Published online Aug 27, 2015. doi: 10.4240/wjgs.v7.i8.152
Peer-review started: March 21, 2015
First decision: April 10, 2015
Revised: June 3, 2015
Accepted: June 18, 2015
Article in press: June 19, 2015
Published online: August 27, 2015
AIM: To help the surgeon in decision making when treating a patient with recurrent gallstone ileus (RGSI).
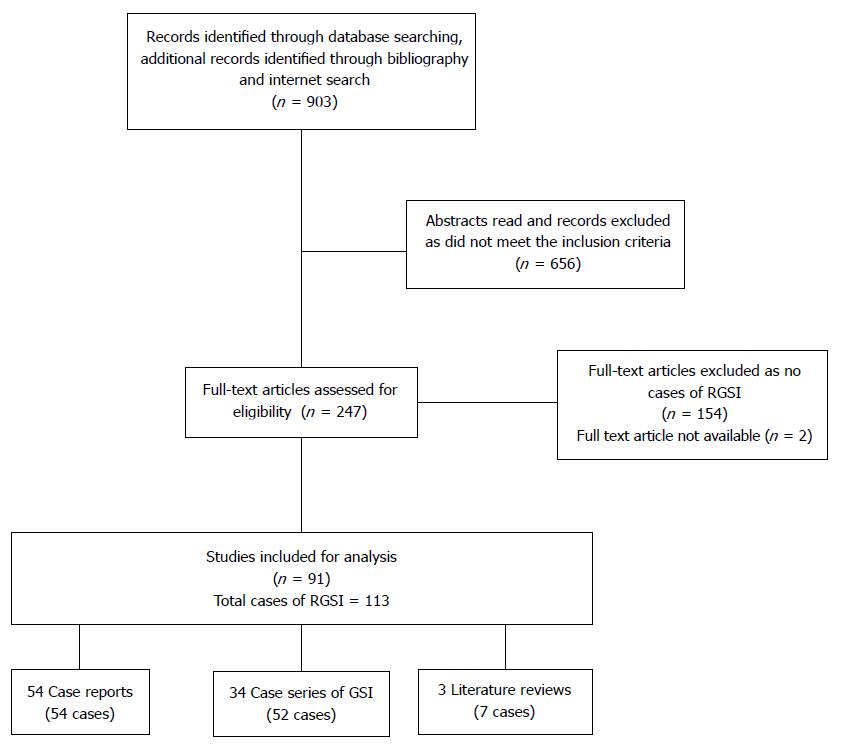
METHODS: A systematic review related to RGSI was performed using the databases CINAHL, EMBASE, MEDLINE via PubMed from May 1912 to April 2015. All languages were included and the grey literature was also searched. The abstracts were explored for relevance to the topic and full texts obtained as appropriate. A manual search was carried out by scrutinising the reference lists of all the full text articles and further articles were identified and obtained. Total of 903 articles were identified, 656 were excluded after abstract review, 247 full text articles were reviewed and 91 articles selected for final analysis. There were 113 cases of RGSI.
RESULTS: There were 113 cases of RGSI reported in 91 articles. The majority of the recurrences, 62.6%, occurred within 6 wk of the index event. The male to female ratio was 1:7. The mean age was 69.6 years (SD 11.2) with a range of 38-95 years. The small bowel was the commonest site of impaction (92.2%). Treatment data was available for 104 patients. The two main operations performed were: (1) Enterolithotomy without repair of biliary fistula in 70.1% of all patients with a procedural mortality rate of 16.4% (12/73) and (2) a single stage surgery approach involving enterolithotomy with cholecystectomy and repair of the biliary enteric fistula in 16.3% with a procedural mortality of 11.7% (2/17). A subset analysis over last 25 years showed mortality from eneterolithotomy was 4.8% while single stage mortality was 22.2%. Enterolithotomy alone was the commonest operation performed for RGSI with four patients (5.4%) having a further recurrence of gallstone ileus.
CONCLUSION: Enterolithotomy alone or followed by a delayed two-stage treatment approach is the preferred choice offering low mortality and reduced risk of recurrence.
Core tip: Recurrent gallstone ileus, is an acute but rare surgical condition and there is no clear evidence at present as to the appropriate management of this surgical condition. This review will provide a framework to help decision making for this condition when confronted as an emergency by the general surgeon.
- Citation: Mir SA, Hussain Z, Davey CA, Miller GV, Chintapatla S. Management and outcome of recurrent gallstone ileus: A systematic review. World J Gastrointest Surg 2015; 7(8): 152-159
- URL: https://www.wjgnet.com/1948-9366/full/v7/i8/152.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i8.152
Gallstone ileus (GSI) is a rare entity first described in 1654 by Bartholini[1,2]. GSI is a result of an inflamed gallbladder becoming adherent to an adjacent part of the enteric system and discharging its stones into the enteric lumen through formation of a biliary-enteric fistula[3-5]. It is estimated that 80% of intraluminal stones will pass spontaneously[6], Gallstones measuring more than 2.5 cm in diameter are a risk factor for impaction and causing bowel obstruction[7]; the latter is referred to as GSI. The mainstay of management is surgical treatment involving enterolithotomy alone or combined with a cholecystectomy and repair of biliary-enteric fistula as a single stage procedure.
