- Chief of Neurosurgical Spine and Education, NYU Winthrop Hospital, Mineola, New York, USA
Correspondence Address:
Nancy E. Epstein
Chief of Neurosurgical Spine and Education, NYU Winthrop Hospital, Mineola, New York, USA
DOI:10.4103/sni.sni_101_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. Predominantly negative impact of diabetes on spinal surgery: A review and recommendation for better preoperative screening. 13-Jun-2017;8:107
How to cite this URL: Nancy E. Epstein. Predominantly negative impact of diabetes on spinal surgery: A review and recommendation for better preoperative screening. 13-Jun-2017;8:107. Available from: http://surgicalneurologyint.com/surgicalint-articles/predominantly-negative-impact-of-diabetes-on-spinal-surgery-a-review-and-recommendation-for-better-preoperative-screening/
Abstract
Background:For patients undergoing spine surgery, the literature attributes significant increased perioperative risks/adverse events (AE) complications, longer length of stay (LOS), and higher 30-day readmission/reoperation rates to those with diabetes. Diabetics are often divided into those with insulin dependent diabetes (IDDM), and non-insulin dependent diabetes (NIDD). However, other series also compare those with uncontrolled diabetes (UCDM) vs. those with controlled DM (CDM).
Methods:We found a marked variation in the size and quality of studies identified in PubMed regarding the impact of diabetes on spinal surgery (e.g., focusing on complications, AE, outcomes, morbidity, and mortality).
