Published online Jan 10, 2016. doi: 10.4253/wjge.v8.i1.13
Peer-review started: July 30, 2015
First decision: September 14, 2015
Revised: September 25, 2015
Accepted: November 10, 2015
Article in press: November 11, 2015
Published online: January 10, 2016
With advances in endoscopic technologies, endoscopic clips have been used widely and successfully in the treatment of various types of oesophageal perforations, anastomosis leakages and fistulas. Our aim was to summarize the experience with two types of clips: The through-the-scope (TTS) clip and the over-the-scope clip (OTSC). We summarized the results of oesophageal perforation closure with endoscopic clips. We processed the data from 38 articles and 127 patients using PubMed search. Based on evidence thus far, it can be stated that both clips can be used in the treatment of early (< 24 h), iatrogenic, spontaneous oesophageal perforations in the case of limited injury or contamination. TTS clips are efficacious in the treatment of 10 mm lesions, while bigger (< 20 mm) lesions can be treated successfully with OTSC clips, whose effectiveness is similar to that of surgical treatment. However, the clinical success rate is significantly lower in the case of fistulas and in the treatment of anastomosis insufficiency. Tough prospective randomized multicentre trials, which produce the largest amount of evidence, are still missing. Based on experience so far, endoscopic clips represent a possible therapeutic alternative to surgery in the treatment of oesophageal perforations under well-defined conditions.
Core tip: With advances in endoscopic technologies, endoscopic clips have been used successfully in the treatment of various types of oesophageal perforations, anastomosis leakages and fistulas. We summarized the results of oesophageal perforation closure with endoscopic clips [the through-the-scope (TTS) clip and the over-the-scope clip (OTSC)]. We processed the data from 38 articles and 127 patients using PubMed search. Based on the evidence, TTS clips are efficacious in the treatment of 10 mm lesions, while bigger (< 20 mm) lesions can be treated successfully with OTSC clips. Based on experience so far, endoscopic clips represent a possible therapeutic alternative to surgery in the treatment of oesophageal perforations under well-defined conditions.
- Citation: Lázár G, Paszt A, Mán E. Role of endoscopic clipping in the treatment of oesophageal perforations. World J Gastrointest Endosc 2016; 8(1): 13-22
- URL: https://www.wjgnet.com/1948-5190/full/v8/i1/13.htm
- DOI: https://dx.doi.org/10.4253/wjge.v8.i1.13
Despite remarkable advances in surgery and intensive care, oesophageal perforation is still a life-threatening condition[1,2]. It is iatrogenic (caused by a device) in a majority of cases; perforation caused by a foreign body or trauma and spontaneous perforation are less frequent. Several well-known factors influence its course: location and cause of perforation, time from diagnosis until care, co-morbidities of the oesophagus, general condition of the patient and selected treatment[3,4]. In addition to oesophageal perforation, suture insufficiency of the oesophagus and other oesophageal fistulas also pose serious therapeutic challenges nowadays.
With the development of endoscopic technology during the last two decades, endoscopic clips and self-expanding stents have been used successfully and ever more widely in the treatment of oesophageal perforations/fistulas of various origins[5,6]. Oesophageal injury was first closed endoscopically with the placement of clips in 1995; the injury had occurred as a consequence of pneumatic dilatation in a patient with achalasia[7]. Since then, this method has been used for oesophageal perforations of various aetiologies, including Boerhaave syndrome[8-11]. To date, the method has been successful, especially in the treatment of small (< 2 cm) injuries. The following review article describes indications of endoscopy and endoscopic clips in the treatment of oesophageal perforation.
Various causes of perforation or rupture of the oesophagus are well-known: iatrogenic, foreign body, postemetic (spontaneous, Boerhaave syndrome) trauma, tumour and surrounding inflammation. Iatrogenic injuries are still the most common cause; the second most common is spontaneous oesophageal rupture. These two types represent more than two-thirds of the perforations based on a number of publications from different countries[12,13]. Suture insufficiency in the oesophagus (oesophageal/gastric resections and other sutures) and fistulas of various aetiologies fall into a separate group. In recent decades, the appearance and more widespread use of new therapeutic endoscopic methods have significantly increased the incidence of iatrogenic oesophageal perforations. It can be well determined which endoscopic interventions confer increased risk of perforation: (1) dilatation of the oesophagus (balloon/bougie); (2) endoscopic resections [endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD)]; and (3) removal of a foreign body. Dilatation of the oesophagus is almost as old as endoscopy; however, this method is still not without risks. The risk of perforation is greatest in the case of balloon dilatation (especially due to achalasia), with an approximate 2% overall cumulative rate, which can be reduced if endoscopic guidance is provided and if a balloon with a small (30 mm) diameter is used at the beginning of the intervention[14-16]. The risk of perforation in the dilatation treatment of peptic and other benign strictures is significantly lower with the use of a guide wire and a bougie (0.18%); however, in the case of malignant strictures, the risk of injury is increased again (0.48%)[17]. In the case of endoscopic resections (EMR and ESD), the risk of perforation is similar to that of balloon dilatation (2%-3%)[10,18].
A bidirectional chest X-ray is usually taken in addition to an oesophagogram with water-soluble contrast material to confirm perforation. The oesophagogram is the most common test procedure, but there are a number of false negative results (10%)[19]. Nowadays, abdominal and thoracic CT examinations are also routine[20]. The sensitivity of the CT examination is especially important in detecting a small amount of mediastinal/pleural air and/or fluid[21,22]. If the examination is combined with an oesophagogram, the exact location of extravasation can be determined more precisely. An endoscopic examination[23] may likewise be helpful in the diagnosis. Endoscopy is not only important in setting up the diagnosis, but also in confirming previously unknown accompanying co-morbidities of the oesophagus (such as tumour and stricture), which may significantly modify the treatment strategy. Endoscopy also offers an immediate treatment option (if the conditions are suitable), and it may also be helpful intraoperatively during surgical intervention (in checking whether the sutures are intact, in inserting a nasogastric/jejunal probe, etc.)[23]. The diagnosis of a perforation is especially important in the case of an endoscopic intervention (EMS, ESD, balloon dilatation, etc.), which also determines therapy and prognosis[24].
Essential elements in the treatment of oesophageal perforation include resolving the source of the infection, operative or non-operative closure of the defect, and thoracic and mediastinal debridement. Important parts of therapy are controlling sepsis, intensive monitoring, targeted antibiotic/antimycotic treatment, fluid therapy and strengthening the immune system of the body with enteral nutrition.