Recurrent gallstone ileus (RGSI) is usually a consequence of an untreated biliary-enteric fistula with cholelithiasis[8]. An alternative hypothesis is the presence of a non obstructive biliary calculus more proximal in the small intestine which escaped detection at the first operation despite the need to palpate the entire small bowel looking for a second stone[9]. Predicting the risk of RGSI at the time of first operation is difficult. The literature reports an estimated risk of RGSI of 5%-8%[10-12].
When a patient presents with RGSI the surgeon will not only have to consider how to deal with the emergency obstruction but also how best to manage the cause of the recurrence. There are advocates for enterolithotomy alone without dealing with the biliary-enteric fistula, as low morbidity and mortality are perceived to be associated with this approach. However the advantages of repairing the fistula include preventing recurrence, ascending cholangitis and gallstone related complications[13-15]. These issues are similar to the ones at primary presentation of Gall Stone ileus but increase in significance now as at the primary presentation the risk of recurrence is only 5%-8%.
Although there have been several reviews of GSI, there has been no review focusing on RGSI since 1998[11]. Following a case in our hospital where a patient presented with two recurrences of GSI[16], we performed an up to date systematic review to gain a better understanding of its presentation, management and outcomes. This review will assist clinicians with the management of this rare but important condition.
To perform a systematic review of the literature from May 1912 to April 2015 to accumulate a body of evidence to help clinicians in the management of patients with RGSI.
An electronic search was performed using CINAHL, EMBASE, MEDLINE via PubMed, from inception of each database to April 2015. A web-based search was also carried out using the Boolean Internet search engine “Google”. The search terms used were; “recurrent” or “recurrence” and “intestinal obstruction”, “gallstone” or “GSI”. The search included articles written in any language.
The abstracts were explored for relevance to the topic and full texts obtained as appropriate. A manual search was carried out by scrutinising the reference lists of all the full text articles and further articles were identified and obtained.
A search of the grey literature was undertaken by searching the Royal College of Surgeon’s website and a search of the grey literature database Open Grey http://www.opengrey.eu/. No further articles were identified.
Thirty-six articles of potential relevance in languages other than English were identified. All the articles were translated by native speakers in health related professions. The translations were independently reviewed by the authors before a decision was made about whether the papers were relevant for this review. Of the 36 articles identified, 20 were subsequently included.
The definition of a RGSI event was based on a confirmed recurrence of intestinal obstruction by a gallstone demonstrated radiologically or intra-operatively. No article with a case of recurrence of GSI was excluded; papers with incomplete data were included.
Two authors (MS and ZH) independently extracted the data. Data extracted included the names of the authors, date of publication and language. Other data included demographic information about each patient and clinical data such as surgical history, stone characteristics, time interval from the first operation to onset of symptoms, search for second stone at the time of first operation, site of obstruction and its relation to previous enterolithotomy, and details of the surgery performed. Mortality and morbidity were also noted.
The data analysis was limited to descriptive statistics. No meta–analysis was performed.
The search identified 903 articles from multiple sources as described. Ninety one articles were eventually included (Figure 1). These included 54 individual case reports, 34 case series and 3 review articles[10,17,18]. There were 113 cases of RGSI documented in the 91 articles. Full data were not available on all the categories of interest. Consequently the denominator for each category varies. This is made explicit in the text.
Data on age was available for 89 people. The mean age of these patients was 69.6 years (SD 11.2) with an age range of 38-95 years. The average age in males was 64.5 years (SD 15.1) with an age range of 38-94 years. The average age in females was 70.4 years (SD 10.4) with an age range of 44-95 years.
Data on gender was available for 99 cases. There were 12 males and 87 females (M: F ratio of 1:7). It was not possible to extract the data for age and gender in some case series where data was provided as an aggregate.
The treatment strategies were divided into two broad categories: (1) treatment to relieve intestinal obstruction alone; and (2) treatment to prevent recurrence, i.e., enterolithotomy + cholecystectomy + repair of biliary enteric fistula.
We looked at the treatment given for the first episode of GSI that resulted in subsequent recurrence. Data for treatment of this primary gall stone ileus was available for 106 of the 113 patients. The first episode of GSI was treated with enterolithotomy in 92 patients, 86.7%. Five people (4.9%) were treated conservatively and offending stone removed via rectum. A single stage surgical approach in two patients (1.9%) still resulted in RGSI. The two patients treated by a single stage procedure by Rodriguez[5] developed recurrence of symptoms two weeks postoperatively. Rodriguez does not mention whether a second stone was missed at the time of the first operation. Other operations included small bowel resection, colostomy, pyloroplasty, gastrostomy accounting for 11.7%.
Cooperman[19] performed transverse colotomy for GSI in a patient who had cholecystostomy three months prior to the first episode of GSI.
The majority of the recurrences were experienced in the early postoperative period.
