Abstract
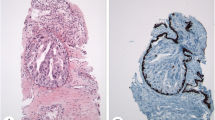
Buschke-Löwenstein tumor (BLT) is a rare sexually transmitted disease, mostly described in clinical literature as case reports or small series. Here, we investigated the clinicopathologic features of BLT in a total of 38 cases retrieved from multiple academic institutions. The average age was 47.6 ± 12.8 (mean ± SD) years old at diagnosis. The male to female ratio was 4.4:1. Common presenting symptoms were pain/discomfort, bleeding, mass lesion, and discharge. It was frequently linked to smoking and positive human immunodeficiency virus status. The tumor size and thickness were 8.5 ± 6.6 cm and 1.5 ± 1.3 cm, respectively. Histologically, 19 (50%) cases had an invasive squamous cell carcinoma component and were associated with high-risk human papillomavirus infection. There was no lymphovascular or perineural invasion, or nodal metastasis at initial diagnosis. BLTs with invasion had higher frequency of dyskeratosis, neutrophilic microabscesses, and abnormal mitoses, but lower frequency of pushing border compared with BLTs without invasion. All patients underwent wide excision, and some also received chemoradiation therapy. After a median follow-up of 23 months (range 1–207), the recurrence rate was 23.7% and disease-specific mortality was 2.6%. In summary, we presented the largest case series of BLT to date to characterize its unique clinicopathologic features. Our study indicated that certain histologic features such as dyskeratosis, neutrophilic microabscess, and abnormal mitosis in the non-invasive portion may be important clues on lesional biopsy to predict the presence of underlying invasive carcinoma.


Similar content being viewed by others
References
Erkek E, Basar H, Bozdogan O et al (2009) Giant condyloma acuminata of Buschke–Lowenstein: successful treatment with a combination of surgicalexcision, oral acitretin and topical imiquimod. Clin Exp Dermatol 34:366–368
Steffen C (2006) The men behind the eponym – Abraham Buschke and LudwigLowenstein: giant condyloma (Buschke–Loewenstein). Am J Dermatopathol 28:526–536
Trombetta LJ, Place RJ (2001) Giant condyloma acuminatum of the anorectum: trends in epidemiology and management: report of a case and review of the literature. Dis Colon Rectum 44:1878–1886
Chu QD, Vezeridis MP, Libbey NP, Wanebo HJ (1994) Giant condyloma acuminatum (Buschke–Lowenstein tumor) of the anorectal and perianal regions. Analysis of 42 cases. Dis Colon Rectum 37:950–957
Creasman C, Haas PA, Fox TA et al (1989) Malignant transformation of anorectal giant condyloma acuminatum (Buschke-Loewenstein tumor). Dis Colon Rectum 32:481–487
Boshart M, zur Hausen H (1986) Human papillomaviruses in Buschke–Lowensteintumors: physical state of the DNA and identification of a tandem duplication in the noncoding region of a human papillomavirus 6 subtype. J Virol 58: 963–966.
Rubben A, Beaudenon S, Favre M et al (1992) Rearrangements of the upstream regulatory region of human papillomavirustype 6 can be found in both Buschke–Lowenstein tumours and in condylomataacuminata. J Gen Virol 73:3147–3153
Gissmann L, de Villiers EM, zur Hausen H (1982) Analysis of human genital warts (condylomata acuminata) and other genital tumors for human papillomavirus type 6 DNA. Int J Cancer 29: 143–146.
Haycox CL, Kuypers J, Krieger JN (1999) Role of human papillomavirus typing in diagnosis and clinical decision making for a giant verrucous genital lesion. Urology 53:627–630
Yang C, Liu S, Wang Z, Yang S (2013) Buschke-Löwenstein tumor in an old woman: cryotherapy and holmium laser treatment. Arch Gynecol Obstet 288:221–223
Geusau A, Heinz-Peer G, Volc-Platzer B, Stingl G, Kirnbauer R (2000) Regression of deeply infiltrating giant condyloma (Buschke–Lowenstein tumor) following long-term intralesional interferon alfa therapy. Arch Dermatol 136:707–710
Ilkay AK, Chodak GW, Vogelsang NJ et al (1993) Buschke-Loewenstein tumor: therapeutic options including systemic chemotherapy. Urology 42:599–601
Heinzerling LM, Kempf W, Kamarashev J, Hafner J, Nestle FO (2003) Treatment of verrucous carcinoma with imiquimod and CO2 laser ablation. Dermatology 207:119–122
Gholam P, Enk A, Hartschuh W (2009) Successful surgical management of giant condyloma acuminatum (Buschke-Löwenstein tumor) in the genitoanal region: a case report and evaluation of current therapies. Dermatology 218:56–59
Zidar N, Langner C, Odar K, Hošnjak L, Kamarádová K, Daum O, Pollheimer MJ, Košorok P, Poljak M (2017) Anal verrucous carcinoma is not related to infection with human papillomaviruses and should be distinguished from giant condyloma (Buschke-Löwenstein tumour). Histopathology 70:938–945
Tytherleigh MG, Birtle AJ, Cohen CE, Glynne-Jones R, Livingstone J, Gilbert J (2006) Combined surgery and chemoradiation as a treatment for the Buschke-Lowenstein tumour. Surgeon 4:378–383
Nascimento AF, Granter SR, Cviko A, Yuan L, Hecht JL, Crum CP (2004) Vulvar acanthosis with altered differentiation: a precursor to verrucous carcinoma? Am J Surg Pathol 28:638–643
Del Pino M, Bleeker MCG, Quint WG et al (2012) Comprehensive analysis of human papillomavirus prevalence and the potential role of low-risk types in verrucous carcinoma. Mod Pathol 25:1354–1363
Patel KR, Chernock RD, Zhang TR et al (2013) Verrucous carcinomas of the head and neck, including those with associated squamous cell carcinoma, lack transcriptionally active high-risk human papillomavirus. Hum Pathol 44:2385–2392
Odar K, Kocjan BJ, Hošnjak L, Gale N, Poljak M, Zidar N (2014) Verrucous carcinoma of the head and neck – not a human papillomavirus-related tumour? J Cell Mol Med 18:635–645
Tauber M, Monsel G, Bonnecarrère L et al (2014) Unresectable perineal cuniculatum carcinoma: partial remission using systemic isotretinoin and interferon-α2a therapy. Acta Derm Venereol 94:721–722
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Contributions
DZ and XL (Xiuli Liu) contributed to the design and implementation of the study, to the analysis of the results, and to the writing of the manuscript. RG, MF, KU, HL, DA, DK, MZ, JL, MW, XZ, LA, and JL contributed to the retrieval of the cases and interpretation of the results. All authors provided critical feedback and helped shape the research, analysis, and manuscript. XL (Xiaoyan Liao) contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
The study was approved by Institutional Review Board of each participating institution.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, D., Gonzalez, R.S., Feely, M. et al. Clinicopathologic features of Buschke-Löwenstein tumor: a multi-institutional analysis of 38 cases . Virchows Arch 476, 543–550 (2020). https://doi.org/10.1007/s00428-019-02680-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-019-02680-z