Several obvious factors determine treatment strategy and prognosis: (1) time of the diagnosis (delay); (2) localization of the perforation; (3) severity and size of the perforation; (4) presence of septic complications, physiologic reserves of the patient and existing co-morbidity of the oesophagus; and (5) the experience of the professionals providing care.
Primary closure of the oesophagus is successful in more than 90% of cases if the defect is closed within 24 h and there were no co-morbidities in the oesophagus (tumour, stricture, etc.)[25,26]. In this phase, tissues are not oedematic and are easy to suture/close; in addition, there is no active bacterial infection in the thoracic cavity and/or mediastinum. If the perforation occurred more than 24 h beforehand, the prognosis is significantly reduced due to rapidly developing septic complications and less successful surgical/conservative treatment[12,27].
It is well-known that thoracic transmural injuries of the oesophagus have the worst prognosis due to rapidly developing mediastinitis and sepsis, followed by injury of the abdominal segment, while perforation in the cervical segment has the best prognosis.
Intramural injuries usually respond well to conservative treatment. Transmural and transpleural injuries represent the worst defects. Treatment strategy is also essentially influenced by the size of the defect. These factors are especially important in using the endoscopic technique (see below).
General stress tolerance of the patient, existing co-morbidities and severe septic condition are known to worsen the prognosis[12,27]. Existing co-morbidities of the oesophagus are especially important in selecting a treatment option, but may also influence the prognosis significantly (such as tumorous perforation).
Today, it is only possible to manage oesophageal perforations with multidisciplinary co-operation. The role of a surgeon experienced in the treatment of perforations and that of a gastroenterologist familiar with new innovative endoscopic techniques are decisive. Treatment has to be administered individually with an understanding of the general principles involved.
Endoscopic procedures representing a minimal or significantly lower burden are more widely used not only in the diagnosis of oesophageal perforation, but also in its treatment. A number of publications, especially case histories, demonstrate the successful use of endoscopic clips and self-expanding stents in the treatment of oesophageal injuries[5,28]. The applicability of endoscopic methods has also been confirmed in experimental animal models (endoscopic clipping vs suturing vs thoracoscopic repair)[29]. Endoscopic clipping basically results in the immediate resolution of the oesophageal defect, while various types of stents aid in resolving extravasation from the oesophagus (diversion of enteral contents) and provide further slow healing of the injury. Stent implantation is mainly used in the treatment of large (> 2.5-3 cm) injuries of the middle and lower third segments of the oesophagus, and is especially suitable for the treatment of tumorous perforations where dysphagia is also resolved. Several types of stents are known, such as self-expanding plastic stents and fully and partially covered, self-expanding metal stents. In the case of injuries of the gastro-oesophageal junction, a partially covered stent is recommended with the smallest migration tendency if there is no oesophageal stricture[30]. The success of the procedure also depends on early application. Any delay in endoscopic treatment significantly reduces the chances of healing of the oesophageal perforation, as is the case with other treatment options[5]. According to the latest systematic review, the overall technical and clinical success rates of oesophageal stent placement in patient groups were 91% and 81%, respectively, and mortality was also acceptably low at 13%[31]. One of the most common complications of stent implantation is stent migration, which occurs in 20.8% of cases; this percentage is lower (11%) in the case of metal stents and higher for plastic stents (27%)[31]. However, stent migration may be reduced significantly with clips (proximal clip fixation[32]).
A method providing permanent continuous suction/drainage, is used in a number of areas with high efficacy, such as in the treatment of open abdomen, chronic wounds and suture insufficiency (rectum and oesophagus)[33]. The procedure is suitable for the treatment of chronic fistulas, particularly well-defined peri-oesophageal abscesses. It can also be used for intrathoracic oesophagus anastomosis insufficiency. It may be used to stimulate the formation of granulation tissue; therefore, the duration of prolonged secondary wound healing is decreased significantly[34-36]. Due to excessive granulation tissue formation, oesophageal stenosis can occur later within a 6%-40% range, but with an incidence of 15% in most cases[37]. Due to severe mediastinal/intrathoracic infection, the mortality rate is also naturally high (0%-20%) with this method[37].
Endoscopic clips have been used in the treatment of oesophageal perforation for 20 years; however, the number of publications on their use has only increased during the last few years. Generally, experience is available with two types of clip: the through-the-scope (TTS) clip and the over-the-scope clip (OTSC). TTS clips were developed for haemostasis and the treatment of mucosal ruptures. However, they may only be used in treating small (< 10 mm) injuries due to their limited (< 11 mm) wingspan.
The wingspan of the OTSC (OVESCO Endoscopy, Tübingen, Germany) is not significantly larger (11-14 mm), but the system also features a special applicator cap[38]. The entire thickness of the tissue may be pulled into the cap by suction and/or with graspers, and the tissue may be united with special clamps (a bear claw). Experience shows that this innovative clipping device made of biocompatible nitinol also provides stronger closure of large (1-2 cm) defects[39]. Nowadays, several types of clips are available (blunt/atraumatic and pointed-teeth/traumatic). There is also a special “anchor” which aids in the closure of fibrotic fistulas. It only takes an experienced endoscopic professional a few minutes to close a defect[40]. One iatrogenic oesophageal injury has been reported with the use of this device when an endoscopic OTSC was inserted[40]; the injury may have been caused by the 2 mm rim of the plastic cap. However, experience shows that the device can be used safely, and the complication rate is around 1%[40,41].