In our review, 67 of 107 patients (62.6%) experienced recurrence within six weeks of being treated for GSI. Within six months 91 of the patients out of 107 (85%) had experienced recurrent symptoms. The range varied from 1 d to 3287 d. The median time was 26 d with an interquartile range of 10-90 d.
Of the 16 patients who presented with RGSI after six months, nine had a recurrence of symptoms between six months and a year and seven patients a year or more after the index procedure. We could not elicit data on whether the entire small bowel was palpated for a second gallstone at the primary operation, i.e., whether the reason for RGSI was a missed second gallstone at primary presentation.
The ileum was the commonest site of the stone impaction. Small bowel was the site of obstruction in 92.2% of the patients with RGSI. The recurrent stone was impacted in ileum in 49.5% of the patients. Colon and rectum impaction was seen in 3.8% of the cases respectively.
The mean size of the obstructing stone was 3.6 cm with a range of 1.5-6 cm. The smallest stone that caused obstruction in the small bowel was 1.5 cm[20] and in the large bowel was 3 cm[21].
The size of the stone appeared to have no correlation with the site of obstruction. The largest impacted stone, measuring 6 cm, was found in the duodenum. The largest stone in the small bowel was 5.5 cm and in the large bowel, 5 cm.
At the time of second laparotomy for RGSI, intestinal obstruction occurred as a consequence of a single stone in 75 cases (89.2%). Two or more stones were found in 9 cases (10.7%), information was not available for 29 cases.
Goldstein[22] published a case in which multiple stones were found at both the laparotomies for GSI.
The vast majority of the gallstones were faceted in shape. Where the information was found 83.3% of the patients (30 of 36) were faceted in shape. In case of a faceted stone being found at the first surgery the likelihood of finding a second stone is very high and multiple authors have advocated a through search of the residual GI tract to omit recurrence of GSI.
The information comparing the site of obstruction at the first and the second episode was available for 75 patients. In 32 patients (42.5%) the site of impaction was distal to the previous enterolithotomy. In 17 patients (22.6%) the stone impacted at the site of the previous repair, while in 26 patients (34.6%) the site of impaction was proximal to the site of the previous enterolithotomy.
Information related to specific treatment for RGSI was available in 104 patients.
In our review the following treatment strategies were adopted.
Enterolithotomy was performed on its own as the main surgical method of relieving the intestinal obstruction in RGSI in 73 patients. When performed on its own it carried a mortality rate of 16.4% (Table 1).
| Treatment | n | % | Mortality | % |
| Enterolithotomy1 | 73 | 83.9 | 12 | 16.4 |
| Small bowel resection | 4 | 4.5 | 1 | 25 |
| Conservative +/manual evacuation | 8 | 9.1 | 2 | 25 |
| OGD YAG laser lithotripsy | 1 | 1.1 | 0 | 0 |
| Loop colostomy | 1 | 1.1 | 0 | 0 |
Seven patients treated initially with enterolithotomy alone underwent a staged elective cholecystectomy and repair of the biliary-enteric fistula for the RGSI[9,10,16,17,39,42,51,53,57,61,76,77]. One of these seven patients had a Cholecystostomy with their enterolithotomy[61]. There was no mortality in this group (Table 1).
Other methods to relieve the obstruction were occasionally used. In one patient a stone impacted at the pylorus was dealt with using endoscopic YAG laser lithotripsy accessing the stone by gastroscopylogie[22]. Four patients had small bowel resection with one death, giving a mortality of 25% (Table 1).
Only 17 patients had single stage surgery and one of them died giving a mortality rate of 11.7% (Table 2).
| Treatment | n | % | Mortality | % |
| Enterolithotomy/resection plus cholecystectomy with biliary-enteric fistula repair | 14 | 82.3 | 2 | 11.7 |
| Cholecystostomy and repair of biliary enteric fistula | 2 | 11.7 | 0 | |
| Right hemi-colectomy and cholecystectomy | 1 | 5.8 | 0 |
Eight patients were treated conservatively with a 25% mortality rate (Table 1). Pybus[88] and Foss[91] each described a person with RGSI not operated on who died and whose RGSI was diagnosed at post-mortem. A conservative approach led to spontaneous passage of the obstructing stone in four cases[18,92]. Rectal impaction of stone necessitated manual evacuation of stone in two patients[89,90].
The mean age of patients in the group who received enterolithotomy alone (data available for 62/73) was 70.5 years (SD 10.5, 47-95 years). The average age of patients in the single stage surgery group (data available for 12/17) was 65 years (SD 13.8, 38-88 years). The youngest patient to have RGSI was 38 years of age, had Crohn’s disease, and was treated with right hemi-colectomy and definitive single stage surgery. The oldest patient, 95 years of age, was treated with enterolithotomy and survived.
