Abstract
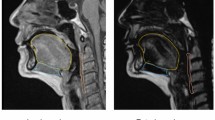
Muscle aging such as sarcopenia adversely affects motor activities. However, few studies have elucidated the aging physiological mechanism of tongue concerted with the changes muscle composition. The present study aimed to examine the tongue composition changes to detect the effect of tongue fat mass on tongue pressure and swallowing function with aging. Twenty community-dwelling elderly without head and neck cancer, stroke, or neuromuscular disease and 20 healthy young were included. Tongue volume, tongue fat mass, tongue lean muscle mass, and tongue fat percentage were evaluated with 3D magnetic resonance imaging (MRI) and Dixon MRI. Tongue pressure was also measured. Swallowing function among elderly individuals was assessed via videofluorography, which was evaluated using the penetration–aspiration scale (PAS) and normalized residue ratio scale (NRRS). Tongue fat mass and tongue fat percentage significantly increased with aging. The tongue fat percentage of elderly participants was 20%, which was two times greater than that of young participants. No significant difference was observed in tongue volume and tongue lean muscle mass. A significantly negative correlation was observed between tongue fat mass and tongue fat percentage as well as tongue pressure. Conversely, tongue volume was not significantly correlated with tongue pressure. Tongue muscle composition exhibited no effect in the PAS and NRRS. Increase of fat mass is a major change in tongue composition with aging, which is associated with low tongue pressure. Thus, attention must be paid not only to tongue quantity but also to the quality of tongue muscles.





Similar content being viewed by others
References
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, Jang HC, Kang L, Kim M, Kim S, Kojima T, Kuzuya M, Lee JSW, Lee SY, Lee WJ, Lee Y, Liang CK, Lim JY, Lim WS, Peng LN, Sugimoto K, Tanaka T, Won CW, Yamada M, Zhang T, Akishita M, Arai H, Asian Working Group for Sarcopenia. Asian Working Group for Sarcopenia: 2019 Consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21:300–307.e2. https://doi.org/10.1016/j.jamda.2019.12.012.
Akima H, Yoshiko A, Tomita A, Ando R, Saito A, Ogawa M, Kondo S, Tanaka NI. Relationship between quadriceps echo intensity and functional and morphological characteristics in older men and women. Arch Gerontol Geriatr. 2017;70:105–11. https://doi.org/10.1016/j.archger.2017.01.014.
Marcus RL, Addison O, Dibble LE, Foreman KB, Morrell G, Lastayo P. Intramuscular adipose tissue, sarcopenia, and mobility function in older individuals. J Aging Res. 2012;2012:629637. https://doi.org/10.1155/2012/629637.
Tuttle LJ, Sinacore DR, Mueller MJ. Intermuscular adipose tissue is muscle specific and associated with poor functional performance. J Aging Res. 2012;2012:172957. https://doi.org/10.1155/2012/172957.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M, Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2, Writing Group for the European. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–311. https://doi.org/10.1093/ageing/afy169.
Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53:1483–9. https://doi.org/10.1111/j.1532-5415.2005.53467.x.
Namasivayam AM, Steele CM, Keller H. The effect of tongue strength on meal consumption in long term care. Clin Nutr. 2016;35:1078–83. https://doi.org/10.1016/j.clnu.2015.08.001.
Buehring B, Hind J, Fidler E, Krueger D, Binkley N, Robbins J. Tongue strength is associated with jumping mechanography performance and handgrip strength but not with classic functional tests in older adults. J Am Geriatr Soc. 2013;61:418–22. https://doi.org/10.1111/jgs.12124.
Butler SG, Stuart A, Leng X, Wilhelm E, Rees C, Williamson J, Kritchevsky SB. The relationship of aspiration status with tongue and handgrip strength in healthy older adults. J Gerontol A Biol Sci Med Sci. 2011;66:452–8. https://doi.org/10.1093/gerona/glq234.
Maeda K, Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia. 2015;30:80–7. https://doi.org/10.1007/s00455-014-9577-y.
Robbins J, Levine R, Wood J, Roecker EB, Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol A Biol Sci Med Sci. 1995;50:M257–M262262. https://doi.org/10.1093/gerona/50a.5.m257.
Ono T, Kumakura I, Arimoto M, Hori K, Dong J, Iwata H, Nokubi T, Tsuga K, Akagawa Y. Influence of bite force and tongue pressure on oro-pharyngeal residue in the elderly. Gerodontology. 2007;24:143–50. https://doi.org/10.1111/j.1741-2358.2007.00172.x.
Todd JT, Lintzenich CR, Butler SG. Isometric and swallowing tongue strength in healthy adults. Laryngoscope. 2013;123:2469–73. https://doi.org/10.1002/lary.23852.
Tamura F, Kikutani T, Tohara T, Yoshida M, Yaegaki K. Tongue thickness relates to nutritional status in the elderly. Dysphagia. 2012;27:556–61. https://doi.org/10.1007/s00455-012-9407-z.
Tamura F, Kikutani T, Furuya H, Okayama H, Takahashi N. A study of tongue thickness in elderly people in Japan. Med Res Arch. 2017;5:1–14.
Butler SG, Lintzenich CR, Leng X, Stuart A, Feng X, Carr JJ, Kritchevsky SB. Tongue adiposity and strength in healthy older adults. Laryngoscope. 2012;122:1600–4. https://doi.org/10.1002/lary.23290.
Ogawa N, Mori T, Fujishima I, Wakabayashi H, Itoda M, Kunieda K, Shigematsu T, Nishioka S, Tohara H, Yamada M, Ogawa S. Ultrasonography to measure swallowing muscle mass and quality in older patients with sarcopenic dysphagia. J Am Med Dir Assoc. 2018;19:516–22. https://doi.org/10.1016/j.jamda.2017.11.007.