Tables 1 and 2 summarize the results of the PubMed (Medline) search.
| Ref. | Cause | Size/mm | Time to treatment | Im/Tm/Tp | Method | Nr | Clinical success | Additional treatment | Hospital stay /d | Follow-up |
| Wewalka et al[7] | Perforation (1) | < 10 | < 24 | Tm | Endoclip | 1/1 (100%) | None | ND | ND | |
| Rodella et al[44] | Leak (7) | 10-20 | > 24 | ND | Endoclip | ND | 2/7 (14%) | Yes | ND | 9.6 mo avg. |
| van Bodegraven et al[57] | Fistula (1) | 12 | > 24 | ND | Endoclip + argon beam electrocoagulation | ND | 1/1 (100%) | Yes | ND | 7 mo |
| Cipolletta et al[8] | Perforation (2) | 7-8 | < 24 | Im/Tm | Endoclip | 1 | 1/1 (100%) | No | 5 | 9 mo |
| 10 | < 24 | Im/Tm | Endoclip | 2 | 1/1 (100%) | No | 6 | 14 mo | ||
| Shimamoto et al[50] | Perforation (1) | 20 | < 24 | Tm | Endoclip | 3 | 1/1 (100%) | No | 37 | ND |
| Abe et al[58] | Perforation (1) | 5 | > 24 | Tm | Endoclip | ND | 1/1 (100%) | Yes | 36 | ND |
| Mizobuchi et al[59] | Fistula (1) | ND | > 24 | Tm | Endoclip | 1 | 1/1 (100%) | Yes | > 31 | ND |
| Raymer et al[9] | Fistula (3) | ≤ 25 | > 24 | Tm/Tp | Endoclip | ND | 3/3 (100%) | Yes | ND | ND |
| > 24 | Tm/Tp | Endoclip + surgery | ND | Yes | ND | ND | ||||
| > 24 | Tm/Tp | ND | Yes | ND | ND | |||||
| Shimizu et al[10] | Perforation (3) | 8/10/2008 | < 24 | Tm | Endoclip | ND | 3/3 (100%) | Yes | 14 | ND |
| Schubert et al[60] | Leak (1) | ND | > 24 | Tm | Stent + endoclip | ND | 1/1 (100%) | ND | ND | 1 mo |
| Wehrmann et al[45] | Perforation (4) | ND | > 24 | Tm | Endoclip | ND | 4/4 (100%) | Yes | 9-22 | 12 mo |
| Leak (3) | ND | > 24 | Tm | Endoscopic lavage + endoclip | ND | 3/3 (100%) | Yes | |||
| Matsuda et al[46] | Perforation (1) | 25 | < 24 | Im | Endoclip | ND | 1/1 (100%) | No | ND | ND |
| Sriram et al[11] | Perforation (1) | 10 | > 24 | Tm | Endoclip | ND | 1/1 (100%) | Yes | ND | ND |
| Fischer et al[61] | Perforation (4) | 20-40 | < 24 | Tm | Endoclip | 2-6 | 4/4 (100%) | No | 7-18 | No |
| < 24 | Tm | Endoclip | No | No | ||||||
| < 24 | Tm | Endoclip | No | No | ||||||
| < 24 | Tm | Endoclip | No | No | ||||||
| Gerke et al[62] | Perforation (1) | 15 | < 24 | Tm | Endoclip | 3 + 1 | 1/1 (100%) | No | 7 | 6 mo |
| Qadeer et al[28] | Fistula (1) | 3 | > 24 | Tm | Endoclip + stent | 4 | 1/1 (100%) | Yes | 65 | 17 mo |
| Luigiano et al[56] | Fistula (1) | 25 | > 24 | Tm | Endoclip | 5 | 1/1 (100%) | ND | ND | 1 mo |
| Endoloop | 1 | |||||||||
| Ivekovic et al[55] | Perforation (1) | 15 × 10 | ≤ 24 | Im/Tm | Endoloop | 1 | 1/1 (100%) | ND | ND | 4 wk |
| Endoclip | 4 | |||||||||
| Jung et al[63] | Perforation (1) | 25 | > 24 | Im/Tm | Endoclip | 12 | 1/1 (100%) | Yes | ND | 2 mo |
| Endoloop | 1 | |||||||||
| Rokszin et al[47] | Perforation (1) | 5-7 | < 24 | Tp | Endoclip | 3 | 1/1 (100%) | Yes | 14 | 6 mo |
| Coda et al[64] | Perforation (1) | 20 (distal) | < 24 | Tm | Endoclip | 6 | 1/1 (100%) | Yes | 15 | 6 mo |
| Sato et al[24] | Perforation (1) | ND | < 24 | Im/Tm | Endoclip | ND | 1/1 (100%) | No | ND | ND |
| Biancari et al[65] | Perforation (4) | 8 (median) | < 24 | Tm | Endoclip | ND | 3/4 (75%) | Yes | 32 (median) | No |
| Huang et al[66] | Perforation (4) | ND | < 24 | ND | Endoclip | 2 | 4/4 (100%) | ND | ND | ND |
| Ref. | Cause | Size/mm | Time to treatment (< 24 h <) | Im/Tm/Tp | Method | Nr | Clinical success | Additional treatment | Hospital stay /d | Follow-up |
| Pohl et al[67] | Leak (1) | < 0 | > 24 | Tp | OTSC | 1 | 1/1(100%) | No | 30 | ND |
| Perforation (1) | ND | > 24 | Tp | Surgery + stent + OTSC | 0/1(0%) | Yes | Died | ND | ||
| von Renteln et al[68] | Fistula (2) | ND | > 24 | Tm | OTSC | 1 | 0/2(0%) | ND | ND | ND |
| ND | > 24 | Tm | OTSC | 1 | Yes | ND | ND | |||
| Traina et al[69] | Fistula (1) | ND | > 24 | Tm | OTSC | 1 | 1/1(100%) | ND | ND | 4 wk |
| Albert et al[70] | Fistula (1) | ND | > 24 | Tm | OTSC | 1 | 1/1(100%) | ND | ND | 46 wk |
| Leak (1) | ND | > 24 | Tm | OTSC | 1 | 0/1(0%) | Stent | ND | 4 wk | |
| Leak (1) | ND | > 24 | Tm | OTSC | 1 | 1/1(100%) | ND | ND | 63 wk | |
| Kirschniak et al[71] | Leak (1) | ND | > 24 | ND | OTSC | ND | 1/1(100%) | ND | 10 | ND |
| Manta et al[72] | Fistula (1) | 8 × 4 | > 24 | Tm | OTSC + standard clips | 1+3 | 1/1(100%) | No | 0 | ND |
| Surace et al[73] | Leak (1) | ND | > 24 | ND | OTSC | ND | 1/1(100%) | ND | ND | ND |
| Baron et al[41] | Leak (3) | ND | > 24 | Tm | OTSC | 4 | 1/3(33%) | ND | ND | 77 avg. (30-330 d) |
| Perforation (1) | ND | < 24 | Tm | 1/1(100%) | ND | ND | ||||