Results:Of the 197,461 lumbar fusions in one NIS (Nationwide Inpatient Sample 1988–2003), 11,000 (5.6%) diabetics (DM) had higher infection rates, transfusion rates, more pneumonias, higher in-hospital mortality rates, greater costs, and longer LOS than those undergoing similar procedures without DM. For 3726 ACS-NSQIP patients undergoing anterior cervical fusions, 270 NIDDM had more urinary tract infections and returns to the operating room; the 171 IDDM required more reoperations, 30 day readmission, and longer LOS (by 5 days) vs. 3285 non DM. Of the 5627 patients undergoing posterior cervical fusions (ACS-NSQIP), 2029 (36.1%) had AE directly related to DM. In another NSQUIP study of 51277 patients undergoing lumbar spine surgery, IDDM and NIDDM demonstrated longer LOS, plus IDDM showed more surgical AE and 30 day readmissions vs. those with no DM.
Conclusions:Patients with IDDM or NIDDM undergoing spine surgery exhibited more perioperative complications/AE/morbidity, longer LOS, and higher readmission/reoperation rates vs. non DM.
Keywords: Diabetes: spinal surgery, insulin dependent DM (IDDM), more adverse events, more complications, poorer outcomes: non-insulin dependent DM (NIDDM)
INTRODUCTION
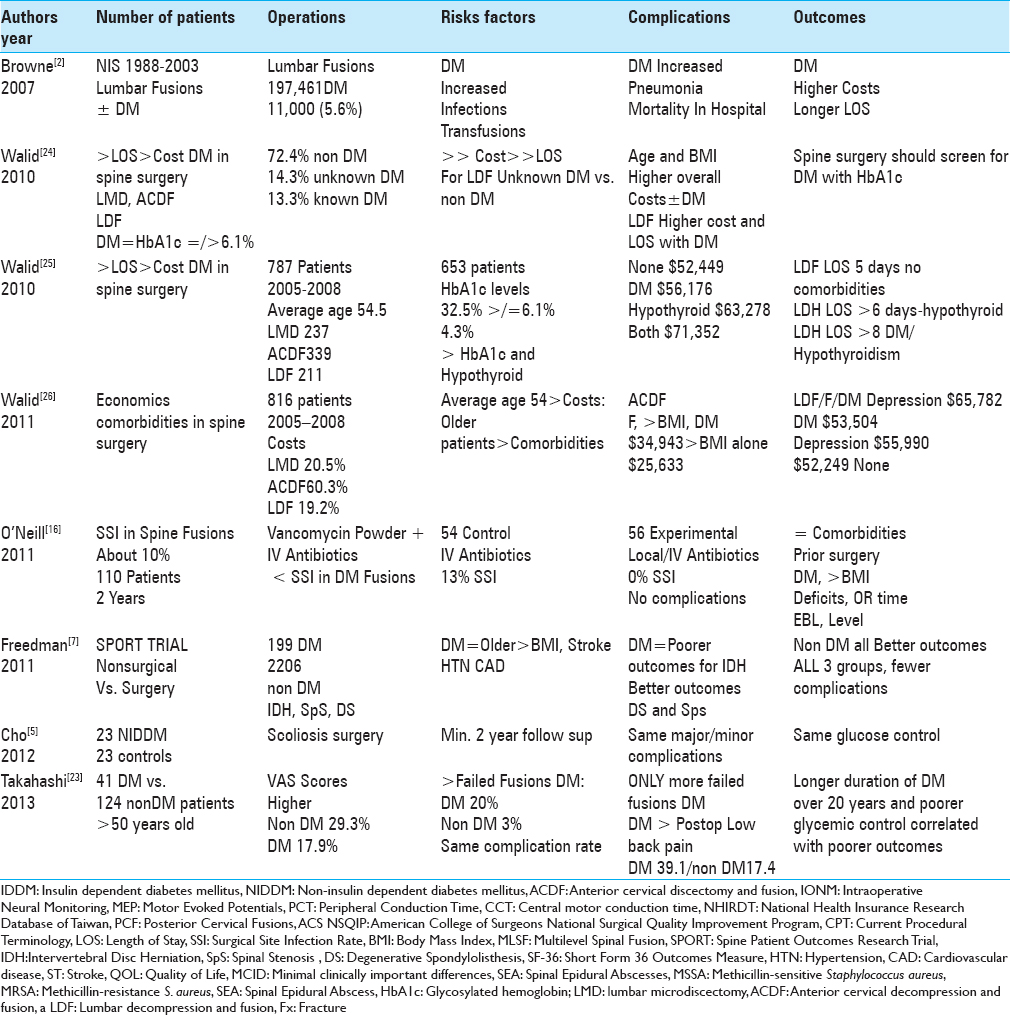
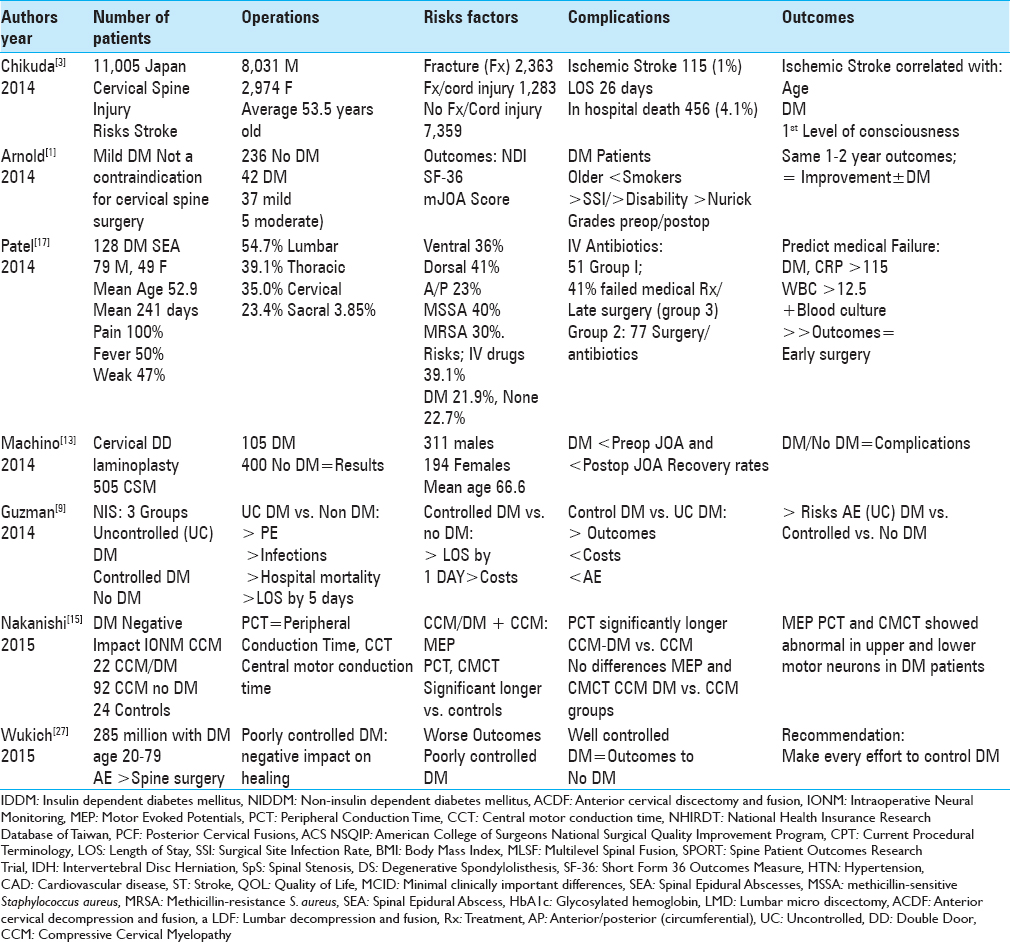
For patients undergoing spinal surgery, the literature attributes significantly increased morbidity, adverse events (AE), complications and even mortality to diabetes [Tables
In this study, we queried PubMed utilizing the following search engines; diabetes, spinal surgery, complications/adverse events (AE), outcomes, morbidity, and mortality. The 27 studies identified varied markedly in quality and design, ranging from small series to large national database analyses. In the Browne et al. (2007) report, that included an evaluation of 197,461 NIS (Nationwide Inpatient Sample 1988–2003) patients