injury
Accepted if serum creatinine rises abruptly from baseline levels by 0.5 mg/dl or increases by 50 % or more.
Decompensation of chronic disease
Decompensation of previously known heart failure, kidney failure, chronic obstructive pulmonary disease, or hematological disease needing specific therapy, different from the patient’s usual treatment.
Delirium
Accepted if suggestive symptoms (acute, fluctuating change in mental status, altered level of consciousness, disorganized thinking) were recorded and specific pharmacological treatment or physical restraints were prescribed.
Nosocomial infection
Development of infection at least 3 days after admission; accepted if a positive urine or blood culture was present, a positive C difficile toxin assay and diarrhea were present or respiratory symptoms with a newly developed infiltrate on the chest X ray appeared.
Other complications
Newly diagnosed problems or diseases stated as secondary to the hospital stay or to the pharmacological treatments prescribed during hospital stay.
Post-ERCP pancreatitis
Condition presenting the following criteria: (1) new or worsened abdominal pain, (2) new or prolongation of hospitalization for at least 2 days, and (3) serum amylase or lipase three times or more the upper normal limit, measured 24 h after the procedure.
ERCP-related digestive bleeding
Decrease of at least 1 g/dl in hemoglobin value after ERCP and hematemesis, melena, or endoscopic demonstration of papillary bleeding or bleeding stigmata.
Perforation
Abdominal pain and radiological or surgical proof of a hollow viscus perforation.
Acute biliary infection
Development of new signs and symptoms fulfilling the 2013 Tokyo guidelines criteria for the diagnosis of acute cholangitis or acute cholecystitis.
Other complications related to the ERCP
Problems arising after the procedure and stated as secondary to the procedure itself (including sedation).
Cholecystostomy-related bleeding
Decrease of at least 1 g/dl in hemoglobin value after cholecystostomy and overt superficial bleeding, passage of melena, radiological documentation of hemoperitoneum, radiological, or endoscopic proof of hemobilia.
Biliary leak
Radiological or surgical proof of passage of bile to the peritoneum
Hollow viscus perforation
Abdominal pain and radiological or surgical proof of a hollow viscus perforation following a cholecystostomy.
Drainage tube dislocation
Involuntary removal or dislocation of the drainage tube, abandoning its intravesicular location.
Pneumothorax
Abnormal collection of air in the pleural space appearing after cholecystostomy.
Sepsis
Development of sepsis criteria (or worsening of condition to severe sepsis or septic shock if sepsis criteria were present previous to cholecystostomy) after the procedure.
Other cholecystostomy-related complications
Problems arising after the procedure and stated as secondary to the procedure itself (including sedation).
Surgery-related nosocomial infection
Development of infection at least 3 days after admission, accepted if a positive urine or blood culture was present, a positive C difficile toxin assay and diarrhea were present or respiratory symptoms with a newly developed infiltrate on the chest X ray appeared after cholecystectomy.
Surgical wound infection
Development of local signs of infection and/or a positive culture of the wound exudate.
Surgery-related thromboembolic disease
Deep vein thrombosis confirmed with Doppler ultrasound or pulmonary embolism confirmed with computer tomography, gammagraphy, or cardiac ultrasound appearing after cholecystectomy.
Ileus
Abdominal distention accompanied by nausea, constipation, and an abnormal bowel abdominal auscultation without an obstructive cause.
Bile duct injury
Endoscopic or radiological demonstration of a biliary leak or stenosis after cholecystectomy.
Other surgery-related complications
Problems arising after the surgical procedure and stated as secondary to the procedure itself (including sedation).
About this article
Cite this article
García-Alonso, F.J., de Lucas Gallego, M., Bonillo Cambrodón, D. et al. Gallstone-Related Disease in the Elderly: Is There Room for Improvement?. Dig Dis Sci 60, 1770–1777 (2015). https://doi.org/10.1007/s10620-014-3497-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3497-4