| Hadj Amor et al[74] | Perforation (1) | 20 | < 24 | Tp | OTSC + stent | 1 | 1/1(100%) | VATS | ND | ND |
| Hagel et al[53] | Leak (2) | 28 × 13 | > 24 | Tm/Tp | OTSC | 3 | 1/2(50%) | Surgery | Died | 30 d |
| 8 × 4 | No | 12.3 ± 11 | 30 d | |||||||
| Perforation (2) | 8 × 3 | > 24 | Tm/Tp | OTSC | 1 | 0/2(0%) | Surgery | 30 d | ||
| 14 × 3 | > 24 | Surgery | 30 d | |||||||
| Jacobsen et al[75] | Perforation (3) | 9 | > 24 | ND | OTSC | 2 | 3/3(100%) | No | ND | ND |
| 10 (distal) | > 24 | ND | 1 | No | ND | ND | ||||
| 10 | > 24 | ND | 2 | No | ND | ND | ||||
| Markar et al[76] | Leak (1) | ND | > 24 | Tm | OTSC | 2 | 1/1(100%) | Yes | ND | 3 mo |
| Voermans et al[40] | Perforation (5) | < 30 | < 24 | ND | OTSC | ND | 5/5(100%) | No | ND | 6 mo |
| Zolotarevsky et al[77] | Fistula (1) | 5 | > 24 | ND | OTSC | ND | 1/1(100%) | ND | 7 | 3 mo |
| Braun et al[43] | Perforation (6) | 10-40 | < 24 | Tm/Tp | OTSC | 1-4 | 6/6(100%) | VATS | 9-19 | 6-12 wk |
| Ferreira et al[51] | Perforation (1) | 10 (distal) | > 24 | Tm | OTSC | 1 | 1/1(100%) | No | 21 | 3 mo |
| Noronha Ferreira et al[78] | Leak (1) | 10 × 6 | > 24 | Tm | OTSC | 1 | 1/1(100%) | No | 14 | ND |
| Nishiyama et al[79] | Perforation (1) | 20 | > 24 | ND | OTSC | ND | 1/1(100%) | ND | ND | 56 d |
| Ramhamadany et al[49] | Perforation (1) | ND | > 24 | ND | OTSC | ND | 1/1(100%) | Yes | ND | 6 mo |
| Bona et al[48] | Perforation (1) | 10 | > 24 | Tm/Tp | OTSC | 1 | 1/1(100%) | No | 28 | No |
| Haito-Chavez et al[42] | Perforation (10) | ND | < 24 | Tm/Tp | OTSC | 10/10(100%) | ND | ND | Median follow-up: 121-207 d | |
| Leaks (5) | ND | > 24 | Tm/Tp | 4/5(80%) | ND | ND | ||||
| Fistula (16) | ND | > 24 | Tm/Tp | 9/16(57%) | ND | ND | ||||
| Mönkemüller et al[52] | Fistula (4) | 10-15 | > 24 | ND | OTSC | 1-2 | 2/4(50%) | No | ND | 10 mo (1-10) |
| Leak (1) | 10-12 | > 24 | ND | OTSC | 0/1(0%) | No | ND |
We used the following key words: Oesophageal perforation, gastrointestinal perforation, endoscopic clip (ping) and OTSC (latest search date: 15 March 2015). We processed the data from 38 articles and 127 patients. We placed causes of perforation into three categories in the table: Perforation was defined as an acute iatrogenic or spontaneous defect, leak as an insufficiency/disruption of a surgical anastomosis, and fistula as a chronic residual inflammatory communication between the oesophagus, with a mediastinal or pleural space or tracheobronchial tract under the skin.
Statistical analysis: Categorical data were analyzed using χ2 and Fisher’s exact test [SPSS version 15.0 (© 2007 SPSS Inc.)].
Most publications are case reports or retrospective analyses with heterogeneous indications. The number of publications significantly increased after the first clinical use of the OTSC clip in 2007, first in Europe and then in the United States and other countries as well. Neither randomized nor comparative (TTS vs OTSC) studies have been conducted with the use of clips. One prospective European multicentre study and two retrospective North American multicentre studies have been published on the use of OTSC clips in the treatment of GI perforations[40-42]. Unfortunately, salient information is missing from numerous articles, and generally there are no reports on the follow-up period at all.
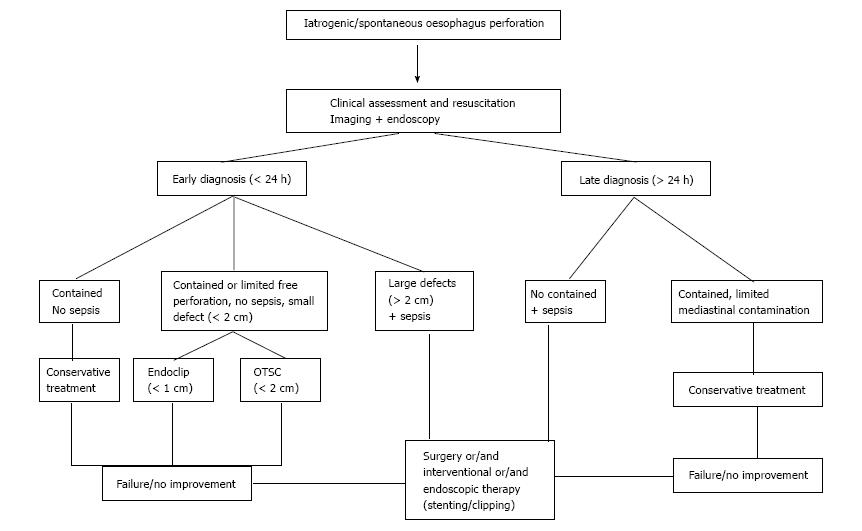
Based on the results, it can be concluded that both clips are suitable for the treatment and early management (< 24 h) of iatrogenic, spontaneous oesophageal perforation in the case of limited injury and contamination. TTS clips are successfully used for injuries of an average of 10 mm, while OTSC clips may also be successful in the treatment of larger injuries. More clips may also be used to close a defect, and various clips may be combined[40,43]; in addition, closure with a clip may be repeated[44]. In accordance with the latest recommendations from the European Society of Gastrointestinal Endoscopy[30], clips may only be used in the treatment of an injury in the case of safe care, in stable patients, with a clear oesophagus, limited mediastinal contamination and limited injury (intramural/transmural). Certain immediately diagnosed iatrogenic perforations meet this criterion system in particular. If the amount of mediastinal and/or pleural fluid is more significant, mediastinal and/or pleural space drainage/VATS treatment usually cannot be avoided. The treatment algorithm is summarized in Figure 1.