undergoing lumbar spine fusions, there were 11000 (5.6%) diabetics (based on HbA1c testing); the diabetic patients exhibited higher rates of infection, pneumonia, in-hospital mortality, hospital costs, required more transfusions, and had longer lengths of stay (LOS) vs. non-DM patients [
DIABETES: A MAJOR COMORBIDITY FOR PATIENTS UNDERGOING SPINAL SURGERY
For patients undergoing spinal surgery, Epstein (2012) noted that diabetes (DM) was associated with a higher risk of infection, osteoporosis, and pseudarthrosis, as well as other major medical risk factors.[
VARIABLE IMPACT OF DIABETES ON CERVICAL SPINE SURGERY
Although one study documented the absence of a negative impact of DM on AE events associated with decompressive cervical spine surgery, three studies did show increased DM-related perioperative morbidity. In the first study, Arnold et al. (2014), evaluated 42 DM (37 mild/5 moderate) vs. 236 non DM: they found that DM had no negative impact on the results of decompressive cervical surgery for cervical spondylotic myelopathy (CSM) [
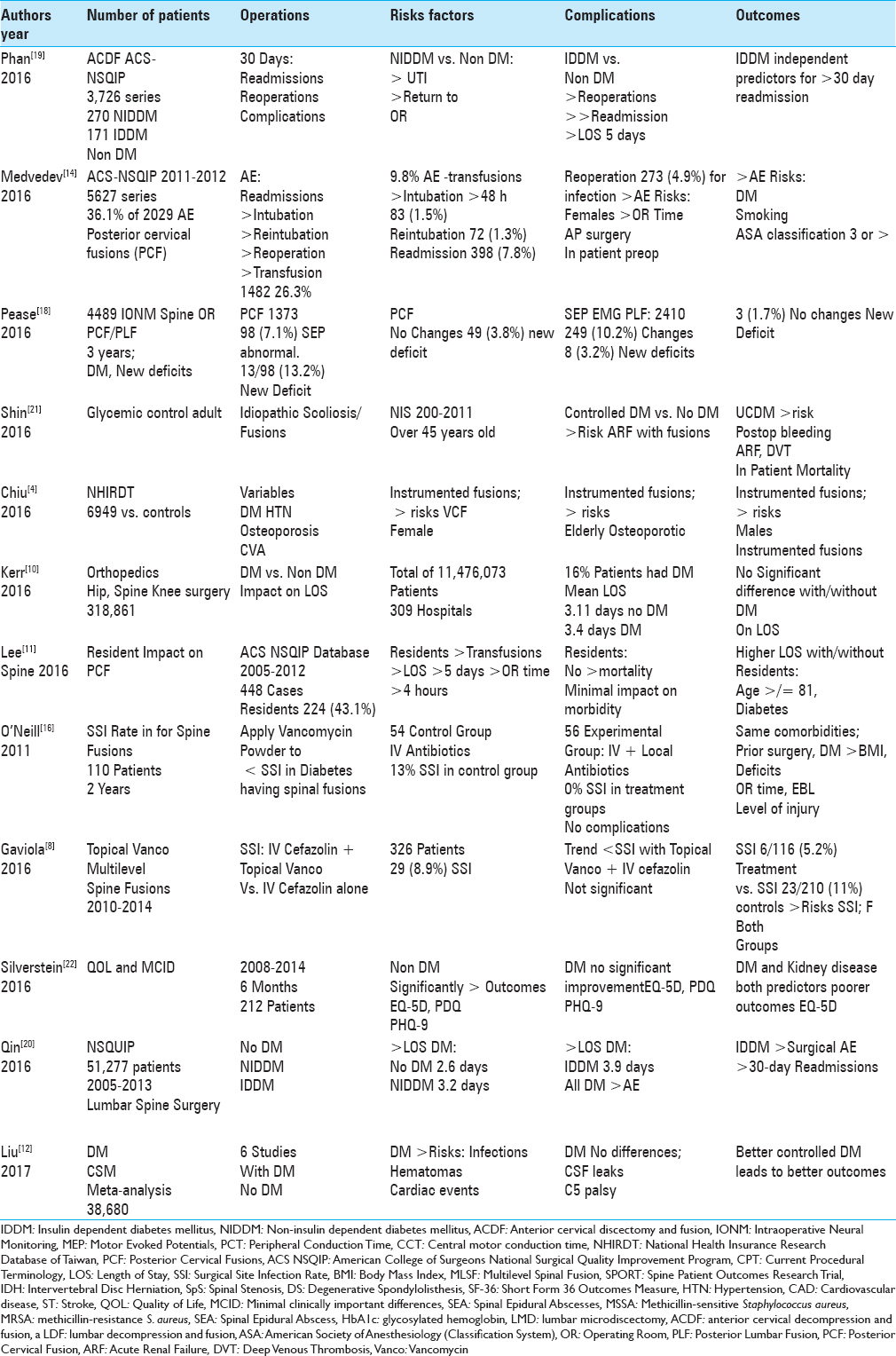
NEGATIVE IMPACT OF DIABETES ON ANTERIOR CERVICAL DISKECTOMY/FUSION
Out of 3726 patients undergoing ACDF obtained from an ACS NSQIP (American College of Surgeons-National Surgical Quality Improvement Program) database, Phan et al. (2016) showed that IDDM (171 patients) and NIDDM (270 patients) exhibited higher risks, complication rates, AE, and greater 30-day reoperation/readmission rates [
VARIABLE IMPACT OF DIABETES ON POSTERIOR CERVICAL SURGERY