Humbert IA, Reeder SB, Porcaro EJ, Kays SA, Brittain JH, Robbins J. Simultaneous estimation of tongue volume and fat fraction using IDEAL-FSE. J Magn Reson Imaging. 2008. https://doi.org/10.1002/jmri.21431.
Grimm A, Meyer H, Nickel MD, Nittka M, Raithel E, Chaudry O, Friedberger A, Uder M, Kemmler W, Engelke K, Quick HH. Repeatability of Dixon magnetic resonance imaging and magnetic resonance spectroscopy for quantitative muscle fat assessments in the thigh. J Cachexia Sarcopenia Muscle. 2018;9:1093–100. https://doi.org/10.1002/jcsm.12343.
Kovanlikaya A, Guclu C, Desai C, Becerra R, Gilsanz V. Fat quantification using three-point Dixon technique: in vitro validation. Acad Radiol. 2005;12:636–9. https://doi.org/10.1016/j.acra.2005.01.019.
Yang YX, Chong MS, Tay L, Yew S, Yeo A, Tan CH. Automated assessment of thigh composition using machine learning for Dixon magnetic resonance images. Magma. 2016;29:723–31. https://doi.org/10.1007/s10334-016-0547-2.
Eichner K. Renewed examination of the group classification of partially edentulous arches by Eichner and application advices for studies on morbidity statistics. Stomatol DDR. 1990;40:321–5.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8. https://doi.org/10.1007/BF00417897.
Pearson WG Jr, Molfenter SM, Smith ZM, Steele CM. Image-based measurement of post-swallow residue: the normalized residue ratio scale. Dysphagia. 2013;28:167–77. https://doi.org/10.1007/s00455-012-9426-9.
Sakayori T, Maki Y, Hirata S, Okada M, Ishii T. Evaluation of a Japanese “Prevention of long-term care” project for the improvement in oral function in the high-risk elderly. Geriatr Gerontol Int. 2013;13:451–7. https://doi.org/10.1111/j.1447-0594.2012.00930.x.
Kubota T, Mishima H, Hanada M, Minami I, Kojima Y. Paralytic dysphagia in cerebrovascular disorder—screening tests and their clinical application. Sogo Rehabil. 1982;10:271–6.
Osawa A, Maeshima S, Tanahashi N. Food and liquid swallowing difficulty in stroke patients: a study based on the findings of food tests, a modified water swallowing test and videofluoroscopic examination of swallowing. The Jpn J Rehabil Med. 2012;49:838–45. https://doi.org/10.2490/jjrmc.49.838.
Leys C, Schumann S. A nonparametric method to analyze interactions: the adjusted rank transform test. J Exp Soc ol. 2010;46:684–8. https://doi.org/10.1016/j.jesp.2010.02.007.
Addison O, Marcus RL, Lastayo PC, Ryan AS. Intermuscular fat: a review of the consequences and causes. Int J Endocrinol. 2014;2014:309570. https://doi.org/10.1155/2014/309570.
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, Simonsick EM, Tylavsky FA, Visser M, Newman AB. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61:1059–64. https://doi.org/10.1093/gerona/61.10.1059.
St-Jean-Pelletier F, Pion CH, Leduc-Gaudet JP, Sgarioto N, Zovile I, Barbat-Artigas S, Reynaud O, Alkaterji F, Lemieux FC, Grenon A, Gaudreau P, Hepple RT, Chevalier S, Belanger M, Morais JA, Aubertin-Leheudre M, Gouspillou G. The impact of ageing, physical activity, and pre-frailty on skeletal muscle phenotype, mitochondrial content, and intramyocellular lipids in men. J Cachexia Sarcopenia Muscle. 2017;8:213–28. https://doi.org/10.1002/jcsm.12139.
Hamrick MW, McGee-Lawrence ME, Frechette DM. Fatty infiltration of skeletal muscle: mechanisms and comparisons with bone marrow adiposity. Front Endocrinol (Lausanne). 2016;7:69. https://doi.org/10.3389/fendo.2016.00069.
Essén-Gustavsson B, Karlsson A, Lundström K, Enfält AC. Intramuscular fat and muscle fibre lipid contents in halothane-gene-free pigs fed high or low protein diets and its relation to meat quality. Meat Sci. 1994;38:269–77. https://doi.org/10.1016/0309-1740(94)90116-3.
Sanders I, Mu L, Amirali A, Su H, Sobotka S. The human tongue slows down to speak: muscle fibers of the human tongue. Anat Rec (Hoboken). 2013;296:1615–27. https://doi.org/10.1002/ar.22755.
Acknowledgements
This study was partly supported by the Japan Society for the Promotion of Science (KAKENHI [17K11927]).
Author information
Authors and Affiliations
Contributions
Y.N, T.Y, K.H, Y.N, and K.D contributed to conceptualization and data curation. Y.N contributed to the evaluation of tongue strength and whole-body sarcopenia. T.K contributed to the analysis of tongue MRI. T.K, Y.H, K.A, and R.I contributed to MRI data collection. K.H and Y.N contributed to the evaluation of occlusal contact. T.Y, N.K, and Y.U contributed to the evaluation of VFSS. All authors contributed to the writing of the original draft, review, and editing. K.D contributed to the final approval of the article.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakao, Y., Yamashita, T., Honda, K. et al. Association Among Age-Related Tongue Muscle Abnormality, Tongue Pressure, and Presbyphagia: A 3D MRI Study. Dysphagia 36, 483–491 (2021). https://doi.org/10.1007/s00455-020-10165-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-020-10165-4