Based on our analysis (Tables 1 and 2), clips were used early (immediate diagnosis, < 24 h), especially in the case of minimally contaminated iatrogenic injuries or spontaneous ruptures, and the success of healing was similar to that of surgical treatment [TTS 88.8% (24/27); OTSC 92.86% (26/28)]. Although TTS and OTSC clips were used for injuries of varying sizes, their success rates did not diverge significantly (88.8% vs 92.85%, P > 0.12). Of further interest, clips were used with a similar success rate for the far smaller number of perforations of > 24 h which are only associated with a well-defined mediastinal inflammation/abscess [TTS 100% (8/8) vs OTSC 83.3% (5/6)]. Transoesophageal lavage of the process or even vacuum therapy may be of great aid in resolving the abscessing mediastinal process[45].
In selected cases of Boerhaave syndrome, closing the oesophageal injury with endoscopic clips might also be successful. TTS clips were used in two cases. In one patient, a minimal transmural oesophageal injury was diagnosed (a little air in the mediastinum), only the mucosal injury was partially closed with endoscopy, and conservative treatment was administered[46]. In another patient, a 5-7 mm transpleural injury was closed with 3 TTS clips, and additional thoracic drainage and enteral nutrition were administered[47]. In three additional cases, OTSC clips were used successfully to close a spontaneous transmural injury[43,48,49]. In the two matured (> 24 h) perforations, additional VATS therapy was necessary. Similarly, only limited cases have been reported on the treatment of injuries caused by foreign bodies[50,51].
Broad-spectrum antibiotic therapy and suspension of oral nutrition are required in addition to successful early endoscopic care. In the majority of cases, complication-free healing can be expected with careful indication. However, close monitoring of the patient and additional therapy such as mediastinal/pleural drainage or even surgical treatment, if necessary, are also essential.
Fistulizing chronic injuries and treating anastomosis insufficiencies represent a separate group. Experience shows that OTSC clips have provided relatively secure closure so far, but the success rate in acute cases [OTSC 57.7% (15/26) vs TTS 100% (4/4) (P < 0.05) for fistulas; OTSC 77.7% (12/18) vs TTS 54.5% (6/11) (P < 0.05) for leaks] differed significantly in the groups.
Closure is technically often unfeasible, especially in the case of fibrotizing, scarred fistulas and a severely inflamed environment[52]. Most problems stem from insufficiency of the oesophageal anastomosis diagnosed in the early postoperative state. These cases are usually subacute, the tissues are extremely fragile, often ischaemic, and therefore the tendency to heal is already decreased[53]. The success rate for the closure of chronic fistulas is also reduced by previous radiation therapy. If a TTS clip is used, argon plasma coagulation and other mechanical freshening up (with a cytology brush) may aid in stabilizing the clip. These extra manoeuvres may only increase tissue oedema and the success of clip deployment when OTSC clips are used[41,52]. There are only a few case reports on successful closure of a chronic spontaneous oesophageal rupture and a consequently developed fistula with endoscopic clips[9,11].
Endoscopic vacuum therapy may be helpful in reducing the inflammatory cavity and closing the remaining fistula with good localization in the case of chronic injuries and mediastinal/pleural inflammation[37,45]. Following initial stent placement and removal in the treatment of an early, well-defined injury, a cavity marked by chronic inflammation may remain, one which may not be resolved with primary clipping alone. In these cases, EVT and/or surgical treatment (VATS) represent the primary therapeutic procedure[34-36,45].
Very few articles report long-term follow-up data. The biggest and most detailed report is a North American study which evaluated gastrointestinal defects in 188 patients treated with OTSC. Success was achieved in 60.2% of the patients in a median follow-up of 146 d. The long-term rate for clinically successful closure of perforations (90%) and leaks (73.3%) was significantly higher than that of fistulas (42.9%). The study also showed significantly greater long-term success when OTSCs were used in primary therapy.
On the whole, it is clear that closure with clips shows the best results in the treatment of early injuries, and the success rate for clinical recovery approaches the result for surgical treatment.
Endoscopic clips may also be used with endoloop. The method was first used for endoscopic mucosal resection to resolve large defects[54]. Later, it was successful in the treatment of Mallory-Weis syndrome[55] and in closing oesophageal fistulas[56]. Due to the limited number of these articles, no conclusions can be drawn about their efficacy.
A number of case reports and case series reports have been published on the successful outcome of clip closure of endoscopic perforations, but high-evidence, case-controlled, multicentre studies are still missing. This method can only be used under very strict conditions (Figure 1). The introduction of OTSC clips significantly increases the size of treatable lesions (from 1 to 2-3 cm). However, this technique is only used in a limited number of centres. It is important to point out that both conventional TTS and the new OTSC methods are both safe. But a learning curve period and experience will both be necessary in their usage, including the selection of patients suitable for clip treatment. Multidisciplinary teams (surgeon, endoscopy specialist and intensive care therapist) are further important conditions in the successful treatment of oesophageal perforations. Surgical treatment still constitutes the primary therapy in oesophageal perforation. Based on the results so far, we can state that endoscopic closure of early, well-defined oesophageal perforations represents a therapeutic alternative to surgical treatment.