DM had a variable impact on the frequency of AE and outcomes doe for posterior cervical surgery [e.g., including laminoplasty and posterior cervical fusion (PCF)]. Over 12 months following double door laminoplasty performed for CSM (mean 66.6 years of age), Machino (2014) showed comparable AE/outcomes for 105 DM vs. 400 non DM patients [
DIABETES NEGATIVE IMPACT ON INTRAOPERATIVE NEURAL MONITORING FOR SPINE SURGERY
DM had a negative impact on intraoperative neural monitoring (IONM) for patients undergoing decompressive cervical surgery for myelopathy (CCM) [Tables
DIABETES: VARIABLE IMPACT ON ADVERSE EVENTS/LENGTH OF STAY FOR ELECTIVE GENERAL ORTHOPEDIC PROCEDURES
Two studies demonstrated the variable impact of DM on AE/LOS/outcomes for general orthopedic procedures [Tables
The marked disparity in results for orthopedic procedures involving DM patients utilizing such large database analyses remains difficult to explain. One question is who was doing the surgery? When residents were involved, greater morbidity typically follows (e.g., greater LOS and more transfusions), a finding typically attributed to their inexpert technical/surgical skills. Here, better supervision by more senior surgeons/physicians may improve results. On the other hand, there may be great disparities in different settings (e.g., private practice vs. academia with residents) regarding how patients are selected for surgery. Some surgeons may choose to operate on patients irrespective of their comorbidities, whereas others may perform surgery without sufficient indications (e.g., unnecessary surgery). Another major consideration is whether the data entered into the various large databases (ACS-NSQIP, CPDDF, NIS) were correct, relevant, and appropriate for the problem under investigation. Certainly, these questionnaires may miss the critical factors that may be truly impacting outcomes.