Data on postoperative morbidity was reported for 36 patients (Table 3). Wound related complication in terms of abscess and wound dehiscence were reported in 8 patients[2,16,24,34,36,40,49,51,64,77,78,83]. Haq[60] reported on a suture line breakdown after a closure of enterolithotomy that was managed conservatively leading to enterocutaneous fistula. McGreevy[38] also reported an enterocutaneous fistula after enterolithotomy for RGSI which was treated with conservative management.
| Morbidity | Enterolithotomyn = 28 | Single stage definitive surgeryn = 8 |
| No complications | 10 | 5 |
| Wound related-infection, dehiscence | 7 | 1 |
| Anastomosis related, including leak, fistula, intra-abdominal abscess | 2 | 1 |
| Other medical complications, sepsis, MI, pneumonia, renal failure | 9 | 1 |
Four case reports also mentioned a recurrent episode of GSI after second enterolithotomy[9,16,73,75].
In recent years there has been an improvement in surgical techniques and perioperative care and therefore a subset analysis of treatment outcomes over the last 25 years (1990-2015) was performed.
Thirty published cases of RGSI were found. Twenty one patients (70%) were treated with enterolithotomy with one death (mortality rate 4.8%). This compares with 11 deaths in 52 patients in the previous 77 years for enterolithotomy giving a 21.2% mortality rate (1912 -1989).
Nine patients had single stage surgery (30%) between 1990 and 2015, with two postoperative deaths giving a mortality rate of 22.2%. This compares with no deaths in 8 patients having single stage surgery in the previous 77 years (1912-1989) giving a mortality rate of 0%.
With regard to morbidity in the last 25 years, one patient in the single stage group had an intra-abdominal abscess and five patients in the enterolithotomy group had complications related to wound infection (two), evisceration (one), C.diff infection (one) and respiratory failure (one).
The literature reports an estimated risk of RGSI of 5%-8%[10-12,74]. However reporting of RGSI is probably underestimated because the figures are based on published case reports or series.
The management of RGSI presents a dilemma for the surgeon. Should one only deal with the presenting obstruction once more, in which case an enterolithotomy will suffice, or should one now also deal with the cause of the recurrence in which case additional cholecystectomy and repair of biliary-enteric fistula will be needed. We sought to review existing literature that would help clinicians choose appropriate treatment strategies when faced with RGSI.
In our review RGSI mainly occurred in patients who had their primary GSI treated with enterolithotomy (86.7%). However two patients who had RGSI had single stage surgery including biliary-enteric fistula repair at the initial episode[5]. The latter suggests that recurrence can be due to pre-existing stones in the bowel that have been missed. Identification of multiple stones at the outset is therefore likely to be helpful. While a pre operative CT scan may help, careful per operative manual searching for additional stones is crucial. The authors have personal experience with a patient who had two episodes of recurrent Gall Stone Ileus having been noted to have visible stones within the gall bladder on the CT scan at the time of initial and second presentation[16].
With regard to per operative searching for additional stones, the shape of the index stone may be a useful indicator. The presence of a faceted or a cylindrical stone at the time of first surgery suggests presence of multiple stones[10]. Most of the articles in our review did not comment on the shape of the stone but of the 36 articles that did, 83.3% of the stones were faceted. This suggests that a search for additional stones may be required more often than not, and that the search will be productive.
Treatment of RGSI is usually surgery, though our review found eight cases that had been dealt with conservatively. The mortality in these latter cases was very high (25%) and therefore should be avoided unless severe co-morbidities prohibit surgical intervention.
The surgical options include enterolithotomy alone with removal of the stone thus relieving the obstruction or an enterolithotomy with a definitive operation involving cholecystectomy and repair of the biliary-enteric fistula in order to prevent future RGSI.
Enterolithotomy alone is seen as technically less demanding than single stage surgery. The increased complexity of the latter procedure theoretically carries a higher operative risk. In addition, elderly patients with multiple medical co-morbidities may present a greater physiological risk and this has to be factored into the management of RGSI.
In our review of RGSI cases comparing the recent 25 years to the preceding 77 years, the operative mortality for single stage surgery was 22.2% (1990-2015) compared to 0% (1912-1989). This is despite advanced in surgical techniques and perioperative care. However these results must be interpreted with caution as this is based on published cases only and relatively small numbers of patients.
Of the cases treated with enterolithotomy the mortality rate for 1912-1989 was 21.2% compared to a rate of 4.8% for 1990-2015. The latter concurs with the mortality rate of 5% reported in 2013 by Halabi et al[93] from their analysis of the Project Nationwide inpatient sample (NIS) database of just over 2000 cases.
The mortality rate of the whole cohort over the last 100 years was lower for single stage surgery in comparison to enterolithotomy despite the procedure being technically more demanding (11.7% vs 16.4%). If age is used as a surrogate marker for physiological fitness then we can perhaps assume that patients undergoing single stage surgery were not only younger but also fitter. However the number of patients having single stage definitive surgery was small and data on age was not available for all patients therefore caution must be taken in the interpretation of these results.
A two-stage strategy with initial enterolithotomy followed by an elective cholecystectomy and biliary-enteric fistula repair had a better outcome with 0% mortality in the seven patients[10,17,39,51,55,59,83], however this represents less than 10% of the cases and probably represents a selection bias in patients fit enough to consider an elective second surgery. However this option should also be considered in the management of RGSI.