P- Reviewer: Kuehn F, Natsugoe S S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
| 1. | Bufkin BL, Miller JI, Mansour KA. Esophageal perforation: emphasis on management. Ann Thorac Surg. 1996;61:1447-1451; discussion 1451-1452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 181] [Cited by in F6Publishing: 188] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Sakamoto Y, Tanaka N, Furuya T, Ueno T, Okamoto H, Nagai M, Murakawa T, Takayama T, Mafune K, Makuuchi M. Surgical management of late esophageal perforation. Thorac Cardiovasc Surg. 1997;45:269-272. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Skinner DB, Little AG, DeMeester TR. Management of esophageal perforation. Am J Surg. 1980;139:760-764. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 156] [Cited by in F6Publishing: 167] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Tilanus HW, Bossuyt P, Schattenkerk ME, Obertop H. Treatment of oesophageal perforation: a multivariate analysis. Br J Surg. 1991;78:582-585. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 62] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Fischer A, Thomusch O, Benz S, von Dobschuetz E, Baier P, Hopt UT. Nonoperative treatment of 15 benign esophageal perforations with self-expandable covered metal stents. Ann Thorac Surg. 2006;81:467-472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 160] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 6. | Johnsson E, Lundell L, Liedman B. Sealing of esophageal perforation or ruptures with expandable metallic stents: a prospective controlled study on treatment efficacy and limitations. Dis Esophagus. 2005;18:262-266. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 104] [Cited by in F6Publishing: 107] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Wewalka FW, Clodi PH, Haidinger D. Endoscopic clipping of esophageal perforation after pneumatic dilation for achalasia. Endoscopy. 1995;27:608-611. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 58] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Cipolletta L, Bianco MA, Rotondano G, Marmo R, Piscopo R, Meucci C. Endoscopic clipping of perforation following pneumatic dilation of esophagojejunal anastomotic strictures. Endoscopy. 2000;32:720-722. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Raymer GS, Sadana A, Campbell DB, Rowe WA. Endoscopic clip application as an adjunct to closure of mature esophageal perforation with fistulae. Clin Gastroenterol Hepatol. 2003;1:44-50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Shimizu Y, Kato M, Yamamoto J, Nakagawa S, Komatsu Y, Tsukagoshi H, Fujita M, Hosokawa M, Asaka M. Endoscopic clip application for closure of esophageal perforations caused by EMR. Gastrointest Endosc. 2004;60:636-639. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 53] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Sriram PV, Rao GV, Reddy ND. Successful closure of spontaneous esophageal perforation (Boerhaave’s syndrome) by endoscopic clipping. Indian J Gastroenterol. 2006;25:39-41. [PubMed] [Cited in This Article: ] |
| 12. | Bhatia P, Fortin D, Inculet RI, Malthaner RA. Current concepts in the management of esophageal perforations: a twenty-seven year Canadian experience. Ann Thorac Surg. 2011;92:209-215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Biancari F, D’Andrea V, Paone R, Di Marco C, Savino G, Koivukangas V, Saarnio J, Lucenteforte E. Current treatment and outcome of esophageal perforations in adults: systematic review and meta-analysis of 75 studies. World J Surg. 2013;37:1051-1059. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 156] [Cited by in F6Publishing: 154] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 14. | Chuah SK, Wu KL, Hu TH, Tai WC, Changchien CS. Endoscope-guided pneumatic dilation for treatment of esophageal achalasia. World J Gastroenterol. 2010;16:411-417. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 22] [Cited by in F6Publishing: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstätter M, Lin F, Ciovica R. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg. 2009;249:45-57. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 481] [Cited by in F6Publishing: 433] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 16. | Lynch KL, Pandolfino JE, Howden CW, Kahrilas PJ. Major complications of pneumatic dilation and Heller myotomy for achalasia: single-center experience and systematic review of the literature. Am J Gastroenterol. 2012;107:1817-1825. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 17. | Piotet E, Escher A, Monnier P. Esophageal and pharyngeal strictures: report on 1,862 endoscopic dilatations using the Savary-Gilliard technique. Eur Arch Otorhinolaryngol. 2008;265:357-364. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Neuhaus H. ESD around the world: Europe. Gastrointest Endosc Clin N Am. 2014;24:295-311. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Giménez A, Franquet T, Erasmus JJ, Martínez S, Estrada P. Thoracic complications of esophageal disorders. Radiographics. 2002;22 Spec No:S247-S258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 120] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 20. | Fadoo F, Ruiz DE, Dawn SK, Webb WR, Gotway MB. Helical CT esophagography for the evaluation of suspected esophageal perforation or rupture. AJR Am J Roentgenol. 2004;182:1177-1179. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 83] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Carrott PW, Low DE. Advances in the management of esophageal perforation. Thorac Surg Clin. 2011;21:541-555. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Kowalczyk L, Forsmark CE, Ben-David K, Wagh MS, Chauhan S, Collins D, Draganov PV. Algorithm for the management of endoscopic perforations: a quality improvement project. Am J Gastroenterol. 2011;106:1022-1027. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Kuppusamy MK, Felisky C, Kozarek RA, Schembre D, Ross A, Gan I, Irani S, Low DE. Impact of endoscopic assessment and treatment on operative and non-operative management of acute oesophageal perforation. Br J Surg. 2011;98:818-824. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Sato H, Inoue H, Ikeda H, Grace R Santi E, Yoshida A, Onimaru M, Kudo S. Clinical experience of esophageal perforation occurring with endoscopic submucosal dissection. Dis Esophagus. 2014;27:617-622. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Lawrence DR, Ohri SK, Moxon RE, Townsend ER, Fountain SW. Primary esophageal repair for Boerhaave’s syndrome. Ann Thorac Surg. 1999;67:818-820. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 87] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 26. | Sabanathan S, Eng J, Richardson J. Surgical management of intrathoracic oesophageal rupture. Br J Surg. 1994;81:863-865. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 43] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Lázár G, Paszt A, Simonka Z, Bársony A, Abrahám S, Horváth G. A successful strategy for surgical treatment of Boerhaave’s syndrome. Surg Endosc. 2011;25:3613-3619. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Qadeer MA, Dumot JA, Vargo JJ, Lopez AR, Rice TW. Endoscopic clips for closing esophageal perforations: case report and pooled analysis. Gastrointest Endosc. 2007;66:605-611. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 102] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 29. | Fritscher-Ravens A, Hampe J, Grange P, Holland C, Olagbeye F, Milla P, von Herbay A, Jacobsen B, Seehusen F, Hadeler KG. Clip closure versus endoscopic suturing versus thoracoscopic repair of an iatrogenic esophageal perforation: a randomized, comparative, long-term survival study in a porcine model (with videos). Gastrointest Endosc. 2010;72:1020-1026. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 30. | Paspatis GA, Dumonceau JM, Barthet M, Meisner S, Repici A, Saunders BP, Vezakis A, Gonzalez JM, Turino SY, Tsiamoulos ZP. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2014;46:693-711. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 197] [Cited by in F6Publishing: 173] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 31. | Dasari BV, Neely D, Kennedy A, Spence G, Rice P, Mackle E, Epanomeritakis E. The role of esophageal stents in the management of esophageal anastomotic leaks and benign esophageal perforations. Ann Surg. 2014;259:852-860. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 171] [Cited by in F6Publishing: 187] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 32. | Vanbiervliet G, Filippi J, Karimdjee BS, Venissac N, Iannelli A, Rahili A, Benizri E, Pop D, Staccini P, Tran A. The role of clips in preventing migration of fully covered metallic esophageal stents: a pilot comparative study. Surg Endosc. 2012;26:53-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 120] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 33. | Loske G, Schorsch T, Müller C. Endoscopic vacuum sponge therapy for esophageal defects. Surg Endosc. 2010;24:2531-2535. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 34. | Loske G, Schorsch T, Müller C. Endoscopic intracavitary vacuum therapy of Boerhaave’s syndrome: a case report. Endoscopy. 2010;42 Suppl 2:E144-E145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Ahrens M, Schulte T, Egberts J, Schafmayer C, Hampe J, Fritscher-Ravens A, Broering DC, Schniewind B. Drainage of esophageal leakage using endoscopic vacuum therapy: a prospective pilot study. Endoscopy. 2010;42:693-698. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 92] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 36. | Loske G, Schorsch T, Müller C. Intraluminal and intracavitary vacuum therapy for esophageal leakage: a new endoscopic minimally invasive approach. Endoscopy. 2011;43:540-544. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 83] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 37. | Mennigen R, Senninger N, Laukoetter MG. Novel treatment options for perforations of the upper gastrointestinal tract: endoscopic vacuum therapy and over-the-scope clips. World J Gastroenterol. 2014;20:7767-7776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 89] [Cited by in F6Publishing: 80] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 38. | Kirschniak A, Kratt T, Stüker D, Braun A, Schurr MO, Königsrainer A. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162-167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 238] [Cited by in F6Publishing: 222] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 39. | Parodi A, Repici A, Pedroni A, Blanchi S, Conio M. Endoscopic management of GI perforations with a new over-the-scope clip device (with videos). Gastrointest Endosc. 2010;72:881-886. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 145] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 40. | Voermans RP, Le Moine O, von Renteln D, Ponchon T, Giovannini M, Bruno M, Weusten B, Seewald S, Costamagna G, Deprez P. Efficacy of endoscopic closure of acute perforations of the gastrointestinal tract. Clin Gastroenterol Hepatol. 2012;10:603-608. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 137] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 41. | Baron TH, Song LM, Ross A, Tokar JL, Irani S, Kozarek RA. Use of an over-the-scope clipping device: multicenter retrospective results of the first U.S. experience (with videos). Gastrointest Endosc. 2012;76:202-208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 137] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 42. | Haito-Chavez Y, Law JK, Kratt T, Arezzo A, Verra M, Morino M, Sharaiha RZ, Poley JW, Kahaleh M, Thompson CC. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video). Gastrointest Endosc. 2014;80:610-622. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 204] [Cited by in F6Publishing: 190] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 43. | Braun A, Richter-Schrag HJ, Fischer A, Hoeppner J. Minimally invasive therapy of perforations at the esophagogastric junction by over-the-scope clipping. Endoscopy. 2013;45 Suppl 2 UCTN:E133-E134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 44. | Rodella L, Laterza E, De Manzoni G, Kind R, Lombardo F, Catalano F, Ricci F, Cordiano C. Endoscopic clipping of anastomotic leakages in esophagogastric surgery. Endoscopy. 1998;30:453-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 104] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 45. | Wehrmann T, Stergiou N, Vogel B, Riphaus A, Köckerling F, Frenz MB. Endoscopic debridement of paraesophageal, mediastinal abscesses: a prospective case series. Gastrointest Endosc. 2005;62:344-349. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 51] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 46. | Matsuda A, Miyashita M, Sasajima K, Nomura T, Makino H, Matsutani T, Katsuno A, Sasaki J, Tajiri T. Boerhaave syndrome treated conservatively following early endoscopic diagnosis: a case report. J Nippon Med Sch. 2006;73:341-345. [PubMed] [Cited in This Article: ] |
| 47. | Rokszin R, Simonka Z, Paszt A, Szepes A, Kucsa K, Lazar G. Successful endoscopic clipping in the early treatment of spontaneous esophageal perforation. Surg Laparosc Endosc Percutan Tech. 2011;21:e311-e312. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 48. | Bona D, Aiolfi A, Rausa E, Bonavina L. Management of Boerhaave’s syndrome with an over-the-scope clip. Eur J Cardiothorac Surg. 2014;45:752-754. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 49. | Ramhamadany E, Mohamed S, Jaunoo S, Baker T, Mannath J, Harding J, Menon V. A delayed presentation of Boerhaave’s syndrome with mediastinitis managed using the over-the-scope clip. J Surg Case Rep. 2013;2013:rjt020. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 50. | Shimamoto C, Hirata I, Umegaki E, Katsu K. Closure of an esophageal perforation due to fish bone ingestion by endoscopic clip application. Gastrointest Endosc. 2000;51:736-739. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 51. | Ferreira AO, Lopes J, Velosa J. Snapper fishbone esophageal perforation closed with an over-the-scope-clip. BMJ Case Rep. 2013;2013:bcr2013201614. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 52. | Mönkemüller K, Peter S, Toshniwal J, Popa D, Zabielski M, Stahl RD, Ramesh J, Wilcox CM. Multipurpose use of the ‘bear claw’ (over-the-scope-clip system) to treat endoluminal gastrointestinal disorders. Dig Endosc. 2014;26:350-357. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 53. | Hagel AF, Naegel A, Lindner AS, Kessler H, Matzel K, Dauth W, Neurath MF, Raithel M. Over-the-scope clip application yields a high rate of closure in gastrointestinal perforations and may reduce emergency surgery. J Gastrointest Surg. 2012;16:2132-2138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 54. | DAVE Project - Gastroenterology. Editors: Kelsey PB, Bounds BC, Raju, GS, Collier DF. Video: Tulip bundle technique: a novel technique for closing perforations caused by endoscopic resection, by placement of clips and approximation with endoloops. Available from: http: //www.podcastchart.com/podcasts/dave-project-gastroenterology/episodes/video-tulip-bundle-technique-a-novel-technique-for-closing-perforations-caused-by-endoscopic-resection-by-placement-of-clips-and-approximation-with-endoloops. [Cited in This Article: ] |