DIABETES RESULTED IN GREATER MORBIDITY/MORTALITY AND POORER OUTCOMES WITH LUMBAR FUSIONS VS. THOSE WITHOUT DIABETES MELLITUS
Multiple studies documented increased complication/AE rates for DM patients undergoing lumbar fusions [Tables
VARIABLE IMPACT OF DIABETES ON SCOLIOSIS FUSION SURGERY
Two series, one very small, and another every large (NIS), demonstrated very different conclusions regarding the impact of DM vs. no DM on scoliosis surgery [Tables
DIABETES: A MAJOR RISK FACTOR FOR SPINAL EPIDURAL ABSCESS (SEA)
DM is a major risk factor for patients to develop SEA following spinal surgery, it could also contribute to the postoperative risk of SEA. When Patel et al. (2014) examined 128 consecutive bacterial SEA extending over an average of 3.85 disc levels, DM was a major risk factor (21.9%) along with intravenous (IV) drug abuse (39.1%) [
VANCOMYCIN POWDER WITH ROUTINE INTRAVENOUS ANTIBIOTICS DECREASED THE RISK OF SURGICAL SITE INFECTION FOLLOWING INSTRUMENTED FUSION
Ten percent of patients undergoing posterior spinal instrumented infections secondary to trauma typically develop surgical site infection (SSI: deep or superficial) (deep/superficial) [
DIABETES ALONE OR WITH OTHER MAJOR COMORBIDITIES INCREASED TOTAL HOSPITAL COSTS AND LENGTH OF STAY FOR SPINE SURGERY
For patients undergoing spine surgery, DM alone or combined with other major comorbidities, including hypothyroidism, elevated BMI, older age, and depression, increased total hospital costs, and LOS. When Walid et al. (2010) tested elevated glycosylated hemoglobin levels (HbA1c) >/=6.1) for patients undergoing lumbar microdiskectomy (LMD), ACDF, or lumbar decompression/fusion (LDF), they discovered 13.3% were known DM, 14.3% were unknown DM (e.g., prior to surgery), and 72.4% had no DM [
CONCLUSION
The vast majority of the larger series utilizing major U.S. patient databases, documented that diabetic patients (e.g., IDDM, NIDDM, CDM, UCDM) undergoing spine surgery exhibited more perioperative morbidity/AE/complications, longer LOS, higher 30-day readmission/reoperation rates, and increased mortality compared with non DM. Only a subset of smaller studies, too small to yield “significant findings,” demonstrated no negative impact of DM on the results of spinal surgery. Future routine preoperative screening for DM with HbA1c levels would likely be worthwhile (e.g., one series demonstrated 14.3% of patients were “unknown DM”), as this could facilitate better preoperative, intraoperative, and postoperative management.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arnold PM, Fehlings MG, Kopjar B, Yoon ST, Massicotte EM. Mild diabetes is not a contraindication for surgical decompression in cervical spondylotic myelopathy: Results of the AOSpine North America multicenter prospective study (CSM). Spine J. 2014. 14: 65-72
2. Browne JA, Cook C, Pietrobon R, Bethel MA, Richardson WJ. Diabetes and early postoperative outcomes following lumbar fusion. Spine (Phila Pa 1976). 2007. 32: 2214-9
3. Chikuda H, Ohya J, Horiguchi H, Takeshita K, Fushimi K, Tanaka S. Ischemic stroke after cervical spine injury: Analysis of 11,005 patients using the Japanese Diagnosis Procedure Combination database. Spine J. 2014. 14: 2275-80
4. Chiu YC, Tsai TT, Yang SC, Chen HS, Kao YH, Tu YK. Impact of Instrumented Spinal Fusion on the Development of Vertebral Compression Fracture. Medicine (Baltimore). 2016. 95: e3455-
5. Cho W, Lenke LG, Bridwell KH, Dorward IG, Shoda N, Baldus CR. Comparison of spinal deformity surgery in patients with non-insulin-dependent diabetes mellitus (NIDDM) versus controls. Spine (Phila Pa 1976). 2012. 37: E978-84
6. Epstein NE. How much medicine do spine surgeons need to know to better select and care for patients?. Surg Neurol Int. 2012. 3: S329-49
7. Freedman MK, Hilibrand AS, Blood EA, Zhao W, Albert TJ, Vaccaro AR. The impact of diabetes on the outcomes of surgical and nonsurgical treatment of patients in the spine patient outcomes research trial. Spine (Phila Pa 1976). 2011. 36: 290-307
8. Gaviola ML, McMillian WD, Ames SE, Endicott JA, Alston WK. A Retrospective Study on the Protective Effects of Topical Vancomycin in Patients Undergoing Multilevel Spinal Fusion. Pharmacotherapy. 2016. 36: 19-25
9. Guzman JZ, Skovrlj B, Shin J, Hecht AC, Qureshi SA, Iatridis JC. The impact of diabetes mellitus on patients undergoing degenerative cervical spine surgery. Spine (Phila Pa 1976). 2014. 39: 1656-65
10. Kerr D, Yadollahi M, Bautista HM, Chen X, Dong S, Guerrier SN. Use of a Publicly Available Database to Determine the Impact of Diabetes on Length of Hospital Stay for Elective Orthopedic Procedures in California. Popul Health Manag. 2016. 19: 439-44
11. Lee NJ, Kothari P, Kim C, Leven DM, Skovrlj B, Guzman JZ. The Impact of Resident Involvement in Elective Posterior Cervical Fusion. Spine (Phila Pa 1976). 2016. p.
12. Liu Y, Ban DX, Kan SL, Cao TW, Feng SQ. The Impact of Diabetes Mellitus on Patients Undergoing Cervical Spondylotic Myelopathy: A Meta-Analysis. Eur Neurol. 2017. 77: 105-12
13. Machino M, Yukawa Y, Ito K, Inoue T, Kobayakawa A, Matsumoto T. Impact of diabetes on the outcomes of cervical laminoplasty: A prospective cohort study of more than 500 patients with cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2014. 39: 220-7
14. Medvedev G, Wang C, Cyriac M, Amdur R, O’Brien J. Complications, Readmissions, and Reoperations in Posterior Cervical Fusion. Spine (Phila Pa 1976). 2016. 41: 1477-83
15. Nakanishi K, Tanaka N, Kamei N, Hiramatsu T, Ujigo S, Sumiyoshi N. Electrophysiological assessments of the motor pathway in diabetic patients with compressive cervical myelopathy. J Neurosurg Spine. 2015. 23: 707-14
16. O’Neill KR, Smith JG, Abtahi AM, Archer KR, Spengler DM, McGirt MJ. Reduced surgical site infections in patients undergoing posterior spinal stabilization of traumatic injuries using vancomycin powder. Spine J. 2011. 11: 641-6
17. Patel AR, Alton TB, Bransford RJ, Lee MJ, Bellabarba CB, Chapman JR. Spinal epidural abscesses: Risk factors, medical versus surgical management, a retrospective review of 128 cases. Spine J. 2014. 14: 326-30
18. Pease M, Gandhoke GS, Kaur J, Thirumala P, Balzer J, Crammond D. Predictive Value of Intraoperative Neurophysiological Monitoring During Spine Surgery: A Prospective Analysis of 4489 Consecutive Patients. Neurosurgery. 2016. 63: 192-3
19. Phan K, Kim JS, Lee N, Kothari P, Cho SK. Impact of Insulin Dependence on Perioperative Outcomes following Anterior Cervical Discectomy and Fusion (ACDF). Spine (Phila Pa 1976). 2016. p.
20. Qin C, Kim JY, Hsu WK. Impact of Insulin Dependence on Lumbar Surgery Outcomes: An NSQIP Analysis of 51,277 Patients. Spine (Phila Pa 1976). 2016. 41: E687-93
21. Shin JI, Phan K, Kothari P, Kim JS, Guzman JZ, Cho SK. Impact of Glycemic Control on Morbidity and Mortality in Adult Idiopathic Scoliosis Patients Undergoing Spinal Fusion. Clin Spine Surg. 2016. p.
22. Silverstein MP, Miller JA, Xiao R, Lubelski D, Benzel EC, Mroz TE. The impact of diabetes upon quality of life outcomes after lumbar decompression. Spine J. 2016. 16: 714-21
23. Takahashi S, Suzuki A, Toyoda H, Terai H, Dohzono S, Yamada K. Characteristics of diabetes associated with poor improvements in clinical outcomes after lumbar spine surgery. Spine (Phila Pa 1976). 2013. 38: 516-22
24. Walid MS, Newman BF, Yelverton JC, Nutter JP, Ajjan M, Robinson JS. Prevalence of previously unknown elevation of glycosylated hemoglobin in spine surgery patients and impact on length of stay and total cost. J Hosp Med. 2010. 5: E10-4
25. Walid MS, Zaytseva N. How does chronic endocrine disease affect cost in spine surgery?. World Neurosurg. 2010. 73: 578-81
26. Walid MS, Robinson JS. Economic impact of comorbidities in spine surgery. J Neurosurg Spine. 2011. 14: 318-21
27. Wukich DK. Diabetes and its negative impact on outcomes in orthopaedic surgery. World J Orthop. 2015. 6: 331-9