The mortality rates from enterolithotomy alone have reduced in the last 25 years and there is a risk, albeit low, of further recurrence. We recommend it as an appropriate choice for the management of RGSI especially for the non hepato-biliary surgeon who has to deal with an emergency obstruction caused by RGSI.
To deal with the problem of possible recurrence Single stage definitive surgery, despite being more technically demanding, may be worth considering but mortality rates remain high. This approach may be appropriate in younger patients who pose a lower risk. This concurs with recommendation from other authors who have reviewed the outcome of primary GSI.
With improvement of surgical techniques and perioperative care a delayed two-stage treatment approach may provide the best results in selected cases.
The authors wish to acknowledge the contribution of Christian Körner of University Hospital Giessen and Marburg, Marta Kankova and Sarah Braungart of York Teaching Hospital for help with translation of the Non- English articles.
Gallstones can often migrate to the intestinal tract and cause obstruction, called gallstone ileus (GSI). This migration of gallstones is a consequence of an inflamed gallbladder fistulating into the GI tract. The common operation to treat GSI is an enterolithotomy. Enterolithotomy deals with intestinal obstruction alone but risks have recurrence of gallstone ileus (RGSI). Various estimates put the incidence of gallstone ileus to be 5%-8%. A definitive surgery to prevent recurrence compromises of enterolithotomy and repair of the biliary fistula and cholecystectomy, this is a technically more demanding and prolonged operation with significant risks. The mortality from enterolithotomy has been quoted from 11%-18% in various studies. In acute setting the surgeon is faced with the dilemma of trying to balance between the risks of the operation compared to risk of recurrence of symptoms. This review will consolidate current evidence and help in choosing appropriate treatment in acute settings.
The review collates evidence towards management of RGSI. This condition is not encountered often in clinical practice and can present management dilemma as treatment options vary. This review will assist clinicians in their decision making process.
GSI: Gallstone ileus, intestinal obstruction caused by gallstone passing into the intestinal lumen; RGSI: Recurrent gallstone ileus is recurrence of intestinal obstruction due to a second gallstone. This gallstone could have passed from the gallbladder or due to a missed stone at the initial operation; Enterolithotomy: Removal of gallstone from bowel through an incision to the bowel wall; Single stage surgery: In the article, refers to enterolithotomy combined with removal of gallbladder (cholecystectomy) and repair of the biliary enteric fistula; Two stage surgery: Enterolithotomy followed by cholecystectomy and biliary enteric fistula at a later date.
The review content is innovative and concentrates on a rare but hard-to-deal emergence disease. The authors summarized the characteristics and treatment strategies of RGSI by reviewing case reports of this disease, which are valuable and has guiding significance in clinical practice.
P- Reviewer: Fu W, Nakayama Y S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Martin F. Intestinal obstruction due to gall-stones: with report of three successful cases. Ann Surg. 1912;55:725-743. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Syme RG. Management of gallstone ileus. Can J Surg. 1989;32:61-64. [PubMed] [Cited in This Article: ] |
| 3. | Fitzgerald JE, Fitzgerald LA, Maxwell-Armstrong CA, Brooks AJ. Recurrent gallstone ileus: time to change our surgery? J Dig Dis. 2009;10:149-151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Räf L, Spangen L. Gallstone ileus. Acta Chir Scand. 1971;137:665-675. [PubMed] [Cited in This Article: ] |
| 5. | Rodríguez-Sanjuán JC, Casado F, Fernández MJ, Morales DJ, Naranjo A. Cholecystectomy and fistula closure versus enterolithotomy alone in gallstone ileus. Br J Surg. 1997;84:634-637. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 82] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Piedad OH, Wels PB. Spontaneous internal biliary fistula, obstructive and nonobstructive types: twenty-year review of 55 cases. Ann Surg. 1972;175:75-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 46] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Clavien PA, Richon J, Burgan S, Rohner A. Gallstone ileus. Br J Surg. 1990;77:737-742. [PubMed] [Cited in This Article: ] |
| 8. | Webb LH, Ott MM, Gunter OL. Once bitten, twice incised: recurrent gallstone ileus. Am J Surg. 2010;200:e72-e74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Vagefi PA, Ferguson CM, Hall JF. Recurrent gallstone ileus: third time is the charm. Arch Surg. 2008;143:1118-1120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Buetow GW, Glaubitz JP, Crampton RS. Recurrent gallstone ileus. Surgery. 1963;54:716-724. [PubMed] [Cited in This Article: ] |
| 11. | Doogue MP, Choong CK, Frizelle FA. Recurrent gallstone ileus: underestimated. Aust N Z J Surg. 1998;68:755-756. [PubMed] [Cited in This Article: ] |
| 12. | Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg. 1994;60:441-446. [PubMed] [Cited in This Article: ] |
| 13. | Muthukumarasamy G, Venkata SP, Shaikh IA, Somani BK, Ravindran R. Gallstone ileus: surgical strategies and clinical outcome. J Dig Dis. 2008;9:156-161. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Abou-Saif A, Al-Kawas FH. Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol. 2002;97:249-254. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 188] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 15. | Ayantunde AA, Agrawal A. Gallstone ileus: diagnosis and management. World J Surg. 2007;31:1292-1297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 132] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 16. | Hussain Z, Ahmed MS, Alexander DJ, Miller GV, Chintapatla S. Recurrent recurrent gallstone ileus. Ann R Coll Surg Engl. 2010;92:W4-W6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Rogers FA, Carter R. Recurrent gallstone ileus. Am J Surg. 1958;96:379-386. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Büttner D. [Recurrent gallstone ileus]. Langenbecks Arch Chir. 1969;324:225-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Cooperman AM, Dickson ER, ReMine WH. Changing concepts in the surgical treatment of gallstone ileus: a review of 15 cases with emphasis on diagnosis and treatment. Ann Surg. 1968;167:377-383. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 61] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Kirkland KC, Croce EJ. Gallstone intestinal obstruction. A review of the literature and presentation of 12 cases, including 3 recurrences. JAMA. 1961;176:494-497. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Vaughan-Shaw PG, Talwar A. Gallstone ileus and fatal gallstone coleus: the importance of the second stone. BMJ Case Rep. 2013;2013:pii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Goldstein EB, Savel RH, Pachter HL, Cohen J, Shamamian P. Successful treatment of Bouveret syndrome using holmium: YAG laser lithotripsy. Am Surg. 2005;71:882-885. [PubMed] [Cited in This Article: ] |
| 23. | Wagner A. Iileus Durch Gallensteine. Deutsche Zeitschrf Chir. 1914;130:353-388. [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Kammerer F. Transactions of the New York Surgical Society: Stated Meeting, Held at the New York Academy of Medicine. Ann Surg. 1914;61:242. [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 25. | Hille R. Zweifachcr Gaflenstein Iieus. Miincben med Hcbnscbr. 1925;72:597-598 Available from: http://www.americanjournalofsurgery.com/article/0002-9610(58)90929-2/references. [Cited in This Article: ] |
| 26. | Turner GG. Intestinal Obstruction from Gall-stone: “Gall-stone Ileus.". Postgrad Med J. 1927;2:65-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Haas W. Demonstrationen-Vereinigung Münchener Chirurgen. Zentrabl Chir. 1927;54:2775 Available from: http://www.americanjournalofsurgery.com/article/0002-9610(58)90929-2/references. [Cited in This Article: ] |
| 28. | Wohlauer W. Zur Frage Des Gallensteinileus Arch Klin Chir 1929; 155: 167. Available from: http://www.americanjournalofsurgery.com/article/0002-9610(58)90929-2/references. [Cited in This Article: ] |
| 29. | Douglas J. Transactions of the New York Surgical Society-Stated Meeting January 27, 1932. Ann Surg. 1932;96:107-117. [PubMed] [Cited in This Article: ] |
| 30. | Mast WH. Recurrent Intestinal Obstruction Due to Gallstone. Am J Surg. 1936;32:516-518. [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 31. | Wakeley CPG, Willway FW. Intestinal Obstruction by Gall‐Stones. British J Surg. 1935;23:377-394. [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Schwarke R. Uber Zweimaligen Gallenstein-Ileus. Zentralblf Chir (Sept.3). 1938;65:1980-1985. [Cited in This Article: ] |
| 33. | Wakefield EG VP, Walters W. Intestinal Obstruction Caused by Gallstones Surgery 1939; 5: 670-673. Available from: http://www.surgjournal.com/article/S0039-6060(39)90378-8/abstract. [Cited in This Article: ] |
| 34. | Hinchey PR. Gallstone Ileus. Arch Surg. 1943;46:9-26. [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 35. | Hand BH, Gilmore WE. Gallstone Ileus: Recurrence in One Case. Am J Surg. 1943;59:72-78. [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 36. | Lee M. Intestinal Obstruction by Gall-stones. Br Med J. 1945;1:555-556. [PubMed] [Cited in This Article: ] |
| 37. | Vin zant LE, Hibbard JS. Recurrent ileus due to gallstones. J Kans Med Soc. 1949;50:17-19. [PubMed] [Cited in This Article: ] |
| 38. | McGeevy JV, McGeevy E. J. Recurrent Gallstone Ileus. South Dakota Journal Med Pharm. 1950;63 Available from: http://www.surgjournal.com/article/0039-6060(63)90218-6/references. [Cited in This Article: ] |
| 39. | Milch E, Mendez Jr F, Murphy H. Recurrent Gallstone Small Bowel Obstruction. Arch Surg. 1952;64:847. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 9] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 40. | Noskin EA, Tannenbaum WJ. Recurrent gallstone ileus; a case report. Surgery. 1952;31:599-601. [PubMed] [Cited in This Article: ] |
| 41. | Macfarlane J. Recurrent Gall-Stone Ileus. Brit Med J. 1953;2:544-545. [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 42. | Shore S, Jacob HH, Cannon JA. Intestinal Obstruction Resulting from Biliary Calculi (Gallstone Ileus). Arch surg. 1953;66:301. [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 43. | Schulte F. [Recurrent gallstone ileus]. Zentralbl Chir. 1954;79:2069-2071. [PubMed] [Cited in This Article: ] |
| 44. | Von Lutzki A. [Ileus and recurrent ileus due to gallstones]. Zentralbl Chir. 1955;80:1503-1513. [PubMed] [Cited in This Article: ] |
| 45. | Paschold K. [Clinical aspects of gallstone ileus and its recurrence]. Zentralbl Chir. 1956;81:2284-2290. [PubMed] [Cited in This Article: ] |
| 46. | Wiley J, Henderson A. Acute Intestinal Obstruction Due to Gallstones; Seven Cases Reported, One Recurrent. West J Surg Obstet Gynecol. 1956;64:213. [Cited in This Article: ] |
| 47. | Brockis JG, Gilbert MC. Intestinal obstruction by gall-stones; a review of 179 cases. Br J Surg. 1957;44:461-466. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 35] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 48. | Collins CM. Surgery repeated for recurrent gallstone ileus; review of literature and report of case. J Fla Med Assoc. 1957;43:675-682. [PubMed] [Cited in This Article: ] |
| 49. | Foley TJ, Selzer J. Gallstone ileus; seven cases with two recurrences. Wis Med J. 1958;57:253-256. [PubMed] [Cited in This Article: ] |
| 50. | Fiddian R. Gall-Stone Ileus Recurrences and Multiple Stones. Postgrad Med J. 1959;35:673-676. [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 51. | Ratner IA. Recurrent gallstone ileus; report of a case. J Maine Med Assoc. 1959;50:170-171. [PubMed] [Cited in This Article: ] |
| 52. | Logie JW, Bishop HM, Bullington DC, Cheek GW, Crabtree H, Fish JC, Lillie RH, MaCris JA, Middleton EE, Miller EB. Chronic Benign Penetrating Lesions of the Gallbladder. Ann Surg. 1961;154:121. [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 53. | Pera Gimenez C. [Biliary ileus (apropos of 23 cases)]. Lyon Chir. 1961;57:513-517. [PubMed] [Cited in This Article: ] |
| 54. | Thomas HS, Cherry JK, Averbook BD. Gallstone Ileus. JAMA. 1962;179:625-629. [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 17] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 55. | Malt RA. Experience with recurrent gallstone ileus applied to management of the first attack. Am J Surg. 1964;108:92-94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 56. | Giustra PE, Root JA, Killoran PJ. “Gallstone ileus”, times two. Am J Gastroenterol. 1977;67:613-615. [PubMed] [Cited in This Article: ] |
| 57. | Kvist E. Gallstone ileus. A retrospective study. Acta Chir Scand. 1979;145:101-103. [PubMed] [Cited in This Article: ] |
| 58. | Heuman R, Sjödahl R, Wetterfors J. Gallstone ileus: an analysis of 20 patients. World J Surg. 1980;4:595-598. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 32] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 59. | Levin B, Shapiro RA. Recurrent enteric gallstone obstruction. Gastrointest Radiol. 1980;5:151-153. [PubMed] [Cited in This Article: ] |
| 60. | Haq AU, Morris AH, Daintith H. Recurrent Gall-Stone Ileus. Brit J Radiol. 1981;54:1000-1001. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 61. | Svartholm E, Andrén-Sandberg A, Evander A, Järhult J, Thulin A. Diagnosis and treatment of gallstone ileus. Report of 83 cases. Acta Chir Scand. 1982;148:435-438. [PubMed] [Cited in This Article: ] |
| 62. | Deitz DM, Standage BA, Pinson CW, McConnell DB, Krippaehne WW. Improving the outcome in gallstone ileus. Am J Surg. 1986;151:572-576. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 67] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 63. | van Hillo M, van der Vliet JA, Wiggers T, Obertop H, Terpstra OT, Greep JM. Gallstone obstruction of the intestine: an analysis of ten patients and a review of the literature. Surgery. 1987;101:273-276. [PubMed] [Cited in This Article: ] |
| 64. | Sevilla Molina MP, Sánchez Blanco JM, Escribano Negueruela L, Gómez Rubio D, Recio Moyano G, Campoy Martínez P. [Biliary ileus: enterolithotomy only or radical surgery?]. Rev Esp Enferm Dig. 1992;81:407-410. [PubMed] [Cited in This Article: ] |
| 65. | Davies RJ, Sandrasagra FA, Joseph AE. Case report: ultrasound in the diagnosis of gallstone ileus. Clin Radiol. 1991;43:282-284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 66. | Bauermeister G, Aepler A. [Recurrent gallstone ileus--enterolithotomy alone or synchronous complete management]. Zentralbl Chir. 1998;123 Suppl 2:78-79. [PubMed] [Cited in This Article: ] |
| 67. | Hagger R, Sadek S, Singh K. Recurrent small bowel obstruction after laparoscopic surgery for gallstone ileus. Surg Endosc. 2003;17:1679. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 68. | Zissin R, Osadchy A, Klein E, Konikoff F. Consecutive instances of gallstone ileus due to obstruction first at the ileum and then at the duodenum complicating a gallbladder carcinoma: a case report. Emerg Radiol. 2006;12:108-110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 69. | Suárez Grau JM, Rubio Cháves C, Alarcón del Agua I, Casado Maestre MD, Tamayo López MJ, Palacios González C, López Bernal F, Martín Cartes JA, Bustos Jiménez M, Docobo Durántez F. [Gallstone ileus recurrence]. Rev Esp Enferm Dig. 2009;101:223-225. [PubMed] [Cited in This Article: ] |
| 70. | Farook MS, Harrison MJ. Selected Articles from the Journal Abdominal Surgery. American Society of Abdominal Surgeons, 2008/2009. Available from: http://www.abdominalsurg.org/journal.html. [Cited in This Article: ] |
| 71. | Santosh S, Riaz C. Recurrent Gallstone Ileus with Hostile Right Upper Quadrant: A Surgeon’s Dilemma. American Surgeon. 2010;76:E26-E27. [Cited in This Article: ] |
| 72. | Hayes N, Saha S. Recurrent gallstone ileus. Clin Med Res. 2012;10:236-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 73. | Jones R, Broman D, Hawkins R, Corless D. Twice recurrent gallstone ileus: a case report. J Med Case Rep. 2012;6:362. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 74. | Pronio A, Piroli S, Caporilli D, Ciamberlano B, Coluzzi M, Castellucci G, Vestri A, Pitasi F, Montesani C. Recurrent gallstone ileus: case report and literature review. G Chir. 2013;34:35-37. [PubMed] [Cited in This Article: ] |
| 75. | Aslam J, Patel P, Odogwu S. A case of recurrent gallstone ileus: the fate of the residual gallstone remains unknown. BMJ Case Rep. 2014;2014:pii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 76. | Gandamihardja TA, Kibria SM. Recurrent gallstone ileus: beware of the faceted stone. BMJ Case Rep. 2014;2014:pii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 77. | Welch J, Huizenga K, Roberts S. Recurrent Intestinal Obstruction Due to Gallstones. Proceedings of the Proceedings of the staff meetings Mayo Clinic, 1957: 628. . [Cited in This Article: ] |
| 78. | Claridge M. Recurrent gall-stone ileus. Br J Surg. 1961;49:134-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 79. | Herzog W. [On the postoperative gallstone ileus recurrence]. Chirurg. 1963;34:562-564. [PubMed] [Cited in This Article: ] |
| 80. | Warshaw AL, Bartlett MK. Choice of operation for gallstone intestinal obstruction. Ann Surg. 1966;164:1051-1055. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 48] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 81. | Ulreich S, Massi J. Recurrent gallstone ileus. AJR Am J Roentgenol. 1979;133:921-923. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 82. | Pangan JC, Estrada R, Rosales R. Cholecystoduodenocolic fistula with recurrent gallstone ileus. Arch Surg. 1984;119:1201-1203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 83. | Késmárky J. [Recurrent gallstone ileus]. Zentralbl Chir. 1986;111:50-52. [PubMed] [Cited in This Article: ] |
| 84. | La Meir M, Van Molhem Y. Recurrence of gallstone ileus with Crohn’s disease. Acta Chir Belg. 2001;101:35-37. [PubMed] [Cited in This Article: ] |
| 85. | Guttikonda S, Vaswani KK, Vitellas KM. Recurrent gallstone ileus: a case report. Emerg Radiol. 2002;9:110-112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 86. | Keogh C, Brown JA, Torreggiani WC, MacFarlane J, Halperin L. Recurrent gallstone ileus: case report. Can Assoc Radiol J. 2003;54:90-92. [PubMed] [Cited in This Article: ] |
| 87. | de Alencastro MC, Cardoso KT, Mendes CA, Boteon YL, de Carvalho RB, Fraga GP. Acute intestinal obstruction due to gallstone ileus. Rev Col Bras Cir. 2013;40:275-280. [PubMed] [Cited in This Article: ] |
| 88. | Pybus F. A Note on Two Cases of Gallstone Ileus. Lancet. 1922;200:812-813. [DOI] [Cited in This Article: ] |
| 89. | Cook PH, Watkins RP. Recurring Intestinal Obstruction by Gall Stone. New Engl J Med. 1932;207:462-465. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 90. | Van Ravenswaay A. Acute Intestinal Obstruction by Large Gallstone. Am J Surg. 1932;16:56. [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 91. | Foss HL, Summers JD. Intestinal obstruction from gallstones. Ann Surg. 1942;115:721.b2-721735. [PubMed] [Cited in This Article: ] |
| 92. | Lehr P. [A case of recurrent ileus caused by cholelithiasis]. Z Gesamte Inn Med. 1956;11:415-418. [PubMed] [Cited in This Article: ] |
| 93. | Halabi WJ, Kang CY, Ketana N, Lafaro KJ, Nguyen VQ, Stamos MJ, Imagawa DK, Demirjian AN. Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg. 2014;259:329-335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 141] [Article Influence: 14.1] [Reference Citation Analysis (0)] |