| 55. | Ivekovic H, Rustemovic N, Brkic T, Opacic M, Pulanic R, Ostojic R, Vucelic B. The esophagus as a working channel: successful closure of a large Mallory-Weiss tear with clips and an endoloop. Endoscopy. 2011;43 Suppl 2 UCTN:E170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 56. | Luigiano C, Ferrara F, Polifemo AM, Fabbri C, Ghersi S, Bassi M, D’Imperio N. Endoscopic closure of esophageal fistula using a novel “clips and loop” method. Endoscopy. 2009;41 Suppl 2:E249-E250. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 57. | van Bodegraven AA, Kuipers EJ, Bonenkamp HJ, Meuwissen SG. Esophagopleural fistula treated endoscopically with argon beam electrocoagulation and clips. Gastrointest Endosc. 1999;50:407-409. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 48] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 58. | Abe N, Sugiyama M, Hashimoto Y, Itoh N, Nakaura H, Izumisato Y, Matsuoka H, Masaki T, Nakashima M, Mori T. Endoscopic nasomediastinal drainage followed by clip application for treatment of delayed esophageal perforation with mediastinitis. Gastrointest Endosc. 2001;54:646-648. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 59. | Mizobuchi S, Kuge K, Maeda H, Matsumoto Y, Yamamoto M, Sasaguri S. Endoscopic clip application for closure of an esophagomediastinal-tracheal fistula after surgery for esophageal cancer. Gastrointest Endosc. 2003;57:962-965. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 60. | Schubert D, Scheidbach H, Kuhn R, Wex C, Weiss G, Eder F, Lippert H, Pross M. Endoscopic treatment of thoracic esophageal anastomotic leaks by using silicone-covered, self-expanding polyester stents. Gastrointest Endosc. 2005;61:891-896. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 156] [Cited by in F6Publishing: 168] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 61. | Fischer A, Schrag HJ, Goos M, von Dobschuetz E, Hopt UT. Nonoperative treatment of four esophageal perforations with hemostatic clips. Dis Esophagus. 2007;20:444-448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 62. | Gerke H, Crowe GC, Iannettoni MD. Endoscopic closure of cervical esophageal perforation caused by traumatic insertion of a mucosectomy cap. Ann Thorac Surg. 2007;84:296-298. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 63. | Jung JH, Kim JI, Song JH, Kim JH, Lee SH, Cheung DY, Park SH, Kim JK. A case of Sengstaken-Blakemore tube-induced esophageal rupture repaired by endoscopic clipping. Intern Med. 2011;50:1941-1945. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 64. | Coda S, Antonellis F, Tsagkaropulos S, Francioni F, Trentino P. Complete endoscopic closure (clipping) of a large esophageal perforation after pneumatic dilation in a patient with achalasia. J Laparoendosc Adv Surg Tech A. 2012;22:815-818. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 65. | Biancari F, Saarnio J, Mennander A, Hypén L, Salminen P, Kuttila K, Victorzon M, Böckelman C, Tarantino E, Tiffet O. Outcome of patients with esophageal perforations: a multicenter study. World J Surg. 2014;38:902-909. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 66. | Huang J, Wen W, Tang X, Fan Z, Song H, Wang K. Cap-assisted clip closure of large esophageal perforations caused by a duodenoscope during endoscopic retrograde cholangiopancreatography (with video). Surg Laparosc Endosc Percutan Tech. 2014;24:e101-e105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 67. | Pohl J, Borgulya M, Lorenz D, Ell C. Endoscopic closure of postoperative esophageal leaks with a novel over-the-scope clip system. Endoscopy. 2010;42:757-759. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 68. | von Renteln D, Denzer UW, Schachschal G, Anders M, Groth S, Rösch T. Endoscopic closure of GI fistulae by using an over-the-scope clip (with videos). Gastrointest Endosc. 2010;72:1289-1296. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 69. | Traina M, Curcio G, Tarantino I, Soresi S, Barresi L, Vitulo P, Gridelli B. New endoscopic over-the-scope clip system for closure of a chronic tracheoesophageal fistula. Endoscopy. 2010;42 Suppl 2:E54-E55. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 70. | Albert JG, Friedrich-Rust M, Woeste G, Strey C, Bechstein WO, Zeuzem S, Sarrazin C. Benefit of a clipping device in use in intestinal bleeding and intestinal leakage. Gastrointest Endosc. 2011;74:389-397. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 71. | Kirschniak A, Subotova N, Zieker D, Königsrainer A, Kratt T. The Over-The-Scope Clip (OTSC) for the treatment of gastrointestinal bleeding, perforations, and fistulas. Surg Endosc. 2011;25:2901-2905. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 169] [Cited by in F6Publishing: 193] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 72. | Manta R, Manno M, Bertani H, Barbera C, Pigò F, Mirante V, Longinotti E, Bassotti G, Conigliaro R. Endoscopic treatment of gastrointestinal fistulas using an over-the-scope clip (OTSC) device: case series from a tertiary referral center. Endoscopy. 2011;43:545-548. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 111] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 73. | Surace M, Mercky P, Demarquay JF, Gonzalez JM, Dumas R, Ah-Soune P, Vitton V, Grimaud J, Barthet M. Endoscopic management of GI fistulae with the over-the-scope clip system (with video). Gastrointest Endosc. 2011;74:1416-1419. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 74. | Hadj Amor WB, Bonin EA, Vitton V, Desjeux A, Grimaud JC, Barthet M. Successful endoscopic management of large upper gastrointestinal perforations following EMR using over-the-scope clipping combined with stenting. Endoscopy. 2012;44 Suppl 2 UCTN:E277-E278. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 75. | Jacobsen GR, Coker AM, Acosta G, Talamini MA, Savides TJ, Horgan S. Initial experience with an innovative endoscopic clipping system. Surg Technol Int. 2012;22:39-43. [PubMed] [Cited in This Article: ] |
| 76. | Markar SR, Koehler R, Low DE, Ross A. Novel multimodality endoscopic closure of postoperative esophageal fistula. Int J Surg Case Rep. 2012;3:577-579. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 77. | Zolotarevsky E, Kwon Y, Bains M, Schattner M. Esophagobronchial fistula closure using a novel endoscopic over-the-scope-clip. Ann Thorac Surg. 2012;94:e69-e70. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 78. | Noronha Ferreira C, Ribeiro LC, Velosa J, Ferreira J, Ferreira C, Freire JP, Marques J, Ruivo A, Bicha Castelo H. Total gastrectomy in an elderly patient complicated by esophageal fistula: rescue by the over-the-scope clip. Gastrointest Endosc. 2013;77:497-498. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 79. | Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, Oryu M, Masaki T. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752-2760. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 101] [Cited by in F6Publishing: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |